Summary box
The known: The role of medicines in suicide is complex: they are a common means of suicide in high income countries, non‐adherence to psychotropic therapy is a challenge for health care professionals treating people at risk of suicide, and some medicines are themselves associated with increased risk of self‐harm.
The new: Mismatches between the dispensing of medicines around the time of death from suicide and post mortem toxicology findings suggest considerable levels of non‐adherence to psychotropic pharmacotherapy and inappropriate psychotropic medicine accumulation.
The implications: Monitoring adherence to psychotropic therapy, cessation of therapy, and safe storage and disposal of medicines are important for reducing the risk of suicide.
As mental illness1,2 and many physical disorders are risk factors for suicide,3 the appropriate use of medicines for treating people with these conditions plays a role in suicide prevention. However, medicine overdose, especially with psychotropic medicines, is among the most common suicide methods in high income countries,4 and the incidence of non‐fatal deliberate self‐poisoning is also rising.5 Moreover, non‐adherence to psychotropic therapy is a key challenge for clinicians caring for people at risk of suicide,6 and some psychotropic and non‐psychotropic medicines have been associated with increased risk of suicidal behavior.7,8,9,10
Medicine use at the time of death by suicide has been investigated by analysing administrative claims11,12 and forensic toxicology data.13,14 The former typically provide information on whether a medicine was dispensed, the latter on whether it was used. Studies applying these approaches, mostly in high income countries, have found similar rates of medicine use at the time of death, but have not linked sources of the two data types. Data linkage could provide a more robust overview of medicine use at the time of death and consequently of the medical conditions being treated at this point, improving our knowledge of therapy adherence and medicine use by people who die by suicide.
We therefore analysed linked whole population Australian data on medicine dispensing, toxicology, and mortality to determine the numbers and types of medicines dispensed around the time of death to people who died by suicide, and to compare the medicines listed in post mortem toxicology reports with those recently dispensed.
Methods
We analysed data from the Australian Suicide Prevention using Health Linked Data (ASHLi) study, a population‐based case series study of closed coronial cases for deaths of people in Australia aged ten years or more during 1 July 2013 – 10 October 2019 (date of data extraction) deemed by coroners to be the result of intentional self‐harm.15 In the ASHLi study, National Coronial Information System (NCIS) data were linked with several administrative datasets, including that of the Pharmaceutical Benefits Scheme (PBS).
Any death in Australia suspected to have been a suicide is investigated by a coroner. The NCIS includes detailed information pertaining to each coronial inquiry, including the demographic characteristics of the deceased person, the details and circumstances of their death, and autopsy findings, including any toxicology findings. For this study, we examined toxicology report information regarding drugs and their metabolites detected at autopsy. Post mortem toxicology screening does not encompass all medications, but typically includes almost all psychotropic and analgesic medicines.
For our analysis, we included all PBS‐listed medicines dispensed in the community, by private hospitals, or (for most states) on discharge from public hospitals. The PBS does not subsidise non‐prescription, complementary and alternative medicines, or medicines dispensed within public hospitals to inpatients. Private prescriptions (ie, the patient pays the entire cost of the medicine) are not included in PBS data. The PBS captures the date the medicine was dispensed and medicine‐specific information, including the PBS item code, linked with the World Health Organization Anatomical Therapeutic Chemical (ATC) classification.16
Data linkage
Coronial records for suicide deaths that matched our inclusion criteria were identified by the NCIS, which provided the relevant personal identifiers to the Australian Institute of Health and Welfare (AIHW) for probabilistic linkage with PBS records (and other administrational datasets not pertinent to this article). De‐identified linked data were provided to the researchers.
Measures
We extracted data on age, sex, marital status, employment status, remoteness of residence at time of death (Statistical Area 317), and method of death (as recorded in cause of death field: hanging, poisoning, falls, firearm, drowning, sharp object, moving object, or other) for each deceased person. Each record was then further classified according to whether the coroner found that the death involved poisoning with a medicine; that is, one or more medicines were found to have contributed to the death, regardless of whether they were the primary cause.
We categorised medicines by ATC code according to the anatomical main group (ATC first level), medicine class (ATC third level), and the specific medicine (ATC fifth level).
