There are about 20 000 out‐of‐hospital cardiac arrests (OHCAs) in Australia each year.1 This is almost 20 times the annual fatal road toll.2 We know that governmental legislation on issues of public safety, such as mandating pool fences or smoke alarms to detect fires, has saved lives. Australia has previously led the world in cardiac arrest innovations; for example, in mandating defibrillator placement on international aircraft and in airport terminals.3 Increasing public access to defibrillators further has the potential to at least double survival from OHCA.4 Over the decades, external defibrillators have evolved from weighing 70 kg to some current models weighing only 300 g.5 In other words, it has never been more feasible to roll out widespread public access defibrillators (PADs). So why have we been so slow to regulate improved availability to a device that can save thousands of Australian lives?
The ABC of cardiac arrest
Cardiac arrest is the cessation of cardiac activity requiring resuscitative measures. There is a wide range of underlying conditions that are associated with cardiac arrest in younger people, but in those aged over 50 years, it is almost always due to coronary heart disease.6
About two‐thirds of OHCAs occur during sleep or at rest and a smaller proportion during exercise. Unfortunately, only about 50% of OHCAs are witnessed.7 It is important to note that 80% of OHCAs occur in the home.8 Although OHCA survival rates are generally only about 10%, they are almost fourfold higher in what is known as the “Utstein population”;9 that is, the event is witnessed and the rhythm of the person is susceptible to shock with a defibrillator. This, of course, demands a nearby defibrillator and a bystander prepared to use it.
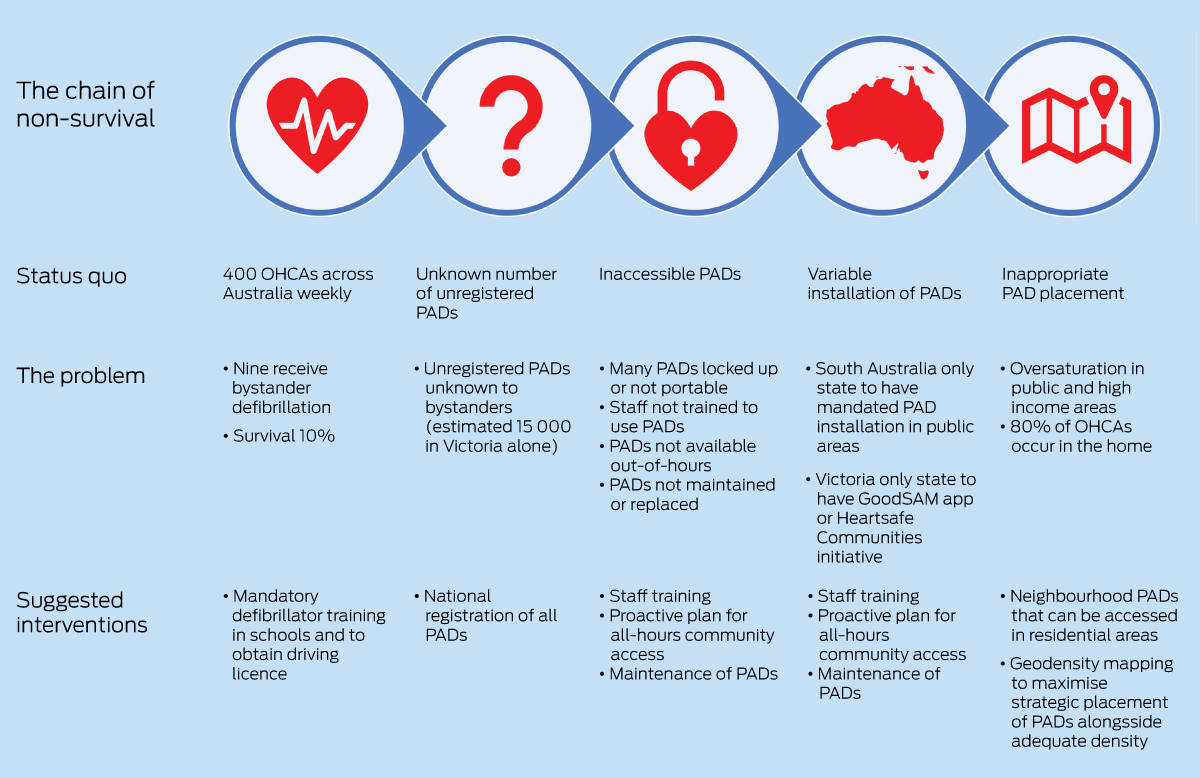
A chain of fatality
Defibrillation is the most useful intervention in OHCAs,10 and the benefits of PADs are well established. In 2016, a Japanese study found that increased PAD use by citizens resulted in a doubling in patient survival with good neurological outcome.10 Given that, at present, 90% of patients with cardiac arrest in Australia die and that one‐quarter of OHCAs have a shockable rhythm,8 implementing widespread PAD availability would indisputably result in lives saved. Yet, of the 400 cardiac arrests across Australia each week, only nine people will be treated with a PAD.5
Why is this? Multiple factors are at play, creating a chain of fatality (Box) that counteracts the widely known chain of survival underpinning successful resuscitation programs. Fortunately, many factors in the chain of fatality can be addressed with simple interventions.
