This is a republished version of an article previously published in MJA Open
In Australia, the 12-month prevalence of anxiety disorders is 14.4% and of affective disorders, 6.2%.1 It has been demonstrated that 39% of individuals with generalised anxiety disorder (GAD) also meet criteria for depression.2 About 85% of patients with depression also experience significant symptoms of anxiety, while comorbid depression occurs in up to 90% of patients with anxiety disorders.3 Considering anxiety and depression symptoms together in a “mixed anxiety-depressive disorder” has been proposed,4 but it is useful to identify and institute effective treatment for each set of symptoms. They can occur in all age groups — almost 50% of older adults with 12-month history of GAD met criteria for lifetime major depressive disorder, while only 7.4% of those without GAD met these criteria.5 Both anxiety and depression are associated with substance use disorder,6 and about 7% of the affected population represent serious cases with high comorbidity.7
Up to 25% of the patients seen in general practice have comorbid anxiety and depression.8 Though recognised in both rural and non-rural primary care, there is often a treatment gap, with patients undertreated for either or both disorders.9 Patients with anxiety and/or depression are particularly likely to present with physical complaints rather than mental health symptoms,10 and symptomatology may initially seem vague and non-specific.
Developmentally, anxiety disorders are almost always the primary condition, with onset usually occurring in childhood or adolescence.11 Comorbidity of anxiety and depression is explained mostly by a shared genetic vulnerability to both disorders, or by one disorder being an epiphenomenon of the other.12
Increased corticotropin-releasing factor in cerebrospinal fluid has been reported in both anxiety and depression, but other peptides or hormones of the hypothalamic–pituitary–adrenal axis are regulated differently in the two disorders.13 More recently, neuroinflammatory, oxidative and nitrosative pathways have been implicated in depression and its comorbidities.14 It is most likely that the first episode of depression in a person’s life follows a psychosocial stressor. After three or more episodes, it becomes increasingly likely that subsequent episodes are spontaneous rather than following an external event.15
Comorbid depression and anxiety can increase impairment16,17 and health care use,18 compared with either disorder alone. Their co-occurrence is often associated with a poor prognosis19 and significant detrimental impact on functioning in the workplace.20 The number and severity of anxiety symptoms, rather than the specific anxiety diagnosis, correlate strongly with the persistence of subsequent depressive symptoms, and this relationship is stable over decades (Box 1).21
Many people do not seek treatment for anxiety and depression and, when they do, treatments are not always used effectively. Australian data suggest that 40% of people with current disorders did not seek treatment in the previous year and, of those who did, only 45% were offered a treatment that could be beneficial.22 Despite the high prevalence of depression and anxiety, and notwithstanding Australia’s universal health insurance scheme, service utilisation in this country is low. An Australian survey published in 2001 indicated that only 35% of people with a mental disorder had consulted a health professional for a mental health problem during the previous year, but most had seen a GP for that disorder or for some other health reason.23 In this setting, barriers to effective care were stated to be patient knowledge and physician competence.
It is important to delineate the specific depressive disorder and the specific anxiety disorder, as each may require different interventions. The most prevalent anxiety disorders in Australia are post-traumatic stress disorder (6.4%), social phobia (social anxiety disorder; 4.7%), agoraphobia (2.8%), GAD (2.7%), panic disorder (2.6%) and obsessive–compulsive disorder (1.9%). Of the population aged 16–85 years, 14.4% have an anxiety disorder. The prevalence of depression is 6.2%, with the prevalence of unipolar depressive episodes being 4.1%, dysthymia, 1.3%, and bipolar disorder, 1.8%.1 Some patients have two or more disorders.
Diagnostic criteria are designed to distinguish between disorders, and exclude clinical features that are common to more than one. Thus, criteria for depression exclude common comorbid anxiety symptoms, and those for anxiety disorders exclude depressive symptoms. However, diagnostic criteria are not the same as clinical presentations. Some somatic symptoms that can occur with both depression and anxiety are outlined in Box 2.