As the prescribed dose of medicines cannot be directly ascertained from PBS records, which include only information on the quantity and strength of medicines dispensed, we estimated medicine exposure time using the PBS 10% sample dataset, a standard dataset provided by Services Australia; it includes all prescription medicine claims for a nationally representative, random 10% sample of PBS‐eligible Australian residents.16 For each medicine, we calculated the number of days between two consecutive dispensings for each person in the PBS 10% sample dataset dispensed the medicine during the period covered by the ASHLi study; we defined the period of exposure as the number of days within which 75% of people in the PBS 10% sample dataset had received a second dispensing of the same medicine. For medicines not dispensed in sufficient quantity to reliably estimate the period of exposure, it was deemed to be fourteen days, as described in an earlier study.18 If the period between the final dispensing and the date of death was less than the estimated exposure period, the medicine was deemed to have been dispensed around the time of death.
Comparison of recent dispensing and post mortem detection of medicines
We compared the recent dispensing and post mortem detection of specific medicines. For psychotropic medicines routinely screened for during autopsy (antidepressants, antipsychotics, anxiolytics, opioids, sedatives/hypnotics), we compared the medicine classes detected post mortem with those deemed to have been dispensed around the time of death, using three dispensing/detection categories: the medicine was dispensed and detected post mortem; the medicine was dispensed but not detected post mortem; and the medicine was detected but had not recently been dispensed.
Statistical analysis
All analyses were conducted in R 4.2.1 (R Foundation for Statistical Computing). We calculated the proportions of people for whom medicines were dispensed around the time of death (case frequency), by medicine group, class, and specific medicine; we report the age and sex characteristics of people dispensed these medicines, and the proportion for whom poisoning with one or more medicines was implicated in their deaths. We also determined the number of different medicines dispensed to each person around the time of death.
For the most frequently dispensed psychotropic medicine classes, we determined the proportions of people for whom a medicine from that class was dispensed or detected in each dispensing/detection category. We then determined the proportion of any medicine‐related deaths among people dispensed each medicine class and detection/dispensing category.
Ethics approval
Our study was approved by the Justice Human Research Ethics Committee of the Victorian Department of Justice and Community Safety (CF/17/23250), the Western Australian Coronial Ethics Committee (EC 14/18 M0400), the AIHW Ethics Committee (EO2017/4/366), and the NSW Population and Health Services Research Ethics Committee (2017/HRE1204, 2013/11/494). Access to the 10% PBS sample was granted by the Services Australia external request evaluation committee (RMS2076).
Results
Of the 14 637 NCIS records for people who died by suicide, 14 354 could be linked by the AIHW to PBS records (98.1%); 148 were excluded after assessing the consistency of key data across the linked datasets. Of the remaining 14 206 cases, forensic toxicology examination reports were available for 13 541 people and were included in our analysis (95.3% of eligible linked record sets); their median age was 44 years (interquartile range [IQR], 31–57 years), and 10 246 were men (75.7%) (Box 1).
Medicines dispensed around the time of death
At least one PBS‐subsidised medicine had been dispensed around the time of death to 7998 people (59.1%); their median age was 49 years (IQR, 36–63 years), and 5620 were men (70.3%). Two or more medicines had been dispensed around the time of death to 5637 people (41.6%) and five or more to 1943 (14.3%). The most frequently dispensed medicine classes, both overall (6456 of 13 541, 47.7%) and for each combination of sex and age group were nervous system medicines (Box 2, Box 3). The most frequently dispensed specific medicines were the nervous system medicines diazepam, mirtazapine, temazepam, quetiapine, and escitalopram (Box 4).
Comparison of medicines dispensed and detected post mortem
Medicines (or their metabolites) were detected post mortem in 9042 people (66.8%). At least one medicine not dispensed around the time of death was detected in 7135 people (52.7%) (Box 5), for 1042 of whom (14.6%) poisoning with one or more medicines was implicated in their deaths.
For three of the most frequently dispensed nervous system medicine classes, the proportions of people in whom the medicines were detected post mortem and their death was deemed medicine‐related were larger for those without records of recent dispensing than for people for whom they had been dispensed around the time of death: antidepressants (17.7% v 12.0%), anxiolytics (16.3% v 14.8%), and sedatives/hypnotics (24.3% v 16.5%) (Box 6).
At least one medicine dispensed around the time of death but not detected post mortem was identified for 6208 people (45.8%); the most frequently dispensed but not detected (of those routinely screened for post mortem) was temazepam (326 people, 2.4%) (Supporting Information, table 2).
Discussion
We found that PBS‐subsidised medicines had been recently dispensed to 59% of people who died by suicide in Australia during 2013–2019, and that more than one medicine had been dispensed to 42%. The most frequently dispensed drugs were nervous system medicines, and the most frequent class dispensed was antidepressants. One or more medicines not recently dispensed were detected post mortem in 53% of people who died by suicide.
