The known: Sexual abuse during childhood has been linked with greater risks of mental illness, health risk behaviour, and negative social outcomes. Its relationship with premature mortality, apart from suicide, has not been as thoroughly investigated.
The new: Rates of all‐cause, internal cause, and external cause mortality into mid‐adulthood were higher among Victorians who had been sexually abused as children than for the general population. External cause mortality rates were particularly high for people who had experienced penetrative sexual abuse.
The implications: Sexual abuse of children and its sequelae may contribute to potentially avoidable deaths later in life. Preventing sexual abuse and supporting those who experience it is essential not only for the child, but also for the adult they become.
Sexual abuse of children is a preventable public health problem with devastating consequences. In a recent Australian survey, 37.3% of women and 18.8% of men reported they had experienced sexual abuse as children, and 12.5% of women and 4.3% of men reported penetrative abuse.1 The grave psychological and often physical violations make sexual abuse during childhood a risk factor for a range of mental disorders throughout life.2,3 It is also associated with lower socio‐economic attainment, drug and alcohol misuse, violence (both as victim and perpetrator), self‐harm and attempted suicide, and physical health problems.3,4,5,6,7 Although these factors increase the risk of early death, the association between sexual abuse during childhood and mortality has not been examined in detail.
Several studies have investigated associations between mortality risk in later life and negative childhood experiences, contact with child protection services, or early exposure to violence.8,9,10,11,12 These studies have generally found that mortality risk is higher for people with such experiences, after adjusting for socio‐demographic, economic, and other family‐related factors. One study found no difference in death rates into young adulthood between people who had experienced documented childhood abuse or neglect and matched controls.13 Although people who have experienced sexual abuse are often included in such studies, separate mortality rates are rarely reported, despite evidence that it is a maltreatment type with unique effects and especially strong associations with several health risks.6,14
The relationship between sexual abuse during childhood and suicide risk has been investigated.14,15 A meta‐analysis of longitudinal studies found that sexual abuse during childhood and bullying were leading violence‐related contributors to suicide attempts by adolescents and young adults.12 In the only longitudinal study to examine child sexual abuse and all‐cause mortality into mid‐adulthood, sexual abuse was the strongest independent predictor of premature death.16 However, the study assessed sexual abuse history with a single retrospective self‐report survey item, restricted consideration to deaths of people aged 44–58 years, and did not report cause‐specific findings.
We compared mortality in an historical cohort of 2759 people who had experienced medically assessed child sexual abuse in Victoria with that of the general population. The study extends an earlier examination of rates of unnatural death (suicide and fatal drug overdose) in the same group during 1991–200815 by examining all‐cause, external cause (eg, suicide, accident, assault), and internal cause (eg, cardiovascular disease, cancer) mortality, extending the follow‐up period, undertaking a more sophisticated comparison with population mortality rates, and separately estimating mortality rates for people who experienced penetrative or non‐penetrative sexual abuse.
Methods
We undertook an historical cohort study of 2759 people who had experienced medically assessed contact sexual abuse in Victoria while aged 16 years or younger during 1964–1995. We analysed data from three statutory datasets.
Victorian Institute of Forensic Medicine (VIFM)
Until 2006, the Victorian Institute of Forensic Medicine (https://www.vifm.org) was responsible for forensic medical examinations of Victorian children following allegations of sexual abuse reported to the police or child protection services. In an earlier study, a database including details for all 2759 cases of contact sexual abuse of Victorian children aged 16 years or younger and medically examined during 1964–1995 (558 boys, 20.2%; 2201 girls, 79.8%), was constructed from the VIFM records.17 Available information included full name, birth date, sex, medical examination date, and physicians’ conclusion about whether penetration of an orifice had occurred.
National Death Index (NDI)
Deaths of people in the 1964–1995 cohort during 1 January 1980 – 31 May 2020 were identified by data linkage with the Australian Institute of Health and Welfare (AIHW) National Death Index. The NDI contains person‐level records for all deaths in Australia since 1980, including fact of death, date of death, and underlying cause of death as International Classification of Diseases, ninth revision (ICD‐9; deaths before 1997) or tenth revision (ICD‐10; deaths from 1997) codes.18 The AIHW undertook probabilistic data linkage based on full name, birth date, and sex, and provided the data to the investigators on 1 September 2020.
General Record of Incidence of Mortality (GRIM)
General Record of Incidence of Mortality books — population‐level datasets including information for all registered deaths19 — were provided by the AIHW. At the time of our request (18 March 2021), GRIM data for deaths of Victorian residents during 1980–2019 were available, including death numbers and rates, population numbers by age (five‐year brackets), and year of death. Actual year of death was used for deaths prior to 2019; year of death registration was used for deaths in 2019. Year of death registration was used for 2019 because actual year of death may take time to be registered, which would result in undercounting deaths for the most recent year.
Statistical analysis
Causes of death were categorised as all causes, external causes (ICD‐10 codes V01–Y98), and internal causes (ICD‐10 codes A00–R99), as in similar studies.20,21 Cell sizes smaller than five were avoided by aggregation or cell suppression.
We separately compared all‐cause, internal cause, and external cause mortality rates by age group for people who were sexually abused during childhood with that for the general population. The denominator for mortality rates for people who had experienced sexual abuse during childhood was the number of living people in this group, by age category. Sex‐ and age‐standardised mortality ratios were estimated (95% confidence intervals [CIs] estimated using Wilson's method22) with respect to the mortality rate for the general population. Numbers of excess deaths were estimated by calculating the expected number of deaths for people who experienced sexual abuse during childhood, based on the rate in the general population, and subtracting this number from the observed number of deaths.
