Most of the research published about the maldistribution of the medical workforce in Australia has concentrated on shortages in rural general practice.1,2 Government medical workforce policies have generally focused on:
attracting and assisting rural students to study medicine;
exposing medical students to rural general practice; and
attracting and assisting medical graduates and practitioners into rural general practice.3
A qualitative review of issues surrounding rural specialist practice has been undertaken,4 but the importance of the barriers to rural consultant physician practice has not been quantified.
To rectify this deficiency, we surveyed all consultant physicians treating adults in both rural and metropolitan Victoria (Australia) to assess the perceived barriers to rural consultant physician practice.
Our study was undertaken in March 2000 under the auspices of the Royal Australasian College of Physicians (RACP). Postal questionnaires were sent to all Victorian Fellows of the Adult Medicine Division of the College in 1999. This group comprised 1027 registered consultant physicians, of whom 18 were retired or no longer in practice and 28 were overseas. Physicians' replies were sent by prepaid mail to the RACP office. Non-respondents were sent a second questionnaire and then followed up with one or more telephone calls until it was clear that a response was unlikely.
Rural practice was defined by the postcode of the primary residence and the primary practice and according to the Rural, Remote and Metropolitan Areas (RRMA) classification.5 Five physicians had rural postcodes for registration but lived and worked in metropolitan Victoria.
The questionnaire included demographic details, work profile (eg, type of practice, private and public mix of practice — based upon the biannual physician survey conducted by the RACP) and planned practice location changes.
Questions regarding barriers to rural practice were developed by us using both closed questions (ie, "yes" or "no" responses to the seven domains in Box 4: "Which of the following do you perceive as barriers to staying as or becoming a rural physician") and open questions (requests for a list of procedures they preferred not to perform and for physicians to give any other reasons for not becoming or not remaining a rural physician). Closed questions were asked about access to locums.
Data were entered into an Excel spreadsheet and then imported into the Statistical Package for the Social Sciences (SPSS) for analysis.6 All tests are two-tailed. Discrete variables were compared using the χ2 test and continuous variables using Student's t-test or Mann–Whitney U test. For the logistic regression, we used a forward conditional approach and then repeated it with a direct entry approach (threshold for entry, P = 0.05; for exit, P = 0.10; 20 iterations). No differences were found and direct entry results are shown. Age was divided into tertiles for the logistic regression.
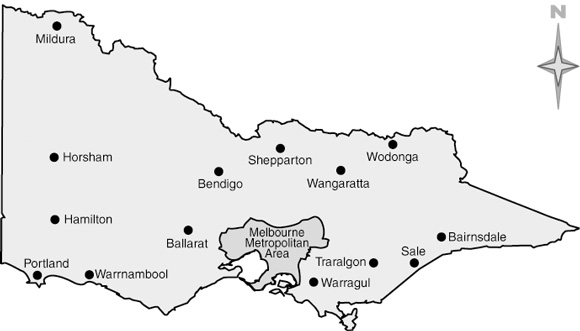
Responses were obtained from all 52 rural physicians and 634 of 929 (68.2%) metropolitan physicians. Of the 295 non-responding metropolitan physicians, 40 refused, 98 could not be contacted and 157 were contacted but did not respond. Box 1 shows the practice locations of the rural physicians.
Box 2 shows the characteristics of respondents.
Age/sex: Metropolitan and rural physicians were of a similar mean age (mean [SD], 46 [9] years), but had different age distributions (age ranges: metropolitan, 30–69 years; rural, 34–66 years). Their median (range) year of qualification was 1978 (1954–1999). There were no female consultant physicians working in rural Victoria.
Hours worked: Rural consultant physicians worked more hours overall (particularly in private practice), but less in research and were more likely to have an intern. While the proportion of rural and metropolitan physicians with a resident was similar, rural hospitals rarely had access to advanced trainees.
Place of birth: Rural physicians were more likely to be born in a rural area. Although only 17 (3.4%) metropolitan-born physicians worked in rural areas, they contributed 32.7% of the rural physician workforce.