The proportions of people in our study dispensed medicines from most classes were larger than for the overall Australian population in 2018; the differences were particularly marked for nervous system medicines (antidepressants: 30.9% v 7.4%; antipsychotics: 11.3% v 1.4%; anxiolytics: 13.4% v < 1%; opioids: 10.0% v 2.6%; hypnotics/sedatives: 7.2% v < 1%)18 (Supporting Information, table 3). These differences are partly attributable to differences in age and sex distributions, but the generally higher dispensing rates for most medicines probably reflect the chronic nature of physical and mental disorders in people who die by suicide.
We found that antidepressants had recently been dispensed to or were detected post mortem in 38% of people who died by suicide, a smaller proportion than expected given their burden of depression and anxiety; the Global Burden of Disease Study 2010 estimated that depression is responsible for 46.1% (95% confidence interval [CI], 28.0–60.8%) of the disability‐adjusted life years (DALYs) lost to suicide, and anxiety disorders for 7.4% (95% CI, 3.0–12.7%).2 Our finding suggests that many people with depression or anxiety were not adhering to prescribed pharmacotherapy, were not being treated with antidepressants, or were not being treated for depression or anxiety around the time of their deaths. Indeed, another Australian data linkage study found low levels of mental health service use prior to suicide,19 and the estimated mental health treatment rate for people with mental illness in Australia in 2014 was only 35%.20 Our finding may therefore reflect generally low levels of help‐seeking by people with mental illness.
Antipsychotics had been recently dispensed to or were detected post mortem in 16% of people, more consistent with the numbers of suicide‐related lost DALYs attributed to bipolar disorder (5.4%; 95% CI, 1.8–10.7%) and schizophrenia (4.7%; 95% CI, 4.1–5.3%).2 We have no information on the indications for medicine prescribing, but our findings suggest that people with schizophrenia or bipolar disorder were more frequently using pharmacotherapy at the time of death than those with depression or anxiety.
Many medicines dispensed around the time of death were not detected post mortem (Supporting Information, table 2), suggesting non‐adherence to therapy. As cessation of antidepressants21 and opioids22 has been associated with greater risk of suicide, the possibility of non‐adherence and the importance of monitoring medicine use6 and assisting with safe tapering and cessation of medicines23 should be borne in mind.
In our study, poisoning by medicines was identified as a contributor to 8.6% of deaths. However, the proportions of medicine poisoning‐related deaths were larger for people recently dispensed most medicine types, and was largest for those dispensed opioids (19.6%) (Box 3). This finding indicates that dispensing of prescription medicines provides access to means for self‐harm, reinforcing the need for caution when prescribing toxic medicines for patients at risk of suicide.13 Further, these medicines may be taken in combination with other medicines or substances, leading to synergistic toxic effects.24
We also found that the proportions of deaths in which poisoning with medicine was implicated were larger for people in whom antidepressants, anxiolytics, or sedatives/hypnotics were detected but had not been dispensed around the time of death than for those for whom the medicine had been dispensed around the time of death (Box 6). This finding suggests that some medicines likely to have been used for suicide were obtained on private prescriptions, had not been dispensed to the person who died (ie, were obtained illegally or from another household member), or had been dispensed many months before the death of the person who used them. The latter possibility may reflect medicine stockpiling or unintentional accumulation, each of which increases access to means for suicide and highlights the importance of safe disposal of unused medicines.
Limitations
Our study overcame many limitations of analysing coronial data or dispensing data alone by examining medicine use according to whether it was dispensed and used by individuals around the time of their deaths. We have nevertheless probably underestimated medicine use. The PBS does not subsidise all dispensed medicines, and post mortem toxicology does not routinely screen for all medicines. Moreover, several factors influence post mortem detectability of drugs, including technological limits of detection and reporting,25 post mortem changes,26 and drug stability.27 As we did not assess combinations of medicines with other medicines or with substances such as alcohol and illicit drugs, we cannot draw conclusions about synergistic toxicity related to drug–drug interactions. The time between death, finalisation of the coronial enquiry, and data linkage means that we did not include all suicide deaths, particularly during the latter years of the series.15
Conclusions
We found that the proportion of people who died by suicide during 2013–19 who were using antidepressants at the time of their deaths was lower than would be expected given the estimated burden of depression and anxiety in people who die by suicide,2 perhaps reflecting suboptimal levels of treatment for people with mental illness. A considerable number of people were dispensed psychotropic medicines in the period preceding their death that were not detected post mortem, suggesting non‐adherence to treatment. Finally, medicines were detected post mortem in many people for whom they had not recently been dispensed, indicating the need to curb the inappropriate intentional or unintentional stockpiling of medicines.