We compared mortality rates for people who had experienced sexual abuse during childhood with those of the general Victorian population in Poisson and quasi‐Poisson inferential models, with population number as an offset term; quasi‐Poisson models were used when overdispersion of errors was apparent. Two sets of models were constructed: the first examined differences between people sexually abused during childhood and the general population in age‐ and sex‐adjusted all‐cause, internal, and external cause mortality; the second examined the same outcomes, but included sexual abuse type (penetrative or non‐penetrative) as a term. An interaction term for sex was tested in each model; as its influence on mortality was not statistically significant, it was not included in the final models. For our main analyses, the reference year for estimating population mortality rates was 2001 (middle of the NDI coverage period). To examine whether the choice of reference year influenced our results, we also constructed models with 1980 or 2019 as the reference year. We report incidence rate ratios (IRRs) with 95% CIs. Statistical analyses were conducted in RStudio 2022.12.0 + 353 and R 4.2 (R Foundation for Statistical Computing).
Ethics approval
The AIHW ethics committee (EO2015/3/191) and Swinburne University human research ethics committee (2015/232) approved the study and waived the requirement for individual consent by cohort members.
Results
Of the 2759 people sexually abused as children during 1964–1995, 153 had died during 1980–2020 (5.5%). Thirty‐eight people were aged 50 years or more at the time of death (fewer than five men aged 50–54 years, and none over 54 years of age); to facilitate more robust age‐ and sex‐based comparisons, we restricted our analysis to the 115 deaths of people under 50 years of age (4.2% of sample; 79 women, 36 men), including 56 deaths with external and 56 with internal causes (cause of death information missing in three cases). The most frequent causes of death were accidents or assault (32 cases), suicide (24 cases), cancers (13 cases), and circulatory diseases (11 cases); mean age at death was 33.1 years (standard deviation, 9.6 years; range, 6–49 years) (Box 1).
In each age group from 15–19 years, the mortality rates for men and women sexually abused as children were higher than for the general population (Box 2). Similar differences were evident using different reference years for estimating population mortality rates (Supporting Information, figures 1 and 2).
Age‐ and sex‐standardised all‐cause mortality ratios (people who were sexually abused as children v general population) were highest for people aged 25–29 years (men: 16.5; 95% CI, 11.0–22.0; women: 19.2; 95% CI, 14.3–24.2) (Box 3). These values correspond to eight excess deaths of men (excess risk, 1532 excess deaths per 100 000 men) and fourteen of women (excess risk, 651 excess deaths per 100 000 women). Standardised mortality ratios were generally lower using 1980 as the general population reference year, and higher using 2019 as the reference year (exception: for external cause deaths of women aged 40 years or more and men aged 35 years or more), but the distributions were similar to those in the main analysis (Supporting Information, tables 2 and 3).
The age‐ and sex‐adjusted mortality rate for people sexually abused as children was higher than for the general population for all‐cause (IRR, 8.25; 95% CI, 5.92–11.5), internal cause (IRR, 5.92; 95% CI, 3.89–9.01), and external cause deaths (IRR, 12.6; 95% CI, 9.61–16.6) (Box 4). Using 1980 as the reference year for estimating population mortality rates, the IRRs were 3.47 (95% CI, 2.04–5.92) for internal cause and 8.71 (95% CI, 6.24–12.2) for external cause deaths; using 2019 as the reference year, the IRRs were 8.70 (95% CI, 5.88–12.9) for internal cause and 17.1 (95% CI, 13.0–22.5) for external cause deaths (Supporting Information, tables 4 and 5).
Compared with the general population, age‐ and sex‐adjusted all‐cause mortality was higher for both people who had experienced penetrative sexual abuse (IRR, 8.90; 95% CI, 6.41–12.4) and for those who had experienced non‐penetrative sexual abuse as children (IRR, 7.08; 95% CI, 4.34–11.6). For external cause deaths, the rate relative to the general population was higher for people who experienced penetrative sexual abuse (IRR, 14.9; 95% CI, 10.9–20.5) than for those subjected to non‐penetrative sexual abuse (IRR, 8.92; 95% CI, 5.35–14.9) (Box 5). Using 1980 or 2019 as alternative reference years for estimating population mortality rates yielded similar results (Supporting Information, tables 6 and 7).
Discussion
Based on deaths data for the period 1980–2020, we found that rates of all‐cause, internal cause, and external cause mortality were higher for people who had experienced medically assessed sexual abuse as children in Victoria during 1964–1995 than for the general population. Age‐ and sex‐standardised all‐cause mortality ratios were largest for men and women aged 25–29 years, which suggests that early adulthood is a period of particular vulnerability for people sexually abused during childhood, consistent with other reports.11 The age‐ and sex‐adjusted all‐cause mortality rate was more than eight times as high among people who had been sexually abused as in the general population; the difference in external cause mortality was larger for people who had experienced penetrative sexual abuse than for those who experienced non‐penetrative abuse.