Despite data suggesting that the accuracy of depression recognition by non-psychiatrists is low,24 the best remedy for this is not clear. Rating scales for depression and anxiety can be helpful, although most are designed to assess the severity of an already diagnosed illness rather than to make a new diagnosis.
A screening instrument that can be used to make a diagnosis and distinguish between illnesses, including unipolar and bipolar depression, is the Mini International Neuropsychiatric Interview.25 Other instruments that can be used to identify the severity (but not the type) of depression include the Kessler Psychological Distress Scale,26 the Hospital Anxiety and Depression Scale,27 or the 12-item Somatic and Psychological Health Report questionnaire.28 The Clinical Global Impression scale is a simple seven-point scale that can be used to monitor progress of treatment response.29
In the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, about half of the patients with major depressive disorder also had clinically meaningful levels of anxiety.30 Remission was significantly less likely and took longer in the 53% of patients with anxious depression than in those with non-anxious depression. Side-effect frequency, intensity and burden, as well as the number of serious adverse events, were significantly greater and outcomes worse in the group with anxious depression.
There is a paucity of data on the treatment of patients with comorbid depression and anxiety, and clinical practice is therefore determined by treating individual anxiety and depressive disorders. There are also online resources that can help, including the Australian National University’s MoodGYM (http://www.moodgym.anu.edu.au) and E-couch (http://www.ecouch.anu.edu.au), Swinburne University’s Anxiety Online (http://www.anxietyonline.org.au), and information sites from beyondblue (http://www. beyondblue.org.au), Youthbeyondblue (http://www. youthbeyondblue.com) and the Black Dog Institute (http://www.blackdoginstitute.org.au).
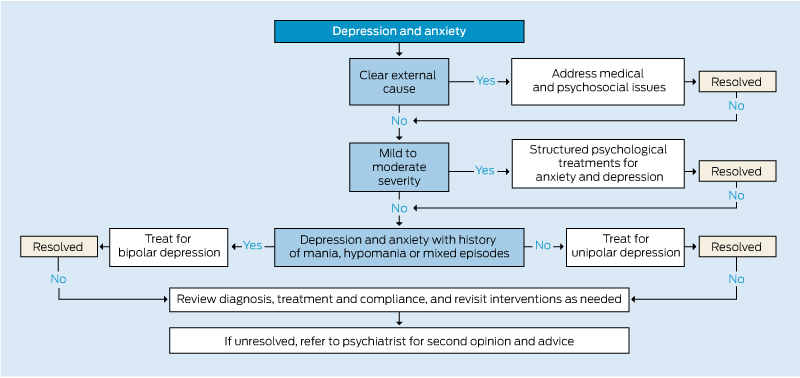
Treatments for anxiety and depression can have substantial elements in common (Box 3). Initial steps are making the diagnosis, explaining symptomatology, and providing hope. Psychosocial interventions, including clinical support, education and rehabilitation, are valuable. For patients with mild to moderately severe depression and anxiety, structured psychological treatments, available under the federal government’s “Better Access” scheme, will often suffice.31
For patients with more severe illness or those who do not respond to psychological interventions, pharmacotherapy is indicated. Pharmacotherapy particularly decreases over-activity of limbic structures of the brain (bottom-up effect), whereas psychotherapy tends to increase activity and recruitment of frontal areas (top-down effect).32
The psychological treatment with the greatest evidence base for depression is cognitive behaviour therapy (CBT).33 CBT is a beneficial treatment that can be readily applied in medical practice. The principles involve educating the patient, teaching basic relaxation skills, and developing the patient’s skills to identify, challenge and change maladaptive thoughts, feelings, perceptions and behaviour.34 Systematic reviews and meta-analyses have shown evidence of efficacy in inpatients with depression35 and those with chronic physical health problems.36 A systematic review showed improved outcomes for patients by enhancing antidepressant therapy with non-pharmacological interventions.37 Psychological treatments for depression are detailed elsewhere in this supplement (see Casey et al).38