Box 1 – Characteristics of 13 541 people who died by suicide in Australia, 1 July 2013 – 10 October 2019
|
Characteristic |
Number of people |
||||||||||||||
|
|
|||||||||||||||
|
Total number of deceased persons |
13 541 |
||||||||||||||
|
Age (years), median (IQR) |
44 (31–57) |
||||||||||||||
|
10–24 |
1843 (13.6%) |
||||||||||||||
|
25–44 |
5070 (37.4%) |
||||||||||||||
|
45–64 |
4525 (33.4%) |
||||||||||||||
|
65 or older |
2103 (15.5%) |
||||||||||||||
|
Sex (men) |
10 246 (75.7%) |
||||||||||||||
|
Geographic remoteness* |
|
||||||||||||||
|
Major cities |
8274 (61.1%) |
||||||||||||||
|
Inner regional |
2960 (21.9%) |
||||||||||||||
|
Outer regional |
1453 (10.7%) |
||||||||||||||
|
Remote/very remote |
435 (3.2%) |
||||||||||||||
|
Missing data |
419 (3.1%) |
||||||||||||||
|
Employment status |
|
||||||||||||||
|
Employed |
4790 (35.4%) |
||||||||||||||
|
Unemployed |
3578 (26.4%) |
||||||||||||||
|
Student |
618 (4.6%) |
||||||||||||||
|
Retired/pensioner |
2579 (19.0%) |
||||||||||||||
|
Other |
173 (1.3%) |
||||||||||||||
|
Missing data |
1803 (13.3%) |
||||||||||||||
|
Marital status |
|
||||||||||||||
|
Never married |
3691 (27.2%) |
||||||||||||||
|
Married |
4666 (34.5%) |
||||||||||||||
|
Separated/divorced |
2777 (20.5%) |
||||||||||||||
|
Widowed |
563 (4.2%) |
||||||||||||||
|
Missing data |
1844 (13.6%) |
||||||||||||||
|
Method of death† |
|
||||||||||||||
|
Hanging |
7422 (54.8%) |
||||||||||||||
|
Any poisoning |
3366 (24.9%) |
||||||||||||||
|
Poisoning with medicines‡ |
1163 (8.6%) |
||||||||||||||
|
Falls |
668 (4.9%) |
||||||||||||||
|
Firearm |
771 (5.7%) |
||||||||||||||
|
Sharp object |
399 (2.9%) |
||||||||||||||
|
Moving object |
586 (4.3%) |
||||||||||||||
|
Other |
750 (5.5%) |
||||||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Australian Statistical Geography Standard (ASGS).17 † Multiple causes possible. ‡ In the National Coronial Information System records, a further 837 deaths (6.2%) under “any poisoning” had “mixed drug” listed as a contributor to death, without specifying the drugs involved. |
|||||||||||||||