Practice support: A range of practices in rural areas were supported (ie, there were subspecialists working there), although most rural physicians were general physicians. Metropolitan physicians provided visiting services to rural Victoria for a total of 226.5 hours per week.
Locums: There was no difference in the proportion of physicians obtaining a locum when needed, but rural physicians were more likely to seek a locum and more likely to cancel and change plans as a result of difficulties finding a locum.
The major obstacles to rural practice for both metropolitan and rural physicians were social (spouse's occupation [65.7%], children's schooling [72.2%] and other issues related to children [66.7%]). A substantial proportion were concerned about problems getting back to metropolitan practice (45.7%). Unfamiliar procedures (eg, ventilators, pacing wires, endoscopy, intensive care, coronary care and emergency management) were a concern for many (25.2%), as well as housing and depreciation in the value of housing (21.6% and 21.8%, respectively). Other barriers reported included loss of wider family support, ageing parents, access to religious and cultural venues, access to subspecialty facilities, academic isolation and lack of facilities, and long after-hours cover. The frequencies of the barriers were similar within each of the major specialties.
Box 4 shows the relationship using logistic regression between each of the key physician characteristics and the seven major barriers to rural practice for the metropolitan physicians.
Clear sex differences were found: female physicians were more concerned about spouse occupation and less concerned about getting back to metropolitan practice and housing depreciation than male physicians.
Physicians born in rural areas were less concerned about schools.
Physicians aged ≤ 40 years were more concerned about returning to metropolitan practice, those aged 41–50 years were more concerned about schooling, and those aged ≥ 51 years were more concerned about unfamiliarity with procedures.
Physicians not born in Australia were more concerned about returning to metropolitan practice.
This is the first major survey quantifying barriers to consultant physician practice in rural Australia. Our study has exposed some local myths. For example:
Difficulties in obtaining rural locums appear to be a function of an increased demand for locums rather than a reduced ability to obtain cover for a particular time period.
Rural consultant physicians are not older than their metropolitan counterparts, but the age distribution differs, with fewer younger physicians in rural practice.
Several respondents emphasised the contribution made by services visiting from the city, but we have shown clearly that this is relatively trivial. Furthermore, such services do not contribute to after-hours cover (commented upon by some respondents as a barrier to becoming a rural physician). Indeed, another study has shown that between 13.3% and 49.1% of rural patients (depending on remoteness of their residential area) travel to metropolitan areas for physician consultations,5 reflecting the limited capacity of both resident and visiting consultant physician services in many parts of rural Australia. There were no reported concerns regarding competition with visiting metropolitan physicians, although difficulties can occur in accessing health records during acute episodes in patients cared for by city-based services.
Rural consultant physicians were more likely to have interns. Access to resident staff was similar in rural and metropolitan areas, but until recently residents in rural areas were almost invariably basic trainees. The importance of placing advanced trainees in rural practice has been demonstrated previously — lack of exposure to rural practice during advanced training was associated with all physicians who were undecided about their preferred place of practice ending up in metropolitan practice, as did several of those intending to become rural practitioners.7
The ethics of attracting overseas-trained physicians to rural positions is debatable,8,9 but our data suggest that there may be additional risks. Non-Australian-born graduates expressed significant concern about not being able to get back to metropolitan practice, which might mean a greater likelihood of overseas-trained physicians moving to the city from rural areas once this is possible.
Physicians born in rural areas and now practising in the city are less likely to view schooling as a barrier to rural practice. This suggests that those born in metropolitan areas have an exaggerated negative view of schools in provincial centres. While those in rural and remote settings are less likely to go to university,10 many of the schools in towns able to support consultant physician practice perform well educationally. The negative metropolitan view of rural schools parallels the negative view of rural health services and practice, which appears to be instilled at a young age. In a recent study among first-year medical students, those born in metropolitan areas were less likely than rural-born students to view rural practice positively.11 A key feature was a difference in the source of metropolitan and rural students' information — the media and personal exposure, respectively. This suggests that proactive approaches to media reporting, and rebutting unbalanced reporting, may be needed, along with, of course, genuine attempts to deal with the cause of any negative stories (eg, schools with difficulties in retaining or attracting suitably qualified teachers).
