“Who should get the last ventilator?” was an esoteric ethics question until footage emerged from inside the main hospital in Bergamo in Northern Italy at the start of the COVID‐19 pandemic.1 While Australia was spared the horror of that reality, the need to ration finite health resources is a perennial problem that confronts all health care systems. Health technology assessment (HTA) is a formal multidisciplinary process that aims to “inform decision‐making in order to promote an equitable, efficient, and high‐quality health system”.2 This article uses a case study approach to examine the role of HTA in the introduction of disruptive technology into the Australian health care system. It identifies structural problems in Australia's current approach that prevent HTA from achieving its equity objective.
Transcatheter aortic valve implantation: a paradigm shift in the management of aortic stenosis
Aortic stenosis is the most common form of valvular heart disease. It usually has a long asymptomatic phase, but once a patient develops symptoms, typically in their 70s or 80s, their prognosis without intervention is poor. Historically, the only effective treatment for aortic stenosis was surgical aortic valve replacement (SAVR). However, a significant proportion of afflicted patients were either unfit or unwilling to undergo open heart surgery, often simply because of their advanced age and associated frailty. It was the unmet needs of this group of patients that drove the development of the less invasive transcatheter aortic valve implantation (TAVI) procedure, which is usually performed via the femoral artery.3 Since the first‐in‐man implant in France in 2002, TAVI has displaced SAVR as the procedure of choice for progressively younger and healthier patient cohorts. The current point of equipoise in Australia is the 75–79‐year‐old cohort (Box 1).4
Both procedures are considered safe, clinically effective, and cost‐effective.5,6 While TAVI valves cost more than SAVR valves, the overall cost of implanting TAVI valves is less than the overall cost of performing SAVR.7,8,9 The long term (> 10 years) durability of TAVI is yet to be proven, whereas the long term durability of SAVR is well established.5,6
Access to TAVI in 2024
In both the public and private sector, access to TAVI requires prior approval by a multidisciplinary heart team. “Who should get the last TAVI valve?” is an ethical dilemma that heart teams at many state‐run public hospitals routinely grapple with. Unlike the ventilator scenario, where demand exceeds physical supply, this is purely a case of economic rationing, where demand exceeds available funding. For paternalistic and utilitarian clinicians, the decision can seem straightforward. But for clinicians who believe in patient autonomy and egalitarianism, or who are at least used to applying the rule of rescue, choosing between individual patients is an uncomfortable role. For patients who are denied access to TAVI, the consequences of the heart team's decision play out over time. Older, more comorbid patients must come to terms with being denied their only therapeutic treatment option. Younger, less comorbid patients must come to terms with being denied their preferred treatment option.
In contrast, all patients with appropriate private health insurance (gold and silver policy holders) are guaranteed access to federally subsidised TAVI. This difference in access explains the disproportionately high rate of private TAVI (Box 2). Based on the level of public activity that would have been required to normalise the rate of private TAVI to that of private SAVR, 1440 public patients were unable to access TAVI in 2021–2022 (author's estimate).4,10
The federal–state divide
In Australia, public–private access gaps are typically attacked and defended along ideological lines. Such arguments are a red herring. These gaps are, for the most part, an unintended consequence of Australia being a federation of states, not a unitary state. Or more specifically, the fact that under our constitutional arrangements and inter‐governmental agreements, state governments have direct responsibility for public hospital activity while the federal government has indirect responsibility for private hospital activity.13,14 It is inevitable with two levels of government making decisions independent of each other that inconsistencies will arise, especially if the fiscal (or political) implications of a given decision are likely to affect one level of government differently from the other level of government. This problem is compounded by the significant vertical fiscal imbalance that exists between these two levels of government, which makes the state governments dependent on a complex series of agreements that control transfer payments from the federal government to state governments.14
HTA in Australia is dominated by two highly respected federal committees, the Medical Services Advisory Committee (MSAC) and the Pharmaceutical Benefits Advisory Committee. MSAC advises the federal health minister directly on whether new services should be listed on the Medicare Benefits Schedule (MBS), and thus subsidised by the federal government. It should come as no surprise that when MSAC undertakes HTAs, it considers value for money and affordability from the perspective of the federal government.
When a new procedure that requires hospitalisation is added to the MBS, it creates a legal obligation on the federal government and third party payers (such as private health insurance companies) to contribute to the cost of the service for patients who elect to be treated as a private patient when they undergo that procedure.15 It does not, however, create an obligation on state governments to provide that procedure in public hospitals.16 Moreover, once a procedure is listed on the MBS, there is no mechanism by which the federal government can limit the number of private patients who can undergo the procedure. In contrast, state governments can limit activity in public hospitals by imposing caps on specific procedures.16 This is the situation we find ourselves in with TAVI.