Although an association between child sexual abuse and suicide risk is recognised,12 the association with deaths attributed to other external causes into middle adulthood has not been investigated. One‐half of the deaths in our study were caused by accidents (eg, accidental poisoning, vehicular accidents, drowning), suicide, or assault, consistent with reports that link child sexual abuse with increased risk of self‐harm, attempted suicide, substance misuse, and involvement in violence.3,4,7,12,15 Our finding that the rate of external cause mortality was even higher among people who had endured penetrative abuse is consistent with reports of a dose–response association between sexual abuse and poorer long term adjustment.14 Risk of mental illness is higher among people who have experienced sexual abuse involving penetration,17 and mental illnesses are important risk factors for suicide.23
Our study is the first to find that rates of death from internal causes (such as cancers, circulatory and respiratory system diseases, and mental and behavioural disorders) are higher for people who suffered sexual abuse as children. Longitudinal study findings suggest causal links between sexual abuse during childhood and mental disorders,2 socio‐economic disadvantage,5 and health risk behaviours,3 which in turn increase morbidity and mortality. Accelerated biological ageing of children who have experienced trauma may also be involved in increased risks of disease and early death,24 but this possibility requires further investigation.
Limitations
Our statistical analyses were adjusted for age and sex, but unmeasured factors, including other forms of maltreatment, other adversity, and socio‐economic disadvantage, could influence statistical associations between sexual abuse and mortality. As poverty and other maltreatment are not as closely associated with sexual abuse in Australia as with other forms of maltreatment,25,26,27 however, these factors are unlikely to fully explain the associations we found. Reports that associations between child sexual abuse and mental health problems,2,3 health risk behaviours,6 and mortality16 persist after controlling for a range of socio‐economic and other factors are broadly consistent with a causal contribution of childhood trauma to adverse health outcomes.2,28 However, our study design precluded drawing conclusions about causal relationships, which would require quasi‐experimental and prospective longitudinal studies.
We may have underestimated the number of deaths of people who experienced sexual abuse during 1964–1995, as we did not have mortality data for the period 1964–1980. Further, we compared mortality rates with those for the general Victorian population, a proportion of whom will themselves have experienced sexual abuse. The relatively small number of deaths precluded examining more cause‐specific mortality. Finally, the people in our study had been subjected to medically assessed contact sexual abuse between the 1960s and 1990s; further, they had frequently experienced more severe levels of abuse. For example, 63% of people in our study experienced penetrative abuse, while 36.6% of participants in a recent Australian survey who reported contact sexual abuse had experienced forced intercourse.1 The medical examination and subsequent social welfare or judicial involvement could have exacerbated the harm of abuse or triggered interventions that mitigated its impact. Our findings may consequently not be generalisable to people who experienced sexual abuse more recently, or to cases in which sexual abuse was not reported to authorities or was non‐contact sexual abuse.