The major importance of education and other family issues in choice of practice location is similar to that found among general practitioners.2 Clearly, female participation is a major issue for the whole medical profession,12 but the absence of any female consultant physician in rural Victoria is a measure of the extent of the need for urgent action in rural practice. Family and professional issues have been identified as an issue for younger male physicians,13,14 and without intervention the ability to maintain the rural consultant physician workforce is likely to become increasingly difficult.
This was a common theme, and, for some, a reason for departure from rural practice. Coping with bureaucracy has also been found to be a reason for leaving rural practice among general practitioners.15 It is unclear whether such conflicts were in response to the greater difficulties experienced in rural hospitals during the economic limitations imposed in Victoria in the 1990s.16 An alternative explanation is that the impacts of conflicts are amplified in rural areas, where people have multiple roles and "strong ties", and where mutual avoidance can be difficult.17 In such a setting, conflicts have more severe and wide-ranging implications.
While performing procedures is attractive to many rural GPs,15 we found that this may be a barrier to practice as a rural consultant physician, particularly among older physicians. This finding is significant in that there appear to be older physicians whose children are grown up (and perhaps have left home) who may be willing to move to rural practice if the problem of unfamiliar procedures can be overcome. Increasing the number of advanced trainees should help, as well as courses which upskill (or reskill) older consultant physicians.
Through its Rural Workforce and Training Program, the RACP already undertakes a number of initiatives in support of Fellows and trainees in regional and rural Australia. Funding assistance has been received from the Commonwealth Department of Health and Ageing and various State government health departments to implement some of these activities (Box 5).
The major barriers to rural consultant physician practice are social and outside the health sector. However, access to additional training, making available and publicising widely known mechanisms for re-entry into metropolitan practice, such as linkage of rural positions with metropolitan clinical activities, and the growth in rural academic facilities are all likely to be helpful.
2: Characteristics of rural and metropolitan physicians
Characteristics |
Metropolitan practice |
Rural practice |
|||||||||
Age/sex (%) |
|||||||||||
≤ 40 years |
32.1% |
19.2%* |
|||||||||
41–50 years |
32.7% |
48.1%* |
|||||||||
51 years and over |
35.2% |
32.7%* |
|||||||||
Male |
79.7% |
100%† |
|||||||||
Place of birth (%) |
|||||||||||
Australia |
74.9% |
71.2% |
|||||||||
Rural area |
11.0% |
67.3%† |
|||||||||
Metropolitan area |
89.0% |
32.7%† |
|||||||||
Type of physician (%) |
|||||||||||
General physician |
19.7% |
64.9%† |
|||||||||
General physician plus major specialty |
11.9% |
28.1%† |
|||||||||
Other medical specialty |
68.4% |
7.0%† |
|||||||||
Assistance (%) |
|||||||||||
Intern |
41.5% |
70.6%† |
|||||||||
Resident (basic/advanced trainee) |
75.1% |
76.5% |
|||||||||
Hours worked (mean, 95% CI) |
|||||||||||
Total hours/week |
54 (53–56) |
60 (54–65)* |
|||||||||
Hours/week in public hospitals |
16 (15–18) |
17 (13–21) |
|||||||||
Hours/week in private practice |
21 (20–23) |
34 (28–40)† |
|||||||||
Hours/week in research |
12 (10–13) |
3 (1–4)† |
|||||||||
Private practice (%) |
|||||||||||
Proportion of total hours engaged in private practice |