Improving bystander confidence
For people to use PADs, they usually need to be confident in deploying a defibrillator. Only half of Australians have undertaken basic life support training.11 This statistic is particularly poor when compared with the European model, where basic life support training and defibrillator practice are compulsory in schools and later to receive a driving licence.11,12 We advocate for a similar model in Australia, together with public messaging that bystanders do not need to be trained to use a PAD.
Invisible PADs are not publicly accessible
A major issue in the availability of PADs is uncertainty regarding how many PADs exist and where they are located. Registration of PADs with state ambulance services is essential, so that “000” callers can be directed to retrieve and use the nearest PAD; if a PAD is not registered, then it is not truly accessible. It is estimated that there are 15 000 unregistered defibrillators in Victoria alone.4 A national system of collaborative data sharing between all defibrillator registry stakeholders would allow optimal identification of all PADs that exist in Australia but are unavailable for public use.
Locked‐up or faulty PADs are not publicly accessible
Many PADs are not truly accessible. Training staff in access to and use of the defibrillator is recommended. Placing clearly visible signage is important and ensuring that it is truly publicly accessible is vital, not locked up with the keys in an unknown drawer. A clear plan needs to be made on how PADs will remain publicly accessible after hours, as many are only accessible during business hours.13 Finally, maintenance is important. Defibrillators last about seven years, with ultra‐portable defibrillators lasting about one year.14 It is concerning that one‐fifth of PADs are non‐functional when tested,15 potentially wasting time and worsening outcomes in time‐critical cardiac arrest management. Ensuring the defibrillator is electrically sound (battery and electrodes) is a clear prerequisite for restarting the patient's electrical circuitry.
An inequitable state of play
State‐based inconsistencies in defibrillator availability further exacerbate an ad hoc approach. Several large companies, including Coles, Woolworths, Officeworks, Bunnings and Dan Murphy's, have installed PADs nationwide, but this is an independent corporate decision existing outside any national framework.4 Likewise, Heart of the Nation communities, where local communities install PADs in residential areas within 200 m of a group of residents, have been implemented in 71 suburbs to date.
All other policies on defibrillator access and training vary between states. Notably, the South Australian government recently introduced legislation coming into effect in 2025 in which all public facilities must carry a PAD.16 The definition of “public building” is broad, including government facilities, commercial buildings, sporting facilities, and schools. No other State or Territory jurisdiction has firm recommendations or legislation in place.