Conclusion
Our findings suggest that exposure to sexual abuse during childhood may be a risk marker that identifies people at greater risk of premature death. Preventing child sexual abuse and intervening early to reduce the damage it inflicts is not only essential for the welfare of the child, but could also help avert avoidable deaths later in life.
Box 1 – Characteristics and causes of death of people who were sexually abused in Victoria aged 16 years or younger during 1964–1995
|
Characteristic |
All people |
Girls/Women |
Boys/Men |
||||||||||||
|
|
|||||||||||||||
|
People who were sexually abused |
2759 |
2201 |
558 |
||||||||||||
|
Type of sexual abuse during childhood |
|
|
|
||||||||||||
|
Penetrative |
1737 (63.0%) |
1429 (64.9%) |
308 (55.2%) |
||||||||||||
|
Non‐penetrative |
1022 (37.0%) |
772 (35.1%) |
250 (44.8%) |
||||||||||||
|
Age at abuse medical examination (years), mean (SD) |
10.2 (4.4) |
10.4 (4.5) |
9.4 (4.2) |
||||||||||||
|
Deaths before age of 50 years (1980–2020) |
115 (4.2%) |
79 (3.6%) |
36 (6.4%) |
||||||||||||
|
Age at death (years), mean (SD) |
33.1 (9.6) |
33.0 (10.0) |
33.1 (9.3) |
||||||||||||
|
Cause of death (ICD‐10 codes)* |
|
|
|
||||||||||||
|
External (V01–Y98) |
56 (2.0%) |
37 (1.7%) |
19 (3.4%) |
||||||||||||
|
Internal (A00–R99) |
56 (2.0%) |
41 (1.9%) |
15 (2.7%) |
||||||||||||
|
External causes of death |
|
|
|
||||||||||||
|
Accidents/assault (V01–X59, X85–Y09) |
32 (1.2%) |
24 (1.1%) |
8 (1.4%) |
||||||||||||
|
Suicide (X60–X84) |
24 (0.9%) |
13 (0.6%) |
11 (2.0%) |
||||||||||||
|
Internal causes of death |
|
|
|
||||||||||||
|
Cancers (C00–D48) |
13 (0.5%) |
† |
† |
||||||||||||
|
Circulatory diseases (I00–I99) |
11 (0.4%) |
† |
† |
||||||||||||
|
Mental and behavioural disorders (F00–F99) |
7 (0.2%) |
† |
† |
||||||||||||
|
Respiratory system diseases (J00–J99) |
5 (0.2%) |
† |
† |
||||||||||||
|
Nervous system diseases/endocrine diseases (G00–G99, E00–E90) |
7 (0.2%) |
† |
† |
||||||||||||
|
Infectious diseases/digestive system diseases (A00–B99, K00–K93) |
5 (0.2%) |
† |
† |
||||||||||||
|
Other‡ |
8 (0.3%) |
† |
† |
||||||||||||
|
|
|||||||||||||||
|
ICD‐10 = International Classification of Diseases, tenth revision; SD = standard deviation. * Causes of death prior to 1997 were recorded using ICD‐9 codes that we have converted to ICD‐10 codes for this table. Cause of death information was not available for three people. † Cells suppressed, as value for at least one cell in row was less than five. ‡ Included causes coded as D50–D89, Q00–Q99, R56. |
|||||||||||||||
Box 2 – Mortality rates (with 95% confidence intervals), for people sexually abused as children in Victoria (1964–1995) who died before the age of 50 years (1980–2020) and for the general Victorian population (reference year: 2001), by cause of death type, sex, and age group*
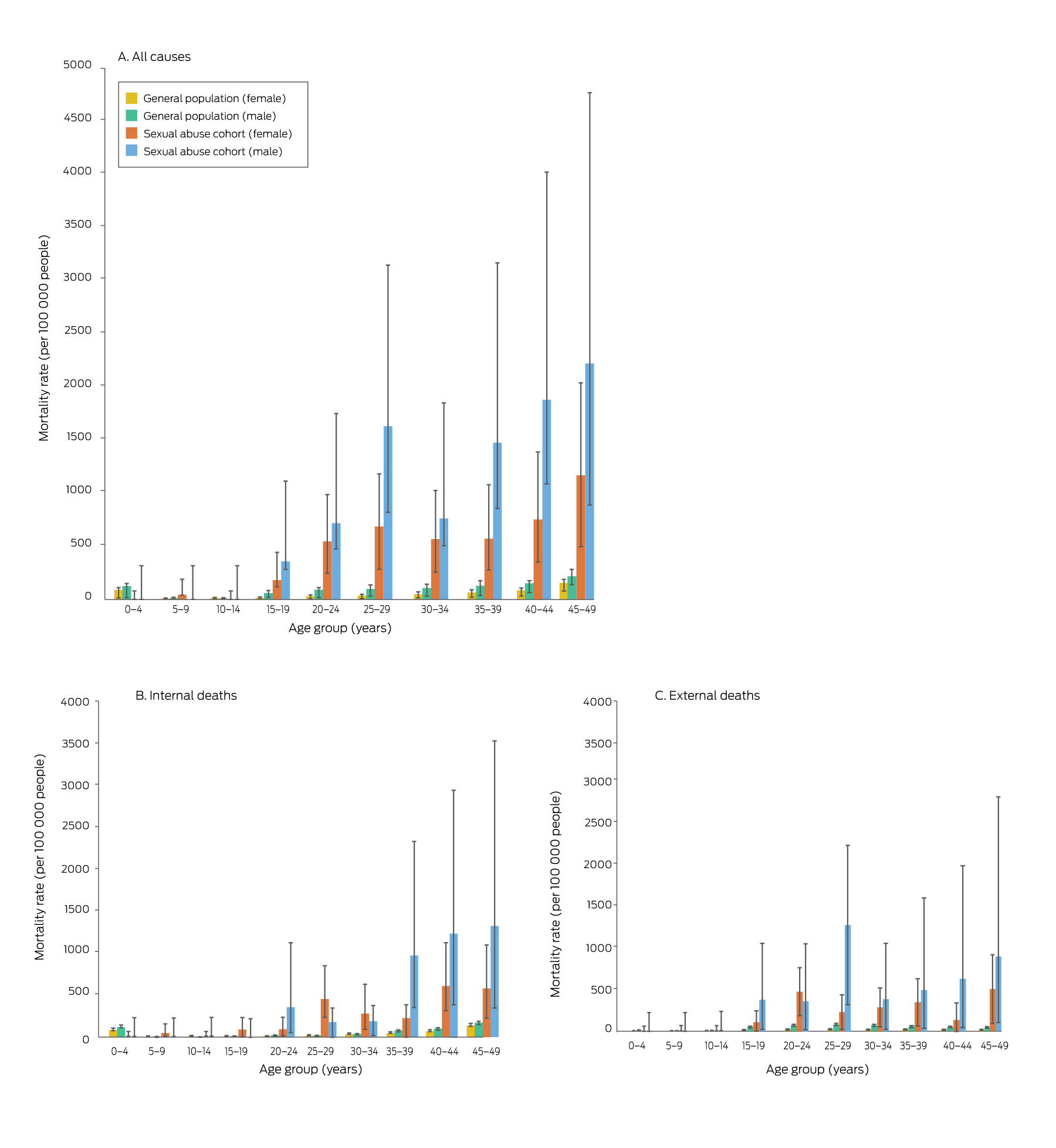
* The data for this graph are including in the Supporting Information, table 1.