Guidance regarding treatment of anxiety disorders can be found in a practical clinician guide and patient manuals,39 and in an overview of management in general practice.40 For GAD, a systematic review showed similar treatment effects for pharmacotherapy (odds ratio [OR] favouring active interventions over controls, 0.32; 95% CI, 0.18–0.54) and psychotherapy (OR, 0.33; 95% CI, 0.17–0.66).41
Antidepressants are the mainstay of treating unipolar depression,42 with present agents working mostly through serotonergic, noradrenergic, and dopaminergic receptors (see Chan et al).43 An increase in prescribing of antidepressants in general practice in recent years coincided with the introduction of the Better Access initiative, which may have increased recognition of depression.44 Antidepressant combinations may add to adverse events without necessarily providing therapeutic advantage, and some authorities do not support such use.45 There is a new focus on normalising endogenous circadian rhythms in the treatment of depression and anxiety.46 Bipolar depression needs different treatment (see Berk et al).47
Low doses of atypical antipsychotic agents can reduce anxiety,48 but there is a risk of tardive dyskinesia with long-term use, and metabolic problems are associated with some of these agents.
Antidepressants are the main options for long-term pharmacological treatment of anxiety disorders.42 The choice of antidepressant depends on the prescribing doctor’s knowledge of the medicine, a history of prior successful response to a particular agent by the patient or a close relative, or specific qualities of a particular medicine.
2 Somatic symptoms that can occur with anxiety and depression
Musculoskeletal
Muscle aches and pains, muscle tension, headaches
Gastrointestinal
Dry mouth, choking sensation, “churning stomach” sensation, nausea, vomiting, diarrhoea
Cardiovascular
Palpitations, tachycardia, chest pain, flushing
Respiratory
Shortness of breath, occasionally hyperventilation
Neurological
Dizziness, vertigo, blurred vision, paraesthesia
Genitourinary
Loss of sex drive, difficulties with micturition
Provenance: Commissioned by supplement editors; externally peer reviewed.
- John W G Tiller1
- University of Melbourne, Melbourne, VIC.
I thank Iveta Krivonos, research assistant, for assisting in the preparation of this article.
I hold an unpaid position on the Board of Directors of Therapeutic Guidelines Ltd and have received speaker fees and travel assistance from AstraZeneca, Eli Lilly, Lundbeck and Pfizer.
- 1. Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: summary of results, 2007. Canberra: ABS, 2007. (ABS Cat. No. 4326.0.) http://www.abs.gov.au/ausstats/abs@.nsf/mf/4326.0 (accessed Sep 2012).
- 2. Hunt C, Issakidis C, Andrews G. DSM-IV generalized anxiety disorder in the Australian National Survey of Mental Health and Well-Being. Psychol Med 2002; 32: 649-659.
- 3. Gorman JM. Comorbid depression and anxiety spectrum disorders. Depress Anxiety 1996-1997; 4: 160-168.
- 4. Pollack MH. Comorbid anxiety and depression. J Clin Psychiatry 2005; 66 Suppl 8: 22-29.
- 5. Gonçalves DC, Pachana NA, Byrne GJ. Prevalence and correlates of generalized anxiety disorder among older adults in the Australian National Survey of Mental Health and Well-Being. J Affect Disord 2011; 132: 223-230.
- 6. Regier DA, Rae DS, Narrow WE, et al. Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. Br J Psychiatry Suppl 1998; (34): 24-28.
- 7. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 617-627.
- 8. Sartorius N, Ustün TB, Lecrubier Y, Wittchen HU. Depression comorbid with anxiety: results from the WHO study on psychological disorders in primary health care. Br J Psychiatry Suppl 1996; (30): 38-43.