How has Australia's approach to HTA contributed to inequitable access to TAVI?
TAVI has been performed in Australia since 200817 but Therapeutic Goods Administration approval, which is a prerequisite for MSAC consideration, was not obtained until 2013. In the absence of system level HTA guidance, early TAVI adopters were forced to rely on ad hoc institutional funding to establish programs in both public and private hospitals. The lack of coordination during this early phase has led to entrenched variations in activity between local health districts (LHDs), which equate to geographical variations in access.18
Between 2014 and 2021, MSAC considered, and ultimately supported, industry‐initiated applications for federal funding of TAVI for private patients whose risk of death following SAVR had been assessed as being either prohibitive/high,19 intermediate,7,8 or low.9 The federal health minister accepted MSAC's advice on each occasion. Corresponding item numbers were added to the MBS in November 2017, March 2022, and July 2022, respectively. Unsurprisingly, these federal HTAs had no immediate impact at the state level. New South Wales, for example, did not establish its High‐risk TAVI Supra‐LHD Service for prohibitive/high risk patients (which remains underfunded) until June 202120 and is yet to extend access to intermediate and low risk patients.
Notably, some of these applications claimed, and MSAC did not contest, that performing TAVI rather than SAVR in intermediate and low risk patients was more efficient in both private and public hospitals.7,9 This claim highlights the importance of understanding the funder's perspective in HTA, and how that influences HTA‐informed decision making. Reduced length of hospital stay is pivotal to TAVI's cost‐efficiency claim. In the private sector, these savings are real because third party payers do not have to pay the private hospital operators for as many bed days. But in the public sector, these savings are only theoretical because the state government invariably continues to pay for the bed. Indeed, caring for the patients to whom the bed days are reallocated may lead to a net increase in state government expenditure.
How can HTA bridge the federal–state divide?
The need for a nationally cohesive or federated approach to HTA is recognised in the National Health Reform Agreement as one of six key long term health reforms.16 However, the current Roadmap does not go far enough.21 It mistakenly conceives of HTA as an abstract process that should deliver consistent results when HTA is a contextual process that is dependent on the funder's perspective and their health care system's cost structure. If the existing fragmented approach to HTA is preserved, as planned, and the state and federal governments continue to make decisions independent of each other, the introduction of new technology will continue to be compromised by public–private access gaps.