Box 3 – Age‐ and sex‐standardised mortality ratios (with 95% confidence intervals) for people sexually abused as children in Victoria (1964–1995) who died before the age of 50 years (1980–2020) compared with the general Victorian population (reference year: 2001), by cause of death type
|
|
All cause |
Internal cause |
External cause |
||||||||||||
|
Age group (years) |
Girls/Women |
Boys/Men |
Girls/Women |
Boys/Men |
Girls/Women |
Boys/Men |
|||||||||
|
|
|||||||||||||||
|
0–4 |
0 |
0 |
0 |
0 |
0 |
0 |
|||||||||
|
5–9 |
5.5 (0.0–11.0) |
0 |
8.0 (0.0–15.9) |
0 |
0 |
0 |
|||||||||
|
10–14 |
0 |
0 |
0 |
0 |
0 |
0 |
|||||||||
|
15–19 |
10.3 (5.2–15.5) |
5.9 (1.7–10.1) |
16.0 (4.7–27.4) |
0 |
7.6 (2.2–13.0) |
7.7 (2.3–13.2) |
|||||||||
|
20–24 |
17.4 (12.4–22.4) |
8.1 (4.1–12.2) |
6.6 (1.9–11.2) |
17.8 (5.2–30.3) |
25.9 (17.7–34.0) |
5.3 (1.6–9.0) |
|||||||||
|
25–29 |
19.2 (14.3–24.2) |
16.5 (11.0–22.0) |
29.9 (20.4–39.4) |
9.2 (0.0–18.4) |
11.2 (6.2–16.2) |
16.0 (10.0–22.0) |
|||||||||
|
30–34 |
11.1 (7.9–14.3) |
7.1 (3.5–10.6) |
8.3 (4.9–11.7) |
4.8 (0.0–9.7) |
16.8 (10.0–23.7) |
5.6 (1.6–9.5) |
|||||||||
|
35–39 |
8.8 (6.0–11.6) |
11.2 (6.6–15.8) |
4.9 (2.4–7.4) |
12.6 (6.3–18.9) |
18.8 (11.1–26.5) |
9.2 (2.7–15.8) |
|||||||||
|
40–44 |
8.9 (6.2–11.6) |
12.4 (7.3–17.5) |
8.8 (5.9–11.7) |
12.1 (6.0–18.1) |
9.3 (2.7–15.8) |
13.1 (3.8–22.4) |
|||||||||
|
45–49 |
7.5 (5.5–9.5) |
10.2 (5.7–14.8) |
4.2 (2.6–5.8) |
7.6 (3.2–12.1) |
32.2 (19.1–45.4) |
20.8 (6.1–35.4) |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 4 – Age‐ and sex‐adjusted mortality among people sexually abused as children in Victoria (1964–1995) who died before the age of 50 years (1980–2020) compared with the general Victorian population (reference year: 2001): incident rate ratios with 95% confidence intervals*
|
Characteristic |
All cause |
Internal cause |
External cause |
||||||||||||
|
|
|||||||||||||||
|
Sexual abuse as child |
8.25 (5.92–11.5) |
5.92 (3.89–9.01) |
12.6 (9.61–16.6) |
||||||||||||
|
Sex (male) |
1.84 (1.59–2.12) |
1.38 (1.19–1.60) |
3.27 (2.83–3.78) |
||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
0–4 |
1 |
1 |
1 |
||||||||||||
|
5–9 |
0.11 (0.06–0.19) |
0.09 (0.05–0.16) |
0.40 (0.17–0.91) |
||||||||||||
|
10–14 |
0.10 (0.05–0.18) |
0.06 (0.03–0.12) |
0.75 (0.38–1.48) |
||||||||||||
|
15–19 |
0.38 (0.27–0.54) |
0.10 (0.05–0.16) |
4.98 (3.05–8.13) |
||||||||||||
|
20–24 |
0.60 (0.45–0.82) |
0.18 (0.12–0.28) |
7.63 (4.73–12.3) |
||||||||||||
|
25–29 |
0.69 (0.52–0.92) |
0.20 (0.14–0.30) |
8.76 (5.46–14.1) |
||||||||||||
|
30–34 |
0.78 (0.60–1.03) |
0.38 (0.28–0.52) |
7.39 (4.60–11.9) |
||||||||||||
|
35–39 |
0.97 (0.75–1.26) |
0.64 (0.49–0.84) |
6.35 (3.92–10.3) |
||||||||||||
|
40–44 |
1.17 (0.91–1.50) |
0.91 (0.71–1.15) |
5.45 (3.35–8.85) |
||||||||||||
|
45–49 |
1.84 (1.46–2.33) |
1.61 (1.29–2.01) |
5.37 (3.29–8.76) |
||||||||||||
|
|
|||||||||||||||
|
* All‐cause and internal cause deaths: quasi‐Poisson models; external cause deaths: Poisson model. |
|||||||||||||||
Box 5 – Age‐ and sex‐adjusted mortality among people sexually abused as children in Victoria (1964–1995) who died before the age of 50 years (1980–2020) compared with the general Victorian population (reference year: 2001), including term for type of abuse (penetrative or non‐penetrative): incident rate ratios with 95% confidence intervals*
|
Characteristic |
All cause |
Internal cause |
External cause |
||||||||||||
|
|
|||||||||||||||
|
Sexual abuse as child |
|
|
|
||||||||||||
|
Non‐penetrative |
7.08 (4.34–11.6) |
5.87 (3.20–10.8) |
8.92 (5.35–14.9) |
||||||||||||
|
Penetrative |
8.90 (6.41–12.4) |
5.94 (3.83–9.22) |
14.9 (10.9–20.5) |
||||||||||||
|
Sex (male) |
1.84 (1.64–2.07) |
1.38 (1.21–1.56) |
3.28 (2.84–3.80) |
||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
0–4 |
1 |
1 |
1 |
||||||||||||
|
5–9 |
0.11 (0.06–0.17) |
0.09 (0.05–0.15) |
0.40 (0.17–0.91) |
||||||||||||
|
10–14 |
0.10 (0.06–0.16) |
0.06 (0.03–0.11) |
0.75 (0.38–1.48) |
||||||||||||
|
15–19 |
0.38 (0.28–0.51) |
0.10 (0.06–0.17) |
4.98 (3.05–8.13) |
||||||||||||
|
20–24 |
0.60 (0.47–0.78) |
0.18 (0.12–0.26) |
7.63 (4.73–12.3) |
||||||||||||
|
25–29 |
0.69 (0.55–0.88) |
0.20 (0.14–0.29) |
8.76 (5.46–14.0) |
||||||||||||
|
30–34 |
0.78 (0.63–0.98) |
0.38 (0.29–0.50) |
7.39 (4.60–11.9) |
||||||||||||
|
35–39 |
0.97 (0.78–1.20) |
0.64 (0.51–0.81) |
6.34 (3.93–10.2) |
||||||||||||
|
40–44 |
1.17 (0.95–1.44) |
