Climatic heat extremes cause heat‐related illnesses such as heat stroke, exacerbate other medical conditions, and can lead to death.1 However, the effect of heat on the number of people who present to emergency departments with mental illness is less well explored. We therefore examined the effects of temperature, humidity, and air pollution on presentations with mental health problems to the emergency department of Westmead Hospital, the major tertiary hospital in the Greater Western Sydney region, during 1 January 2015 – 31 December 2019, by sex, age, and psychiatric diagnosis category. We analysed de‐identified data from the Patient Health Care Records dataset. Major mental illnesses were classified according to the International Classification of Diseases, tenth revision (ICD‐10). Meteorological data were obtained from the Parramatta North (Masons Drive) meteorological station (66124) and the New South Wales Department of Planning, Industry and Environment station at Prospect. Our study was approved by the Western Sydney Local Health District Human Research Ethics Committee (2020/ETH02198).
The relationship between maximum daily temperature and number of emergency mental health presentations was modelled in a distributed lag non‐linear model, with a quasi‐Poisson distributed response variable and fixed effects of sex, age, and primary ICD‐10 diagnosis group; the number of attributable presentations was estimated using the method described by Gasparrini and Leone2 (further details: Supporting Information). We did not adjust our final model for daily pollutant concentrations (ie, particulate matter with a diameter of 10 μm or less [PM10], nitrogen dioxide [NO2], or sulfur dioxide [SO2]) or humidity, as doing so did not improve the overall fit of the model. We compared the number of psychiatric presentations by temperature with the number at the median maximum temperature during 2015–2019 as reference (23.8°C; interquartile range, 20.0–28.0°C); we report relative risks (RRs) with 95% confidence intervals (CIs). Statistical analyses were undertaken in R 4.2.1 (R Foundation for Statistical Computing).
Of 372 723 presentations to the Westmead Hospital emergency department during 2015–2019, 4438 were attributed to mental illness (1.2%): neurotic, stress‐related, and somatoform disorders (F40–F48), 2091 people (47.1%); mood (affective) disorders (F30–F39), 1262 people (28.4%); schizophrenia and schizotypal and delusional disorders (F20–F29), 948 people (21.4%); behavioural syndromes associated with physiological disturbances and physical factors (F50–F59), 73 people (1.6%); and disorders of adult personality and behaviour (F60–F69), 64 people (1.4%). The mean age of people presenting with mental illness was 35.6 years (standard deviation, 14.6 years); 2333 were women (52.6%); 2234 people (50.3%) were admitted or transferred to inpatient psychiatric services.
Daily maximum temperatures during 2015–2019 ranged between 12.2 and 45.0°C; 209 mental health presentations (4.7%) were on days with maximum temperatures at or above the 95th percentile (35.2°C). Compared with the median maximum temperature of 23.8°C, the risk of presentation (men and women combined) increased beyond 36°C, but was not statistically significant at either the 80th (29.2°C; RR, 1.03; 95% CI, 0.999–1.07) or 95th temperature percentiles (35.2°C; RR, 1.07; 95% CI, 0.996–1.14). For women, the risk of presentation increased steadily for temperatures between 28°C and 38°C, and was statistically significant at the 80th (RR, 1.09; 95% CI, 1.04–1.15) and 95th percentiles (RR, 1.17; 95% CI, 1.06–1.30). This risk corresponds to 215 (95% CI, 61–352) attributable presentations at the 80th percentile and 54 (95% CI, 1–98) at the 95th percentile across the study period. The risk was not statistically significant for men at either percentile (80th: RR, 1.03; 95% CI, 0.97–1.10; 95th: RR, 1.10; 95% CI, 0.97–1.25) (Box). Differences by age or ICD‐10 diagnosis category were not evident, nor lag‐specific effects (data not shown).
High temperatures can predispose some people to mental distress or maladaptive and risky behaviour, and they compromise physical health by thermoregulatory and pharmacological mechanisms.3 Socio‐economic factors such as poverty influence access to adaptive architecture and air‐conditioning.4 The greater effect of heat on women than men in our study may reflect a greater propensity to fluid restriction in women with eating disorders or depression, as acclimatised women are not generally more sensitive to higher temperatures than men.5
Enhancing support and allocating additional resources during periods of extreme heat could alleviate the burden on emergency departments and provide better care for people with mental health problems. Moreover, similar presentation patterns may pertain elsewhere as global temperatures rise, and health system mental health strategies may need to take climate factors into consideration. This could include developing early warning systems, integrating temperature data into mental health risk assessments, and targeting interventions to people at greatest risk of heat‐related mental stress.
Our study was limited by its basis in health care data from one large emergency department and two nearby meteorological stations. As temperatures above 40°C were rare, our model could not reliably predict the effect of extreme heat on presentation numbers. Repeated presentations by the same people were not specifically identified. Additional factors potentially relevant to our meteorological (eg, wind speed) and mental health measures (eg, medication use) were not included in our models.