37% (34%–40%) |
54% (44%–64%)† |
|||||||||
All private practice |
6.4% |
5.6% |
|||||||||
No private practice |
26.3% |
24.1% |
|||||||||
Locum availability (%) |
|||||||||||
Sought locum in past 12 months |
25.8% |
40.0%* |
|||||||||
Proportion of these locum requests successful |
81.6% |
75.0% |
|||||||||
Ever not able to obtain a locum and had to cancel plans |
13.1% |
26.8%* |
|||||||||
Ever not able to obtain a locum and had to change plans |
22.4% |
42.1%† |
|||||||||
Changing practice |
|||||||||||
Planning to move practice or retire |
6.9% |
1.9% |
|||||||||
* Metropolitan v rural compared using two-tailed Student's t test or χ2 test. *P < 0.05. † P < 0.01. |
|||||||||||
3: Major barriers to rural practice
Barrier |
Metropolitan
physicians |
Rural
physicians |
|||||||||
Spouse's occupation |
65.0% |
74.5% |
|||||||||
Children's schooling |
72.9% |
63.8% |
|||||||||
Moving children |
67.6% |
55.3% |
|||||||||
Difficulties getting back into metropolitan practice |
46.1% |
40.4% |
|||||||||
Unfamiliarity with some procedures |
24.3% |
36.2% |
|||||||||
Housing |
22.4% |
12.8% |
|||||||||
Housing depreciation |
21.7% |
23.4% |
|||||||||
Data missing for five respondents. Metropolitan v rural compared using χ2 tests (no significant differences were found). |
|||||||||||
4: Odds ratios (95% CIs)* for reporting key barriers to rural practice among metropolitan physicians, by physician characteristics
Barriers (reference) |
Social |
Difficulties getting back into metropolitan practice |
Fear of procedures |
Housing |
Housing depreciation |
||||||
Spouse occupation |
Schooling |
Children |
|||||||||
Sex (male) |
|||||||||||
Female |
1.97 |
1.13 |
1.50 |
0.58 |
1.47 |
1.05 |
0.43 |
||||
95% CI |
(1.21–3.21) |
(0.68–1.87) |
(0.92–2.43) |
(0.37–0.90) |
(0.89–2.41) |
(0.63–1.75) |
(0.24–0.79) |
||||
Place of birth (rural) |
|||||||||||
Metropolitan |
0.96 |
1.82 |
1.64 |
1.04 |
0.74 |
1.39 |
0.77 |
||||
95% CI |
(0.53–1.73) |
(1.02–3.24) |
(0.93–2.90) |
(0.59–1.83) |
(0.40–1.37) |
(0.68–2.84) |
(0.42–1.52) |
||||
Age (age ≤ 40 years) |
|||||||||||
Age 41–50 years |
0.75 |
1.42 |
1.92 |
0.47 |
0.81 |
1.05 |
1.08 |
||||
95% CI |
(0.49–1.16) |
(0.88–2.30) |
(1.22–3.02) |
(0.31–0.71) |
(0.49–1.34) |
(0.64–1.70) |
(0.66–1.77) |
||||
Age ≥ 51 years |
0.74 |
0.68 |
0.95 |
0.49 |
1.84 |
1.05 |
0.83 |
||||
95% CI |
(0.47–1.17) |
(0.42–1.09) |
(0.61–1.49) |
(0.32–0.77) |
(1.12–3.02) |
(0.62–1.76) |
(0.49–1.40) |
||||
Nationality at birth (Australian) |
|||||||||||
Not Australian |
1.13 |
1.00 |
1.25 |
1.58 |
1.12 |
1.34 |
1.13 |
||||
95% CI |
(0.75–1.73) |
(0.64–1.55) |
(0.81–1.93) |
(1.06–2.36) |
(0.71–1.76) |
(0.85–2.12) |
(0.70–1.82) |
||||
Data missing for five respondents. * Odds ratios (95% CIs) by direct entry logistic regression. |
|||||||||||
5: Rural initiatives of the Royal Australasian College of Physicians
For Fellows |
For Advanced Trainees |
||||||||||
Locum coordination program |
Rural advanced training scholarships |
||||||||||
Assistance with accessing continuing medical education |
Mentor program |
||||||||||
Annual continuing medical education fellowships and grants |
Training program support and advice |
||||||||||
Development of advanced training programs |
Training module (in development) |
||||||||||
Policy and program advocacy |
Accreditation of training hospitals |
||||||||||
Workforce policy development |
|||||||||||
Workforce survey and analysis |
|||||||||||
Support of regional physician networks |
|||||||||||
- David Simmons1
- Les E Bolitho2
- Grant J Phelps3
- Rob Ziffer4
- Gary J Disher5
- 1 Department of Rural Health, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Shepparton, VIC.