Australia needs a truly national body that can undertake HTA from the perspectives of both the state and federal governments. It needs to be proactive, using HTA as a facilitator for the introduction of new technology rather than a barrier. It should provide its advice to both state and federal health ministers in a form that can support joint decision making in intergovernmental fora. It is only through unified advice that policy makers can understand the differing implications of providing government funding for new technology in both the public and private health care systems. It is only through joint decision making that accounts for these differences that policy makers can develop implementation strategies that guarantee equitable access to new technology.
Box 1 – Annual procedural volumes for surgical aortic valve replacement (SAVR) and transcatheter aortic valve implantation (TAVI), by age cohorts from 2012–13 to 2021–224
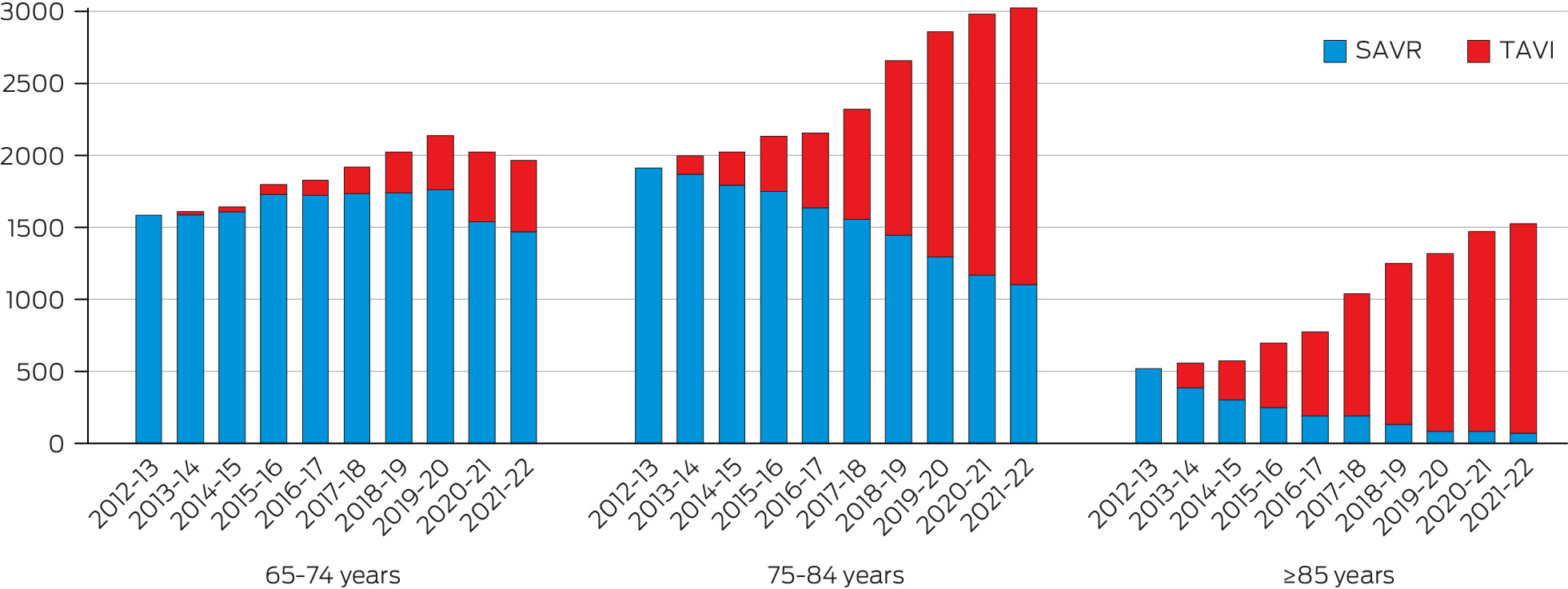
In clinical practice, TAVI is both a substitute treatment (for SAVR eligible patients) and a new treatment (for SAVR ineligible patients). This has resulted in a decrease in the number of SAVR procedures but an increase in the total number of aortic valve procedures.
Box 2 – Private activity as a percentage of total activity, by age cohorts in 2021–224,10
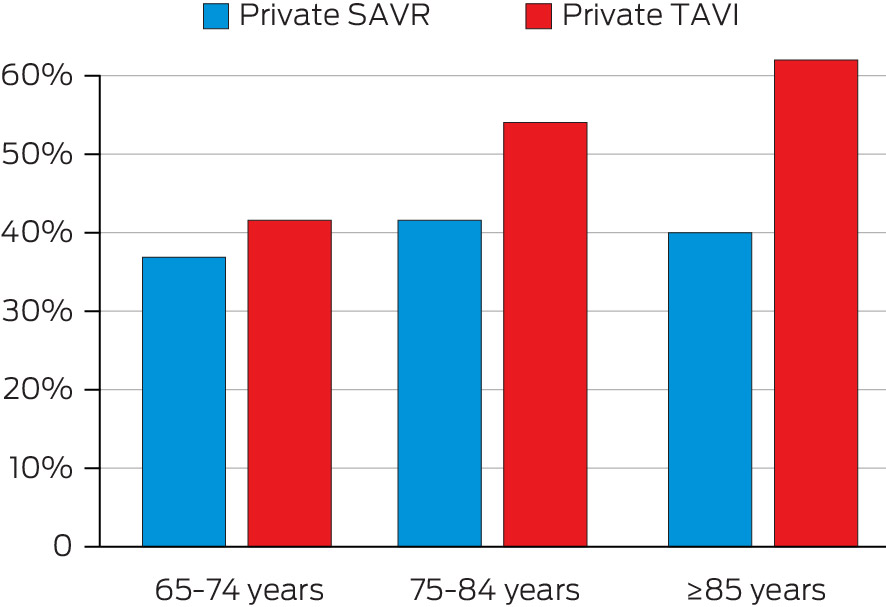
SAVR = surgical aortic valve replacement; TAVI = transcatheter aortic valve implantation.Private patients are over‐represented among patients undergoing TAVI, relative to SAVR. This observation is maximal beyond 85 years of age despite the participation rate for private health insurance declining significantly in this age group.11,12 Contemporary data for SAVR is consistent with historical data for all surgical heart valve replacements (annual mean from 2000–01 to 2021–22, 40% ± 2%).4,10
Provenance: Not commissioned; externally peer reviewed.
- 1. Ramsay S. The shocking centre of the COVID‐19 crisis [video]. Sky News, 20 Mar 2020. https://www.youtube.com/watch?v=_J60fQr0GWo (viewed Apr 2023).
- 2. O'Rourke B, Oortwijn W, Schuller T, et al. The new definition of health technology assessment: a milestone in international collaboration. Int J Technol Assess Health Care 2020; 36: 187‐190.