- 9. Jameson JP, Blank MB. Diagnosis and treatment of depression and anxiety in rural and nonrural primary care: national survey results. Psychiatr Serv 2010; 61: 624-627.
- 10. Goldberg D. Epidemiology of mental disorders in primary care settings. Epidemiol Rev 1995; 17: 182-190.
- 11. Wittchen HU, Kessler RC, Pfister H, Lieb M. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatr Scand Suppl 2000; (406): 14-23.
- 12. Middeldorp CM, Cath DC, Van Dyck R, Boomsma DI. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychol Med 2005; 35: 611-624.
- 13. Boyer P. Do anxiety and depression have a common pathophysiological mechanism? Acta Psychiatr Scand Suppl 2000; (406): 24-29.
- 14. Maes M, Kubera M, Obuchowiczwa E, et al. Depression’s multiple comorbidities explained by (neuro)inflammatory and oxidative & nitrosative stress pathways. Neuro Endocrinol Lett 2011; 32: 7-24.
- 15. Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the “kindling” hypothesis. Am J Psychiatry 2000; 157: 1243-1251.
- 16. Kuzel RJ. Treating comorbid depression and anxiety. J Fam Pract 1996; 43 (6 Suppl): S45-S53.
- 17. Brown C, Schulberg HC, Madonia MJ, et al. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry 1996; 153: 1293-1300.
- 18. Andersson D, Magnusson H, Carstensen J, Borgquist L. Co-morbidity and health care utilisation five years prior to diagnosis for depression. A register-based study in a Swedish population. BMC Public Health 2011; 11: 552.
- 19. Katon W, Unützer J, Russo J. Major depression: the importance of clinical characteristics and treatment response to prognosis. Depress Anxiety 2010; 27: 19-26.
- 20. McIntyre RS, Liauw S, Taylor VH. Depression in the workforce: the intermediary effect of medical comorbidity. J Affect Disord 2011; 128 Suppl 1: S29-S36.
- 21. Coryell W, Fiedorowicz JG, Solomon D, et al. Effects of anxiety on the long-term course of depressive disorders. Br J Psychiatry 2012; 200: 210-215.
- 22. Andrews G, Sanderson K, Slade T, Issakidis C. Why does the burden of disease persist? Relating the burden of anxiety and depression to effectiveness of treatment. Bull World Health Organ 2000; 78: 446-454.
- 23. Andrews G, Henderson S, Hall W. Prevalence, comorbidity, disability and service utilisation. Overview of the Australian National Mental Health Survey. Br J Psychiatry 2001; 178: 145-153.
- 24. Cepoiu M, McCusker J, Cole MG, et al. Recognition of depression by non-psychiatric physicians – a systematic literature review and meta-analysis. J Gen Intern Med 2008; 23: 25-36.
- 25. Sheehan DV, Lecruibier Y. MINI Mini International Neuropsychiatric Interview. English version 5.0.0. 2006. http://www.nccpsychiatry.info/File/MINI500.pdf (accessed Sep 2012).
- 26. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32: 959-976.
- 27. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67: 361-370.
- 28. Hickie IB, Davenport TA, Hadzi-Pavlovic D, et al. Development of a simple screening tool for common mental disorders in general practice. Med J Aust 2001; 175 (2 Suppl): S10-S17.
- 29. Guy W. ECDEU assessment manual for psychopharmacology. Revised, 1976. Rockville, Md: National Institute of Mental Health, 1976.
- 30. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry 2008; 165: 342-351.
- 31. Australian Government Department of Health and Ageing. Better access to psychiatrists, psychologists and general practitioners through the MBS (Better Access) initiative. http://www.health.gov.au/mentalhealth-betteraccess (accessed Sep 2012).
- 32. Quidé Y, Witteveen AB, El-Hage W, et al. Differences between effects of psychological versus pharmacological treatments on functional and morphological brain alterations in anxiety disorders and major depressive disorder: a systematic review. Neurosci Biobehav Rev 2012; 36: 626-644.
