Once the support component of the MEO role becomes known, concern about a particular JMO may be raised by the supervising registrars or consultants, the nursing staff, allied health staff, other JMOs, and, at times, a JMO contacts the MEO directly. There is often a sense of relief that there is someone in the system who can deal with these concerns. Most alerts are prompted by concerns about clinical performance. However, pastoral concerns are sometimes implicated (Box 1).
Following an alert, a wider context needs to be established. There is a need not only to check the information, but also to look beyond the obvious (eg, a seeming inability of the JMO to prioritise may disguise an avoidance issue and a host of other factors). Fact finding may involve talking with other members of the unit, or being aware of a particular unit's history with JMOs, and/or the "track record" of the person who initiated the alert, and of the JMO concerned. Of course, there is a need for discretion, whether enquiries are made directly or at a more casual level. Usually, an informal interview is conducted with the JMO to detail the issues raised and note any additional pertinent information. Once the facts are established and a picture begins to emerge, the underlying issues can be more clearly identified, and then decisions can be made and actions taken. The key drivers of JMO distress that have emerged at NWAHS are listed in Box 2.
Stressors may be external (ie, to do with the outer environment), or internal (ie, to do with inner processes at a personal level). An example of an important external stressor that is crucial to a JMO's experience is the quality and continuity of registrar presence on a unit. For example, how organised is the registrar? Does the registrar involve the JMO in patient management decisions? How willing is the registrar to teach and extend the JMO? How willing is the registrar to assist and support the JMO during busy periods? And, finally, how available is the registrar when needed? In this regard, the lead-up to physicians' examinations is a particularly stressful time for JMOs.
Other external stressors of note include bullying and harassment, particularly the way in which nursing staff can undermine a JMO (or a student). Once covert, these issues are now beginning to be more openly discussed. Having a supportive medical administration, too, can make a big difference to JMOs' sense of wellbeing. This has been clearly documented by end-of-year intern surveys conducted at NWAHS in 1999 and 2000. Highlighted issues included perceived unfair rostering and leave allocation, general unhelpfulness and discourtesy, and bullying and harassment issues.
One of the internal stressors listed, professional ethics, has emerged from interviews and end-of-year surveys of JMOs. Issues related to the constant pressure for early — sometimes perceived as too-early — discharge of patients; how "not for resuscitation" orders are interpreted by nursing staff on some wards; and, more generally, the way patients are routinely treated by some health professionals. By the end of the year, some JMOs report disillusionment with a system which they perceive is forced to practise "conveyor belt" medicine. Given that many JMOs entered medicine for altruistic reasons, these ethical issues are a source of distress.
These assessments will influence decisions on how to tailor individual interventions to best manage each situation. Listed below are some of the strategies that have been implemented at NWAHS.
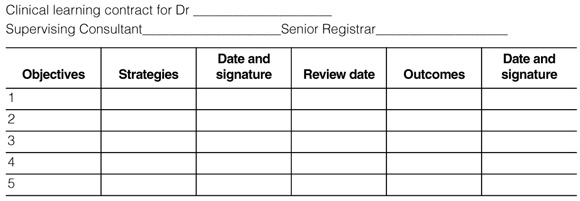
When a JMO's difficulties are related to personal performance, it is most important that this is identified within the first month of an attachment. This allows time for the problems to be discussed by all concerned, a plan of remediation to be constructed, and a performance review to take place before the final assessment. Those involved include the supervising consultant and unit registrar, together with the JMO, and, at times, the MEO or DCT acting in a facilitating and supportive role. The clinical learning contract forms the basis for this process and serves as a simple, documented record of the JMO's progress.
Some of the first-line counselling strategies are listed in Box 4. The first few relate to general skills that are available to most mature and reasonably sensitive people willing to spend time with another person in distress. The second group applies to people trained in counselling.
Integral to the whole process, and the real strength of MEOs, is their independence from medical power structures and from direct involvement in JMOs' evaluation. The MEO, however, should be able to "network" and access hospital and medical authorities. To this extent, the trust placed in MEOs by all concerned (junior doctors, registrars, senior clinicians, and administrators), and the need for confidentiality and discretion, are complex and crucial factors. Professional integrity on the part of the MEO is paramount.
1: What prompts an alert to the Medical Education Officer about a junior medical officer (JMO)?
Performance-related concerns
Problems with time management (eg, discharge summaries not completed in a timely manner or not adequate; working hours too long; difficulties prioritising).
Problems in situations when JMOs provide cover for medical and surgical emergencies, such as during change of shift (short calls).
Problems with clinical competence in a specific setting or situation.
Interpersonal problems (conflicts and difficulties relating to others).
Pastoral concerns
Observably high levels of anxiety and tension.
Inclined to "self put-down".
Crying episodes.
Clinical depression.
Problems with attitude (eg, perceived arrogant and patronising behaviour; short-tempered, impatient outbursts; or shirking a fair share of the workload).
2: Factors affecting stress levels in junior medical officers
External stressors
|
Internal stressors
|
4: First-line counselling strategies
Non-professional counselling
Listening, giving emotional support and clarifying issues.
Providing a confidential opportunity for pressure release — "gripe dumping".
Reality checks — checking that perceptions are valid.
Reframing – reorienting a skewed perception to a more positive perspective.
Encouraging the JMO to ask for help and having him or her rehearse doing so confidently.
Professional counselling
Using problem-solving strategies and skills from a variety of psychological frameworks.
Building centring and anchoring triggers which help to maintain confidence and a calm demeanour.
Self-awareness and skills coaching in responsible assertion.
Self-awareness and skills coaching in anger management.
- Karen Grace1
- North Western Adelaide Health Service, Adelaide, SA.