0.91 (0.74–1.11) |
5.44 (3.35–8.83) |
||||||||||||
|
45–49 |
1.84 (1.51–2.24) |
1.61 (1.34–1.94) |
5.36 (3.29–8.74) |
||||||||||||
|
|
|||||||||||||||
|
* All‐cause and internal cause deaths: quasi‐Poisson models; external cause deaths: Poisson model. |
|||||||||||||||
Received 5 December 2022, accepted 29 June 2023
- Nina Papalia1,2
- Benjamin L Spivak1,2
- Linda Ashford1,2
- Ahona Guha2
- Stefan Luebbers1,2,3
- James RP Ogloff1,2
- Nina Papalia1,2
- Benjamin L Spivak1,2
- Linda Ashford1,2
- Ahona Guha2
- Stefan Luebbers1,2,3
- James RP Ogloff1,2
- 1 Centre for Forensic Behavioural Science, Swinburne University of Technology, Melbourne, VIC
- 2 Victorian Institute of Forensic Mental Health (Forensicare), Melbourne, VIC
- 3 Youth Forensic Specialist Services, Alfred Health, Melbourne, VIC
- 1 Centre for Forensic Behavioural Science, Swinburne University of Technology, Melbourne, VIC
- 2 Victorian Institute of Forensic Mental Health (Forensicare), Melbourne, VIC
- 3 Youth Forensic Specialist Services, Alfred Health, Melbourne, VIC
Open access:
Open access publishing facilitated by Swinburne University of Technology, as part of the Wiley ‐ Swinburne University of Technology agreement via the Council of Australian University Librarians.
This investigation was partly supported by research seed funding provided by Swinburne University of Technology (James Ogloff, Ahona Guha), an Australia Government Research Training Program stipend (Ahona Guha), and an Australian Research Council Early Career Researcher Award (DE220100147) (Nina Papalia). The funders had no role in the design, data collection, analysis or interpretation, reporting, or publication. We also acknowledge the assistance provided by the Australian Institute of Health and Welfare.
No relevant disclosures.
- 1. Mathews B, Pacella R, Scott JG, et al. The prevalence of child maltreatment in Australia: findings from a national survey. Med J Aust 2023; 218 (6 Suppl): S13‐S18. https://www.mja.com.au/journal/2023/218/6/australian‐child‐maltreatment‐study‐national‐prevalence‐and‐associated‐health
- 2. Baldwin JR, Wang B, Karwatowska L, et al. Childhood maltreatment and mental health problems: a systematic review and meta‐analysis of quasi‐experimental studies. Am J Psychiatry 2023; 180: 117‐126.
- 3. Fergusson DM, McLeod GFH, Horwood LJ. Childhood sexual abuse and adult developmental outcomes: findings from a 30‐year longitudinal study in New Zealand. Child Abuse Negl 2013; 37: 664‐674.
- 4. Papalia N, Mann E, Ogloff JRP. Child sexual abuse and risk of revictimization: impact of child demographics, sexual abuse characteristics, and psychiatric disorders. Child Maltreat 2021; 26: 74‐86.
- 5. Assini‐Meytin LC, Thorne EJ, Sanikommu M, et al. Impact of child sexual abuse on socioeconomic attainment in adulthood. J Adolesc Health 2022; 71: 594‐600.
- 6. Lawrence DM, Hunt A, Mathews B, et al. The association between child maltreatment and health risk behaviours and conditions throughout life in the Australian Child Maltreatment Study. Med J Aust 2023; 218 (6 Suppl): S34‐S39. https://www.mja.com.au/journal/2023/218/6/australian‐child‐maltreatment‐study‐national‐prevalence‐and‐associated‐health
- 7. Trauffer N, Widom CS. Child abuse and neglect, and psychiatric disorders in nonviolent and violent female offenders. Violence Gend 2017; 4: 137‐143.
- 8. Kelly‐Irving M, Lepage B, Dedieu D, et al. Adverse childhood experiences and premature all‐cause mortality. Eur J Epidemiol 2013; 28: 721‐734.
- 9. Rod NH, Bengtsson J, Budtz‐Jørgensen E, et al. Trajectories of childhood adversity and mortality in early adulthood: a population‐based cohort study. Lancet 2020; 396: 489‐497.
- 10. Palmer L, Prindle J, Putnam‐Hornstein E. A population‐based examination of suicide and child protection system involvement. J Adolesc Health 2021; 69: 465‐469.
- 11. Segal L, Armfield JM, Gnanamanickam ES, et al. Child maltreatment and mortality in young adults. Pediatrics 2021; 147: e2020023416.
- 12. Castellví P, Miranda‐Mendizábal A, Parés‐Badell O, et al. Exposure to violence, a risk for suicide in youths and young adults: a meta‐analysis of longitudinal studies. Acta Psychiatr Scand 2017; 135: 195‐211.
- 13. White HR, Widom CS. Does childhood victimization increase the risk of early death? A 25‐year prospective study. Child Abuse Negl 2003; 27: 841‐853.
- 14. Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse Negl 2008; 32: 607‐619.