- 33. Fava GA, Ruini C, Rafanelli C, et al. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry 2004; 161: 1872-1876.
- 34. Tiller JWG. Cognitive behaviour therapy in medical practice. Aust Prescr 2001; 24: 33-37. http://www.australianprescriber.com/magazine/24/2/33/7 (accessed Sep 2012).
- 35. Cuijpers P, Clignet F, van Meijel B, et al. Psychological treatment of depression in inpatients: a systematic review and meta-analysis. Clin Psychol Rev 2011; 31: 353-360.
- 36. Rizzo M, Creed F, Goldberg D, et al. A systematic review of non-pharmacological treatments for depression in people with chronic physical health problems. J Psychosom Res 2011; 71: 18-27.
- 37. Oestergaard S, Møldrup C. Improving outcomes for patients with depression by enhancing antidepressant therapy with non-pharmacological interventions: a systematic review of reviews. Public Health 2011; 125: 357-367.
- 38. Casey MF, Perera DN, Clarke DM. Psychosocial treatment approaches to difficult-to-treat depression. MJA Open 2012; 1 Suppl 4: 52-55.
- 39. Andrews G, Creamer M, Crino R, et al, editors. The treatment of anxiety disorders: clinician guides and patient manuals. 2nd ed. Cambridge: Cambridge University Press, 2003.
- 40. Kyrios M, Mouding R, Nedeljkovic M. Anxiety disorders – assessment and management in general practice. Aust Fam Physician 2011; 40: 370-374.
- 41. Gonçalves DC, Byrne GJ. Interventions for generalized anxiety disorder in older adults: systematic review and meta-analysis. J Anxiety Disord 2012; 26: 1-11.
- 42. Therapeutic Guidelines Limited. eTG complete. 2012. http://www.tg.org.au/index.php?sectionid=71 (accessed Sep 2012).
- 43. Chan HN, Mitchell PB, Loo CKA, Harvey SB. Pharmacological treatment approaches to difficult-to-treat depression. MJA Open 2012; 1 Suppl 4: 44-47.
- 44. Harrison C, Britt H, Charles J. Antidepressant use. Aust Fam Physician 2011; 40: 365.
- 45. Keks NA, Burrows GD, Copolov DL, et al. Beyond the evidence: is there a place for antidepressant combinations in the pharmacotherapy of depression? Med J Aust 2007; 186: 142-144. <MJA full text>
- 46. Monteleone P, Martiadis V, Maj M. Circadian rhythms and treatment implications in depression. Prog Neuropsychopharmacol Biol Psychiatry 2011; 35: 1569-1574.
- 47. Berk M, Berk L, Davey CG, et al. Treatment of bipolar depression. MJA Open 2012; 1 Suppl 4: 32-35.
- 48. Vulink NCC, Figee M, Denys D. Review of atypical antipsychotics in anxiety. Eur Neuropsychopharmacol 2011; 21: 429-449.





Summary
Comorbid depression and anxiety disorders occur in up to 25% of general practice patients.
About 85% of patients with depression have significant anxiety, and 90% of patients with anxiety disorder have depression.
Symptomatology may initially seem vague and non-specific. A careful history and examination with relevant investigations should be used to make the diagnosis.
Once the diagnosis is made, rating scales may identify illness severity and help in monitoring treatment progress.
Both the depression disorder and the specific anxiety disorder require appropriate treatment.
Psychological therapies, such as cognitive behaviour therapy, and antidepressants, occasionally augmented with antipsychotics, have proven benefit for treating both depression and anxiety.
Benzodiazepines may help alleviate insomnia and anxiety but not depression. They have dependency and withdrawal issues for some people, and may increase the risk of falls in older people.
Despite the availability of treatments, 40% of patients with depression or anxiety do not seek treatment, and of those who do, less than half are offered beneficial treatment.