In conclusion, our study should alert health services to the potential effects of high ambient temperatures on the frequency of mental health presentations to emergency departments, particularly by women, for whom the risk rises significantly at temperatures of 29.2°C or more. It is important that we recognise the concerns of people with mental illness and develop specific advice related to mental health care during climate extremes in order to mitigate the effects of rising temperatures on people at particular risk.
Box – Relative risk of psychiatric hospital presentation to Westmead Hospital emergency department, 2015–2019, by maximum daily temperature and sex: exposure–response curves*
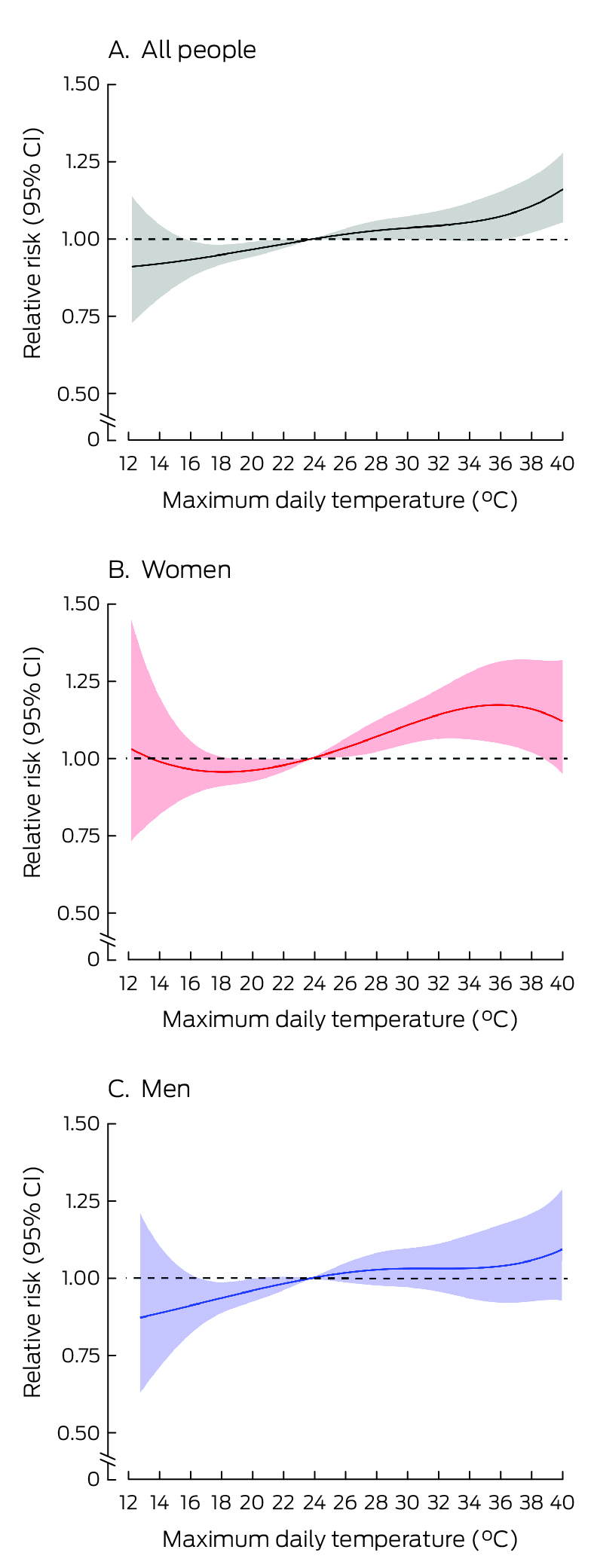
* Reference value: median maximum temperature during 2015–2019 (23.8°C). As there were only 38 psychiatric presentations on days when temperatures exceeded 40°C, the graph is truncated at this temperature.
Received 30 March 2023, accepted 30 November 2023
- 1. Ye X, Wolff R, Yu W, et al. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect 2012; 120: 19‐28.
- 2. Gasparrini A, Leone M. Attributable risk from distributed lag models. BMC Med Res Methodol 2014; 14: 55.
- 3. Liu J, Varghese BM, Hansen A, et al. Is there an association between hot weather and poor mental health outcomes? A systematic review and meta‐analysis. Environ Int 2021; 153: 106533.
- 4. Thompson R, Hornigold R, Page L, Waite T. Associations between high ambient temperatures and heat waves with mental health outcomes: a systematic review. Public Health 2018; 161: 171‐191.
- 5. Foster J, Hodder SG, Lloyd AB, Havenith G. Individual responses to heat stress: implications for hyperthermia and physical work capacity. Front Physiol 2020; 11: 541483.






Open access:
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
Data sharing:
The data underlying the findings of this study are available from the corresponding author upon reasonable request.
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
No relevant disclosures.