- 15. Cutajar MC, Mullen PE, Ogloff JRP, et al. Suicide and fatal drug overdose in child sexual abuse victims: a historical cohort study. Med J Aust 2010; 192: 184‐187. https://www.mja.com.au/journal/2010/192/4/suicide‐and‐fatal‐drug‐overdose‐child‐sexual‐abuse‐victims‐historical‐cohort
- 16. Rogers NT, Power C, Pinto Pereira SM. Child maltreatment, early life socioeconomic disadvantage and all‐cause mortality in mid‐adulthood: findings from a prospective British birth cohort. BMJ Open 2021; 11: e050914.
- 17. Cutajar MC, Mullen PE, Ogloff JRP, et al. Psychopathology in a large cohort of sexually abused children followed up to 43 years. Child Abuse Negl 2010; 34: 813‐822.
- 18. Australian Institute of Health and Welfare. National Death Index (NDI). Updated 3 July 2023. https://www.aihw.gov.au/about‐our‐data/our‐data‐collections/national‐death‐index (viewed July 2023).
- 19. Australian Institute of Health and Welfare. General Record of Incidence of Mortality (GRIM) books. Updated 11 July 2023. https://www.aihw.gov.au/reports/life‐expectancy‐deaths/grim‐books/contents/data‐visualisation (viewed July 2023).
- 20. Bukten A, Skjærvø I, Stavseth MR. The association of prison security level with mortality after release from prison: a retrospective national cohort study (2000–16). Lancet Public Health 2022; 7: e583‐e592.
- 21. Too LS, Spittal MJ, Bugeja L, et al. The association between mental disorders and suicide: a systematic review and meta‐analysis of record linkage studies. J Affect Disord 2019; 259: 302‐313.
- 22. Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc 1927; 22: 209‐212.
- 23. Wilderman C, Andersen LH. Solitary confinement placement and post‐release mortality risk among formerly incarcerated individuals: a population‐based study. Lancet Public Health 2020; 5: e107‐e113.
- 24. Graf GH, Li X, Kwon D, et al. Biological aging in maltreated children followed up into middle adulthood. Psychoneuroendocrinology 2022; 143: 105848.
- 25. Doidge JC, Higgins DJ, Delfabbro P, Segal L. Risk factors for child maltreatment in an Australian population‐based birth cohort. Child Abuse Negl 2017; 64: 47‐60.
- 26. Moore SE, Scott JG, Ferrari AJ, et al. Burden attributable to child maltreatment in Australia. Child Abuse Negl 2015; 48: 208‐220.
- 27. Higgins DJ, Mathews B, Pacella R, et al. The prevalence and nature of multi‐type child maltreatment in Australia. Med J Aust 2023; 218 (6 Suppl): S19‐S25. https://www.mja.com.au/journal/2023/218/6/australian‐child‐maltreatment‐study‐national‐prevalence‐and‐associated‐health
- 28. Baldwin JR, Arseneault L, Caspi A, et al. Childhood victimization and inflammation in young adulthood: a genetically sensitive cohort study. Brain Behav Immun 2018; 67: 211‐217.
- 1. Mathews B, Pacella R, Scott JG, et al. The prevalence of child maltreatment in Australia: findings from a national survey. Med J Aust 2023; 218 (6 Suppl): S13‐S18. https://www.mja.com.au/journal/2023/218/6/australian‐child‐maltreatment‐study‐national‐prevalence‐and‐associated‐health
- 2. Baldwin JR, Wang B, Karwatowska L, et al. Childhood maltreatment and mental health problems: a systematic review and meta‐analysis of quasi‐experimental studies. Am J Psychiatry 2023; 180: 117‐126.
- 3. Fergusson DM, McLeod GFH, Horwood LJ. Childhood sexual abuse and adult developmental outcomes: findings from a 30‐year longitudinal study in New Zealand. Child Abuse Negl 2013; 37: 664‐674.
- 4. Papalia N, Mann E, Ogloff JRP. Child sexual abuse and risk of revictimization: impact of child demographics, sexual abuse characteristics, and psychiatric disorders. Child Maltreat 2021; 26: 74‐86.
- 5. Assini‐Meytin LC, Thorne EJ, Sanikommu M, et al. Impact of child sexual abuse on socioeconomic attainment in adulthood. J Adolesc Health 2022; 71: 594‐600.
- 6. Lawrence DM, Hunt A, Mathews B, et al. The association between child maltreatment and health risk behaviours and conditions throughout life in the Australian Child Maltreatment Study. Med J Aust 2023; 218 (6 Suppl): S34‐S39. https://www.mja.com.au/journal/2023/218/6/australian‐child‐maltreatment‐study‐national‐prevalence‐and‐associated‐health
- 7. Trauffer N, Widom CS. Child abuse and neglect, and psychiatric disorders in nonviolent and violent female offenders. Violence Gend 2017; 4: 137‐143.
- 8. Kelly‐Irving M, Lepage B, Dedieu D, et al. Adverse childhood experiences and premature all‐cause mortality. Eur J Epidemiol 2013; 28: 721‐734.
- 9. Rod NH, Bengtsson J, Budtz‐Jørgensen E, et al. Trajectories of childhood adversity and mortality in early adulthood: a population‐based cohort study. Lancet 2020; 396: 489‐497.
- 10. Palmer L, Prindle J, Putnam‐Hornstein E. A population‐based examination of suicide and child protection system involvement. J Adolesc Health 2021; 69: 465‐469.
- 11. Segal L, Armfield JM, Gnanamanickam ES, et al. Child maltreatment and mortality in young adults. Pediatrics 2021; 147: e2020023416.