Other jurisdictions offer differing bystander recruitment. The GoodSAM smartphone application (app; www.goodsamapp.org) was introduced into the Victorian computer‐assisted dispatch (CAD) system in 2018 and uses app‐based messaging to alert basic life support‐trained community volunteers of cardiac arrests within 400 m of their location, as well as notifying them of the nearest PAD. GoodSAM operates a nationally accessible in‐app system, as does Heart of the Nation, which was introduced in 2021 but it is not integrated into the CAD system. Improved survival rates with app‐based messaging have been demonstrated,17 and increasing its reach nationally is necessary. The GoodSAM CAD‐based program is intended to roll out in New South Wales and South Australia soon. The Heart Safe Community program, which is a joint initiative between ambulance Victoria and the Heart Foundation, has been implemented in Victoria, focusing on community education in life support and increasing accessibility to PADs.18
Although only South Australia has mandated PADs in certain locations, this step could easily be taken in all states and territories. The Bill passed in South Australia could be used as a template by other governments who wish to influence positive societal change, with modifications as necessary for varying community and geographic needs. Greater awareness of the issue through public messaging campaigns to support this law‐making process will also help equip the initial lay responder with the skills and tools to save a life, no matter where the cardiac arrest occurs. Rollouts of the app‐based and community programs already established in Victoria should occur on a national level, making all jurisdictions consistent.
Geographic inequity in PAD placement
PADs are most likely to be used when they are within 100 m of the cardiac arrest, so increasing both the density and strategic deployment of PADs is a priority.4 We need to aspire to achieving “all‐access defibrillation”, with PADs available at every cardiac arrest, at any time of day, and accessible to private residences.5
How could the density of PADs in Australia be increased? The first simple step would be for the government to install more PADs. This would likely be a cost‐effective intervention given the economic burden of cardiac arrest is estimated at $2 billion annually.1 Options for PAD placement may include disused telephone boxes, which was very successful in the United Kingdom,19 or on sponsored properties.20 Indirect measures of governmental support could include tax rebates for businesses and individuals providing PADs, as well as mandating defibrillator practice in schools and during driving license applications.11 Ultra‐portable defibrillators have also now entered the Australian market, making widespread purchase of PADs more feasible for short term ownership. This may be more relevant as private citizens increasingly consider it reasonable, if unlikely to be cost‐effective, to stock a personal defibrillator in the home as part of contingency safety equipment, similar to a fire extinguisher or a smoke alarm. Although a household PAD approach may reduce overall cost‐effectiveness, no other harms would be anticipated.
Apart from improving PAD density, strategic PAD location should also be deployed. Geodata analysis can ensure that PADs are deployed where they are most likely to be used, and that oversaturation of public and high income areas does not occur.21,22 Given that 80% of cardiac arrests occur in the home, the greatest challenge is getting PADs into people's homes at any time of day.23 We need to adopt a neighbourhood PAD approach, where PADs are easily accessible within residential areas and neighbours are connected to each other as responders. Strategic deployment of PADs will reduce the overall number required, further enhancing cost‐effectiveness of the program.
Conclusion
The current environment regarding access to defibrillation in Australia is inequitable and contributing to avoidable deaths. We propose that there is significant and feasible scope for improvement through a series of cost‐effective strategies. We encourage uniform action on a national level integrating efforts of government, individual organisations, and local communities.
Provenance: Commissioned; externally peer reviewed.
- 1. Paratz ED, Smith K, Ball J, et al. The economic impact of sudden cardiac arrest. Resuscitation 2021; 163: 49‐56.
- 2. Transport Accident Commission. Searchable road trauma statistics Victoria, Australia. https://www.tac.vic.gov.au/road‐safety/statistics/online‐crash‐database/search‐crash‐data?date‐period=%22the+last+12+months%22&date‐after=&date‐before=&meta_J_orsand=&meta_G_orsand=&query=%21padrenull&collection=tac‐xml‐meta&clive=tac‐fatalities‐xml (viewed Apr 2023).
- 3. O'Rourke MF, Donaldson E, Geddes JS. An airline cardiac arrest program. Circulation 1997; 96: 2849‐2853.
- 4. Haskins B, Nehme Z, Cameron P, et al. Coles and Woolworths have installed public access defibrillators in all their stores: it is time other Australian businesses followed their lead. Emerg Med Australas 2020; 32: 166‐168.
- 5. Grunau B, Rea T. A goal to transform public access defibrillation to all access defibrillation. Resuscitation 2021; 162: 417‐419.
- 6. Paratz ED, van Heusden A, Zentner D, et al. Causes, circumstances, and potential preventability of cardiac arrest in the young: insights from a state‐wide clinical and forensic registry. Europace 2022; 24: 1933‐1941.
