The morbidity and mortality associated with medication misadventure in Australia is well documented.1,2 A focus on the smooth transition from hospital to community-based general practice is an essential component to help reduce this public health problem.3-9
The guidelines set forth by the Australian Pharmaceutical Advisory Council (APAC) to address continuity of care in therapeutics recommend medication discharge planning and specific communication with patients and their general practitioners about medications.6 The model reflects hospital concerns that changes made to medication during hospitalisation are not maintained in the community, with relatively little focus on the roles and responsibilities of general practice.
In a previous study, we showed that compliance with the APAC Guidelines was poor, with the hospitals in our study directly notifying GPs of the admission of 22% of patients audited.3 The current study continues the use of the GP audit method, with the focus on action through quality improvement as advocated by the APAC Guidelines.3,6,10
Our aim was to evaluate adherence to an agreed minimum dataset for patient medication information exchange between hospitals and GPs.
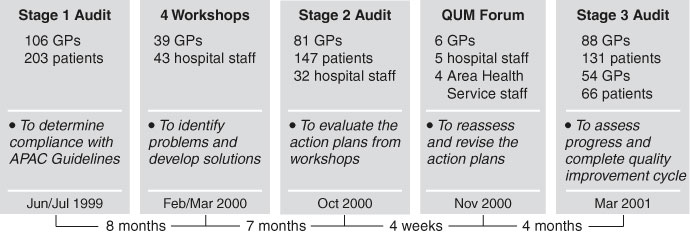
The project was carried out in 2000–2001 (Box 1) within the South East Area Health Service (SEAHS), Sydney. The SEAHS includes 11 public hospitals responsible for 155 000 patient admissions each year. Action plans were determined at workshops conducted at four major hospitals. Key stakeholders agreed on a minimum dataset (Box 2), actions required and who would conduct the tasks. Actions were to be implemented after the workshops.
No significant change occurred from Stage 1 to Stage 2 regarding the direct notification of GPs by hospitals at the time of the patient's admission (Box 3). For 15% (22/146) of patients, GPs were phoned or faxed by the hospital on admission regarding contact details of specialists or registrars managing the patient.
There was a significant increase in the percentage of patients for whom GPs provided medication information to the hospital (χ2 = 5.1; df = 1; P < 0.05). Seventy-four per cent (23/31) of GPs who were directly notified of their patients' admissions provided medication information, compared with 42% (41/97) of those not notified.
There was a significant increase in the percentage of patients for whom GPs received a faxed discharge summary (χ2 = 44.6; df = 1; P < 0.001). Eighty per cent (114/143) of patients audited during Stage 2 were seen by their GP within a week of discharge from hospital. For 31% (44/143) of patients, GPs reported receiving the new discharge referral form that included reasons for changing medications.
GPs reported that they had given their business card to 29% (42/147) of patients audited.
At Stage 3, there was no change in the notification of admission directly to GPs (Box 3). However, the improvement shown in Stage 2 in faxing of discharge summaries directly to GP surgeries was maintained. The proportion of GPs providing medication information to the hospital was maintained in both the original sample of GPs and the comparison sample of GPs during Stage 3.
By focusing on a "shared responsibility" model, our QUM program brought the issue of continuity of care in therapeutics into focus for public hospitals across a large urban Area Health Service and its associated Divisions of General Practice. GPs were a key component of the quality improvement process, by providing the monitoring data and participating in the planning and review process alongside hospital clinicians and administrators.
The program confirmed that system change is slow: overall only two measures (hospitals faxing discharge summaries to GPs and GPs supplying medication information to hospitals) improved significantly over the study period. On the other hand, when it did occur, system change appeared to be maintained. The inclusion of the comparison sample gives some control for participation bias.
A key stage in the quality improvement cycle is reviewing action plans with evidence of what has actually been achieved. The wisdom of working on change in small steps10 was clear. For example, there was no uniform assignment of responsibility for notifying GPs about patient admission. GP liaison officers have now been appointed to the SEAHS's major hospitals. This might facilitate notification of GPs about patient admission and rationales for changes made to patients' medications during hospitalisation.
For the GP surveys, response rates were satisfactory for a quality improvement study. Nevertheless, the overall sample size was small, and may not be generalisable. The number of hospital respondents selected was also small.
The APAC Guidelines call for local action through quality improvement. We found it useful to develop a minimum dataset for monitoring, but adherence remained poor. GP Divisions may need to be involved alongside hospitals in the quality improvement cycle if system change to improve continuity is even to commence.
2: Minimum dataset derived from recommendations at workshops in Stage 1
GP surveys of patients seen following discharge
GPs directly notified of admission by hospital.
Medication information provided by GPs to hospital.
GPs receive discharge summary at surgery by fax.
GPs receive discharge referral form including reasons for changing medications.
GPs report giving business card to patients.
GPs have a dedicated fax line.
Hospital survey
Hospitals have an updated GP directory.