- 3. Cribier A. Development of transcatheter aortic valve implantation (TAVI): a 20‐year odyssey. Arch Cardiovasc Dis 2012; 105: 146‐152.
- 4. Australian Institute of Health and Welfare. Data cubes. Procedures and healthcare interventions (ACHI 11th edition), Australia, 2021‐22. https://www.aihw.gov.au/reports/hospitals/procedures‐data‐cubes/contents/data‐cubes (viewed July 2023).
- 5. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease. J Am Coll Cardiol 2021; 77: e25‐e197.
- 6. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 2022; 43: 561‐632.
- 7. Medical Services Advisory Committee. 1603 – Transcatheter aortic valve implantation (TAVI) via transfemoral delivery, using the SAPIEN 3 balloon‐expandable valve system balloon‐expandable valve (BEV) system, for patients at intermediate risk for surgery. Last updated 17 Feb 2021. http://www.msac.gov.au/internet/msac/publishing.nsf/Content/1603‐public (viewed Apr 2023).
- 8. Medical Services Advisory Committee. 1652 – Transcatheter aortic valve implantation via transfemoral delivery for patients at intermediate risk for surgery. Last updated 8 June 2021. http://www.msac.gov.au/internet/msac/publishing.nsf/Content/1652‐public (viewed Apr 2023).
- 9. Medical Services Advisory Committee. 1640 – Transcatheter aortic valve implantation via transfemoral delivery for patients at low risk for surgery. Last updated 29 Sept 2021. http://www.msac.gov.au/internet/msac/publishing.nsf/Content/1640‐public (viewed Apr 2023).
- 10. Services Australia. Medicare item reports. http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp (viewed Apr 2023).
- 11. Australian Prudential Regulation Authority. Quarterly private health insurance statistics. March 2023. https://www.apra.gov.au/quarterly‐private‐health‐insurance‐statistics (viewed July 2023).
- 12. Australian Bureau of Statistics. National, state and territory population. Data downloads – data cubes: Population by age and sex ‐ national. Reference period June 2022. https://www.abs.gov.au/statistics/people/population/national‐state‐and‐territory‐population/jun‐2022 (viewed July 2023).
- 13. Boxall A‐M, Gillespie JA. Making Medicare: the politics of universal health care in Australia. Sydney: UNSW Press, 2013.
- 14. Twomey A, Withers G. Federalist paper 1: Australia's federal future. Council for the Australian Federation, 2007. https://www.caf.gov.au/__data/assets/pdf_file/0011/976943/AustraliasFederalFuture‐1.pdf (viewed Sept 2023).
- 15. Private Health Insurance Act 2007 (Cth). https://www.legislation.gov.au/Details/C2023C00107 (viewed Sept 2023).
- 16. Australian Government. Addendum to National Health Reform Agreement 2020 – 2025. https://federalfinancialrelations.gov.au/sites/federalfinancialrelations.gov.au/files/2021‐07/NHRA_2020‐25_Addendum_consolidated.pdf (viewed Apr 2023).
- 17. Muller D, Baron D, Roy P. Percutaneous management of aortic valve stenosis. St Vincent's Clinic, Sydney: Proceedings, Vol. 17, No. 1, Dec 2009; pp. 8‐11.
- 18. Lee AH, Ng AC, Yong AS. Outcomes of 1098 patients following transcatheter aortic valve implantation: a statewide population‐linkage cohort study [supplementary data]. Heart Lung Circ 2021; 30: 1213‐1220.
- 19. Medical Services Advisory Committee. 1361.2 – Transcatheter aortic valve implantation via transfemoral or transapical delivery (resubmission). Last updated 13 Feb 2019. http://www.msac.gov.au/internet/msac/publishing.nsf/Content/1361.2‐public (viewed Apr 2023).
- 20. Perrottet D, Hazzard B. $21.6 million to build specialist cardiac capacity for patients across NSW [media release]. 21 June 2021. https://www.treasury.nsw.gov.au/sites/default/files/2021‐06/Dominic%20Perrottet%20Brad%20Hazzard%20med%20rel%20‐%20%2421.6%20million%20Budget%20boost%20to%20cardiac%20support%20for%20patients%20across%20NSW.pdf (viewed Apr 2023).
- 21. Australian Health Ministers. National Health Reform Agreement (NHRA) Long‐term Health Reforms Roadmap. 2021. https://www.health.gov.au/sites/default/files/documents/2021/10/national‐health‐reform‐agreement‐nhra‐long‐term‐health‐reforms‐roadmap_0.pdf (viewed Apr 2023).






Open access:
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
No relevant disclosures.