- 12. Castellví P, Miranda‐Mendizábal A, Parés‐Badell O, et al. Exposure to violence, a risk for suicide in youths and young adults: a meta‐analysis of longitudinal studies. Acta Psychiatr Scand 2017; 135: 195‐211.
- 13. White HR, Widom CS. Does childhood victimization increase the risk of early death? A 25‐year prospective study. Child Abuse Negl 2003; 27: 841‐853.
- 14. Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse Negl 2008; 32: 607‐619.
- 15. Cutajar MC, Mullen PE, Ogloff JRP, et al. Suicide and fatal drug overdose in child sexual abuse victims: a historical cohort study. Med J Aust 2010; 192: 184‐187. https://www.mja.com.au/journal/2010/192/4/suicide‐and‐fatal‐drug‐overdose‐child‐sexual‐abuse‐victims‐historical‐cohort
- 16. Rogers NT, Power C, Pinto Pereira SM. Child maltreatment, early life socioeconomic disadvantage and all‐cause mortality in mid‐adulthood: findings from a prospective British birth cohort. BMJ Open 2021; 11: e050914.
- 17. Cutajar MC, Mullen PE, Ogloff JRP, et al. Psychopathology in a large cohort of sexually abused children followed up to 43 years. Child Abuse Negl 2010; 34: 813‐822.
- 18. Australian Institute of Health and Welfare. National Death Index (NDI). Updated 3 July 2023. https://www.aihw.gov.au/about‐our‐data/our‐data‐collections/national‐death‐index (viewed July 2023).
- 19. Australian Institute of Health and Welfare. General Record of Incidence of Mortality (GRIM) books. Updated 11 July 2023. https://www.aihw.gov.au/reports/life‐expectancy‐deaths/grim‐books/contents/data‐visualisation (viewed July 2023).
- 20. Bukten A, Skjærvø I, Stavseth MR. The association of prison security level with mortality after release from prison: a retrospective national cohort study (2000–16). Lancet Public Health 2022; 7: e583‐e592.
- 21. Too LS, Spittal MJ, Bugeja L, et al. The association between mental disorders and suicide: a systematic review and meta‐analysis of record linkage studies. J Affect Disord 2019; 259: 302‐313.
- 22. Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc 1927; 22: 209‐212.
- 23. Wilderman C, Andersen LH. Solitary confinement placement and post‐release mortality risk among formerly incarcerated individuals: a population‐based study. Lancet Public Health 2020; 5: e107‐e113.
- 24. Graf GH, Li X, Kwon D, et al. Biological aging in maltreated children followed up into middle adulthood. Psychoneuroendocrinology 2022; 143: 105848.
- 25. Doidge JC, Higgins DJ, Delfabbro P, Segal L. Risk factors for child maltreatment in an Australian population‐based birth cohort. Child Abuse Negl 2017; 64: 47‐60.
- 26. Moore SE, Scott JG, Ferrari AJ, et al. Burden attributable to child maltreatment in Australia. Child Abuse Negl 2015; 48: 208‐220.
- 27. Higgins DJ, Mathews B, Pacella R, et al. The prevalence and nature of multi‐type child maltreatment in Australia. Med J Aust 2023; 218 (6 Suppl): S19‐S25. https://www.mja.com.au/journal/2023/218/6/australian‐child‐maltreatment‐study‐national‐prevalence‐and‐associated‐health
- 28. Baldwin JR, Arseneault L, Caspi A, et al. Childhood victimization and inflammation in young adulthood: a genetically sensitive cohort study. Brain Behav Immun 2018; 67: 211‐217.






Abstract
Objective: To compare mortality from all causes, internal causes (eg, cancers, circulatory and respiratory system diseases), and external causes (eg, suicide, accidents, assault) among people who were sexually abused during childhood with mortality for the general population.
Design: Historical cohort study.
Setting, participants: 2759 people (2201 women, 79.8%) who had experienced medically assessed contact sexual abuse in Victoria while aged 16 years or younger during 1964–1995, as recorded in Victorian Institute of Forensic Medicine records.
Main outcome measures: Mortality rate, based on linked National Death Index data (1980–2020), by five‐year age group; sex‐ and age‐standardised mortality ratios; comparison of rates with age‐ and sex‐adjusted rates for the general Victorian population (incident rate ratio [IRR]).
Results: We included 115 deaths of people under 50 years of age in our analysis (4.2% of people sexually abused as children; 79 women, 36 men); 56 deaths were attributed to external, 56 to internal causes (cause of death information missing in three cases). In each age group from 15–19 years, the mortality rates for people sexually abused as children were higher than for the general population; age‐ and sex‐standardised all‐cause mortality ratios were highest for people aged 25–29 years (men: 16.5; 95% confidence interval [CI], 11.0–22.0; women: 19.2; 95% CI, 14.3–24.2). The age‐ and sex‐adjusted mortality rate for people sexually abused as children was higher than in the general population for all‐cause (IRR, 8.25; 95% CI, 5.92–11.5), internal cause (IRR, 5.92; 95% CI, 3.89–9.01), and external cause deaths (IRR, 12.6; 95% CI, 9.61–16.6); the differences in external cause mortality were greater for people who had experienced penetrative (IRR, 14.9; 95% CI, 10.9–20.5) than for those who had experienced non‐penetrative sexual abuse as children (IRR, 8.92; 95% CI, 5.35–14.9).
Conclusions: Sexual abuse during childhood is associated with higher mortality rates into mid‐adulthood. Preventing child sexual abuse and intervening early to reduce the damage it inflicts is not only essential for the welfare of the child, but could also help reduce avoidable deaths later in life.