- 2 Wangaratta, VIC.
- 3 Ballarat, VIC.
- 4 Sale, VIC.
- 5 Royal Australasian College of Physicians, Sydney, NSW.
None declared.
- 1. Rosenman SJ, Batman GJ. Trends in general practitioner distribution from 1984 to 1989. Aust J Public Health 1992; 16: 84-88.
- 2. Humphreys JS, Rolley F. A modified framework for rural general practice: the importance of recruitment and retention. Soc Sci Med 1998; 46: 939-945.
- 3. Commonwealth of Australia. Budget 2000–2001. Available at: http://www.health.gov.au/budget2000/ (accessed June 2001).
- 4. Australian Medical Workforce Advisory Committee. The Medical workforce in rural and remote Australia. Sydney: AMWAC, 1996.
- 5. Australian Institute of Health and Welfare. Health in rural and remote Australia. Canberra: AIHW, 1998.
- 6. SPSS [computer program], version 9. Chicago, Ill: SPSS, 2001.
- 7. Kanaragarajah S, Page JH, Heller RF. Changes in job aspirations during physician training in Australia. Aust N Z J Med 1996; 26: 652-657.
- 8. Medical migration and inequity of health care [editorial]. Lancet 2000; 356: 177.
- 9. Bundred PE, Levitt C. Medical migration: who are the real losers? Lancet 2000; 356: 245-246.
- 10. James R, Wyn J, Baldwin G, et al. Rural and isolated school students and their higher education choices. Canberra: AGPS, 1999.
- 11. Azer S, Simmons D, Elliott S. Rural training and the state of rural health services: effect of rural background on perception and attitude of the first year medical students at the University of Melbourne. Aust J Rural Health 2001. In press.
- 12. Australian Medical Workforce Advisory Committee and Australian Institute of Health and Welfare. Female participation in the Australian medical workforce. Sydney: AMWAC, 1996 (AMWAC report 1996.7).
- 13. Dumelow C, Littlejohns P, Griffiths S. Relation between a career and family life for English hospital consultants: qualitative, semistructured interview study. BMJ 2000; 320: 1437-1440.
- 14. Buske L. Are men losing interest in medical careers? CMAJ 1998; 159: 740.
- 15. Kamien M. Staying in or leaving rural practice: 1996 outcomes of rural doctors' 1986 intentions. Med J Aust 1998; 169: 318-321. <eMJA full text>
- 16. Buckley P, Marley J, Robinson J, et al. Coountry profile: Australia. Lancet 1998; 351: 1569-1578.
- 17. Wilkinson KP. The community in rural America. New York: Greenwood Press, 1991.





Abstract
Objective: To quantify the barriers to practising as a rural consultant physician.
Design: Cross-sectional postal survey.
Participants: All 981 practising consultant physicians in Victoria, Australia, who were Fellows of the Royal Australasian College of Physicians in 1999; 52 (100%) of rural physicians and 634 (68.2%) of metropolitan physicians completed the survey.
Main outcome measures: Demographic and practice characteristics; barriers to rural practice.
Results: There were no rural female consultant physicians, and 35 of the 52 rural consultant physicians (67.3%) were born in a rural area. The most important perceived barriers to rural practice identified by both metropolitan and rural physicians were children's schooling (72.2%), spouse's occupation (65.7%), other issues related to children (66.7%) and difficulties getting back into metropolitan practice (45.7%). Among metropolitan physicians, barriers to rural practice differed by age, sex, place of birth and nationality. Returning to metropolitan practice, children and concern over procedures were more likely to be reported as barriers to rural practice among those aged 40 years or under, 41–50 years and 51 years and over, respectively.
Conclusion: The major barriers to rural practice identified by physicians lie outside the health sector, and particularly concern a perceived need for wider opportunities in children's education and spouse employment.