- 7. Schober P, van den Beuken WMF, Niderost B, et al. Smartwatch based automatic detection of out‐of‐hospital cardiac arrest: Study rationale and protocol of the HEART‐SAFE project. Resusc Plus 2022; 12: 100324.
- 8. Nair R, Andrew E, Sathish‐Kumar K. VACAR annual report 2020–2021. Melbourne: Ambulance Victoria, 2021 https://www.ambulance.vic.gov.au/wp‐content/uploads/2022/10/VACAR‐Annual‐Report‐2020‐21.pdf (viewed Apr 2023).
- 9. Bray J, Howell S, Ball S, et al; Aus‐ROC Epistry Management Committee. The epidemiology of out‐of‐hospital cardiac arrest in Australia and New Zealand: A binational report from the Australasian Resuscitation Outcomes Consortium (Aus‐ROC). Resuscitation 2022;172: 74‐83.
- 10. Kitamura T, Kiyohara K, Sakai T, et al. Public‐access defibrillation and out‐of‐hospital cardiac arrest in Japan. N Engl J Med 2016; 375: 1649‐1659.
- 11. Bray J, Acworth J, Page G, et al. Aussie KIDS SAVE LIVES: a position statement from the Australian Resuscitation Council and supported by stakeholders. Emerg Med Australas 2021; 33: 944‐946.
- 12. Juul Grabmayr A, Andelius L, Bo Christensen N, et al. Contemporary levels of cardiopulmonary resuscitation training in Denmark. Resusc Plus 2022; 11: 100268.
- 13. Hansen CM, Wissenberg M, Weeke P, et al. Automated external defibrillators inaccessible to more than half of nearby cardiac arrests in public locations during evening, nighttime, and weekends. Circulation 2013; 128: 2224‐2231.
- 14. Naser N. On occasion of seventy‐five years of cardiac defibrillation in humans. Acta Inform Med 2023; 31: 68‐72.
- 15. Jespersen SS, Kjoelbye JS, Christensen HC, et al. Functionality of registered automated external defibrillators. Resuscitation 2022; 176: 58‐63.
- 16. Kovoor JG, Page GJ, Kovoor P. Historic breakthrough for public access defibrillation in Australia. Med J Aust 2023; 218: 238. https://www.mja.com.au/journal/2023/218/5/historic‐breakthrough‐public‐access‐defibrillation‐australia
- 17. Smith CM, Lall R, Fothergill RT, et al. The effect of the GoodSAM volunteer first‐responder app on survival to hospital discharge following out‐of‐hospital cardiac arrest. Eur Heart J Acute Cardiovasc Care 2022; 11: 20‐31.
- 18. Naccarella L, Saxton D, Lugg E, Marley J. It takes a community to save a life in cardiac arrest: heart safe community pilots, Australia. Health Promot J Austr 2022; 33: 99‐105.
- 19. Hancock S. Red phone boxes get new lease of life as defibrillators and mini museums. Independent 2021; 15 Mar. https://www.independent.co.uk/news/uk/home‐news/red‐phone‐box‐bt‐defibrillator‐b1817058.html (viewed July 2023).
- 20. Ball S, Morgan A, Simmonds S, et al. Strategic placement of automated external defibrillators (AEDs) for cardiac arrests in public locations and private residences. Resusc Plus 2022; 10: 100237.
- 21. Aeby D, Staeger P, Dami F. How to improve automated external defibrillator placement for out‐of‐hospital cardiac arrests: a case study. PLoS One 2021; 16: e0250591.
- 22. Brown TP, Perkins GD, Smith CM, et al. Are there disparities in the location of automated external defibrillators in England? Resuscitation 2022; 170: 28‐35.
- 23. Karlsson L, Hansen CM, Vourakis C, et al. Improving bystander defibrillation in out‐of‐hospital cardiac arrests at home. Eur Heart J Acute Cardiovasc Care 2020; 9 (Suppl): S74‐S81.






Open access:
Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Gregory Page is a survivor of sudden cardiac arrest.
Gregory Page was Public Access Ambassador for Stryker from March 2020 until March 2022.