3: Changes in the minimum dataset for patients following recent discharge from hospital
General practitioner surveys |
Stage 1* (95% CI) [n/N] |
Stage 2 (95% CI) [n/N] |
Stage 3 (95% CI) [n/N] |
Stage 3C† (95% CI) [n/N] |
|||||||
GP directly notified of admission by hospital |
22% (16%–28%) [44/203] |
23% (16%–30%) [32/141] |
24% (17%–31%) [31/130] |
22% (12%–32%) [14/65] |
|||||||
Medication information provided by GPs to hospitals |
38% (31%–45%) [78/203] |
51% (43%–60%) [69/134] |
52% (43%–61%) [65/124] |
55% (43%–67%) [35/64] |
|||||||
GP receiving discharge summary at surgery by fax |
2% (0.1%–3.9%) [4/203] |
26% (19%–33%) [38/145] |
27% (19%–35%) [35/128] |
32% (20%–44%) [19/60] |
|||||||
GPs receiving discharge referral form including reasons for changing medications |
na |
31% (23%–39%) [44/143] |
29% (21%–37%) [37/128] |
37% (25%–49%) [23/62] |
|||||||
GPs reported giving business cards to patients |
na |
29% (22%–36%) [42/147] |
39% (31%–47%) [51/131] |
27% (16%–38%) [18/66] |
|||||||
GPs with dedicated fax line |
na |
91% (85%–97%) [71/78] |
92% (86%–98%) [80/87] |
85% (75%–96%) [44/52] |
|||||||
* Stage 1 results have been previously published. † Comparison sample of GPs. n = number of positive responses. N = total number in analysis. na = item not available in Stage 1. |
|||||||||||
- Andrea Mant1
- Nicole L Cockayne2
- Linda Kehoe3
- Karen I Kaye4
- Wendy C Rotem5
- 1 Quality Use of Medicines Services, South East Sydney Area Health Service, Sydney, NSW.
- 2 Total Research, Sydney, NSW.
- 3 NSW Therapeutic Assessment Group Inc., Sydney, NSW.
- 4 Health Services Project Management, Sydney, NSW.
In addition to the authors the Area-GP QUM Continuity Project Team included Gary Franks, Sylvia Jacobson, Lynette Lee, Errol Kaplan, Phillip Lye, David Newman, Ven Tan, and RO Day.
None declared.
- 1. Wilson RM, Runciman WB, Gibberd RW, et al. The Quality in Australian Health Care Study. Med J Aust 1995; 163: 458-471. <eMJA pdf>
- 2. Roughead EE, Gilbert AL, Primrose JG, Sansom LN. Drug-related hospital admissions: a review of Australian studies published 1988–1996. Med J Aust 1998; 168: 405-408.
- 3. Mant A, Rotem WC, Kehoe L, Kaye KI. Compliance with guidelines for continuity of care in therapeutics from hospital to community. Med J Aust 2001; 174: 277-280.
- 4. Green CF, Mottram DR, Pirmohamed M, et al. Communication regarding adverse drug reactions between secondary and primary care: a postal questionnaire survey of general practitioners. J Clin Pharm Ther 1999; 24: 133-139.
- 5. Bolton P, Mira M, Kennedy P, Moses Lahra M. The quality of communication between hospitals and general practitioners: an assessment. J Qual Clin Pract 1998; 18: 241-247.
- 6. Australian Pharmaceutical Advisory Council. National guidelines to achieve the continuum of quality use of medicines between hospital and community. Canberra: Commonwealth of Australia, 1998.
- 7. Sturmberg JP. Continuity of care revisited [letter]. Fam Pract 2001; 18: 461-462.
- 8. Sexton J, Brown A. Problems with medicines following hospital discharge: not always the patient's fault? J Soc Admin Pharm 1999; 16: 199-207.
- 9. Balla JI, Jamieson WE. Improving the continuity of care between general practitioners and public hospitals. Med J Aust 1994; 161: 656-659.
- 10. Leape LL, Kabcenell AI, Gandhi TK, et al. Reducing adverse drug events: lessons from a breakthrough series collaborative. J Qual Improv 2000; 26: 321-331.





Abstract
Objective: To evaluate adherence to an agreed minimum dataset for patient medication information exchange between hospitals and general practitioners.
Design: Quasi pre–post design with a supplementary post-program comparison group; sequential descriptive surveys of patients following recent discharge from public hospitals; opinion questionnaire for key hospital informants; stakeholder forum to review data and Quality Use of Medicines (QUM) action plans between pre- and post-program surveys.
Participants and setting: GPs and hospitals from the South East Area Health Service, Sydney. During 2000–2001, 81/124 GPs (65%) returned 147 patient questionnaires in initial follow-up; 88/119 GPs (74%) returned 131 questionnaires in final follow-up; a supplementary group of 54/120 GPs (45%) returned 66 questionnaires; 32/45 (71%) of nominated key informants responded to the hospital survey.
Results: Direct notification of GPs by hospitals of their patient's admission was unchanged from the initial level of 22%. The proportion of GPs providing medication information to the hospital increased from 38% to 51% at Stage 2 (P < 0.05) and remained at 52% at Stage 3. The proportion of GPs receiving discharge summaries directly (initially 2%) increased to 26% at Stage 2 (P < 0.001) and remained at 27% at Stage 3.
Conclusions: System change is slow to occur, but changes that are implemented are maintained. The stakeholder forum suggested that a specific person should be responsible for GP liaison.