Box 2 – Dispensing of medicines around the time of death to 13 541 people who died by suicide in Australia, 1 July 2013 – 10 October 2019, by Anatomical Therapeutic Classification (ATC) first level category, sex, and age group*
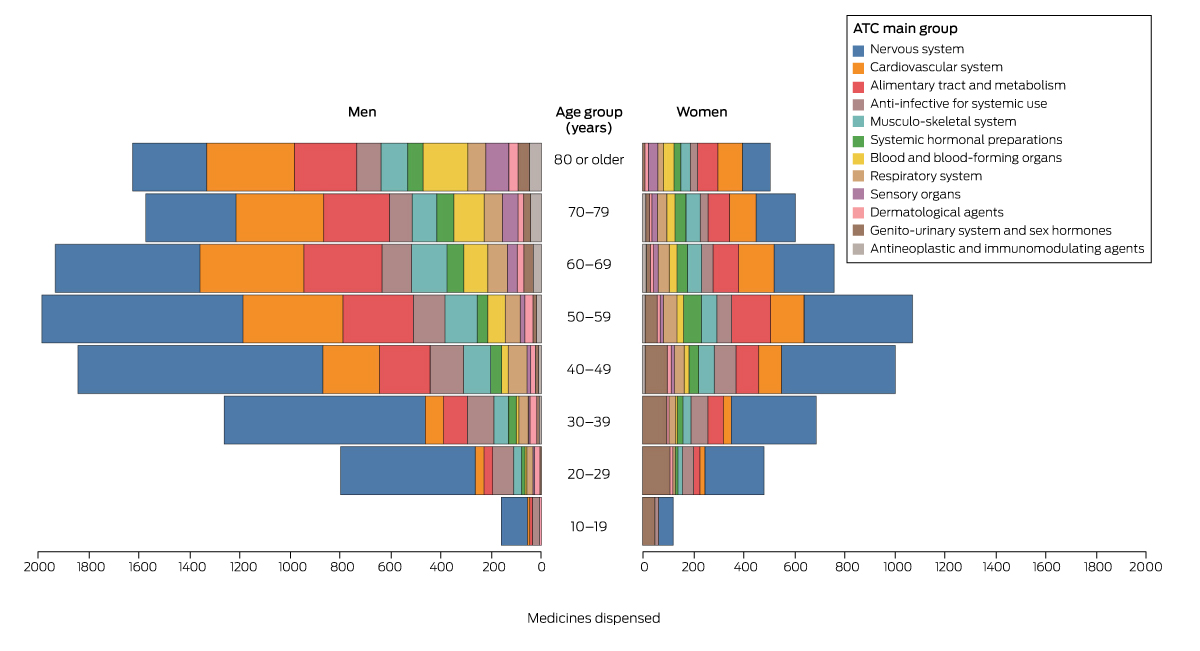
* Data for medicines dispensed to fewer than six people by age/sex group are not included in the figure.
Box 3 – The twenty medicine classes (Anatomical Therapeutic Classification [ATC] third level) most frequently dispensed around the time of death to 13 541 people who died by suicide in Australia, 1 July 2013 – 10 October 2019
|
Medicine class (ATC third level) |
Dispensing frequency* |
Case frequency† |
Median age, years (IQR) |
Men |
Poisoning with medicines‡ |
||||||||||
|
|
|||||||||||||||
|
Antidepressants (N06A) |
7078 |
4183 (30.9%) |
47 (35–59) |
2748 [65.7%] |
497 [11.9%] |
||||||||||
|
Anxiolytics (N05B) |
3423 |
1810 (13.4%) |
47 (36–57) |
1140 [63.0%] |
260 [14.4%] |
||||||||||
|
Antipsychotics (N05A) |
2816 |
1525 (11.3%) |
44 (33–55) |
1012 [66.4%] |
199 [13.0%] |
||||||||||
|
Opioids (N02A) |
3006 |
1359 (10.0%) |
53 (41–68) |
880 [64.8%] |
266 [19.6%] |
||||||||||
|
Drugs for peptic ulcer/gastro‐oesophageal reflux disease (A02B) |
1873 |
1345 (9.9%) |
62 (50–75) |
953 [70.9%] |
218 [16.2%] |
||||||||||
|
Lipid‐modifying agents, plain (C10A) |
1314 |
1023 (7.6%) |
66 (56–78) |
799 [78.1%] |
145 [14.2%] |
||||||||||
|
Hypnotics/sedatives (N05C) |
1558 |
978 (7.2%) |
55 (42–68) |
630 [64.4%] |
129 [13.2%] |
||||||||||
|
Other analgesics and antipyretics (N02B) |
1256 |
725 (5.4%) |
60 (46–74) |
475 [65.5%] |
142 [19.6%] |
||||||||||
|
Beta‐blocking agents (C07A) |
913 |
641 (4.7%) |
63 (50–77) |
480 [74.9%] |
112 [17.5%] |
||||||||||
|
Anti‐inflammatory/anti‐rheumatic agents, non‐steroid (M01A) |
765 |
576 (4.3%) |
54 (42–66) |
387 [67.2%] |
83 [14%] |
||||||||||
|
Adrenergic agents, inhalants (R03A) |
1175 |
564 (4.2%) |
59 (44–72) |
359 [63.7%] |
95 [17%] |
||||||||||
|
Anti‐thrombotic agents (B01A) |
830 |
555 (4.1%) |
73 (61–82) |
444 [80.0%] |
82 [15%] |
||||||||||
|
Beta‐lactam antibacterial agents, penicillins (J01C) |
581 |
482 (3.6%) |
49 (37–67) |
338 [70.1%] |
54 [11%] |
||||||||||
|
Angiotensin‐converting enzyme inhibitors, plain (C09A) |
583 |
473 (3.5%) |
66 (56–78) |
398 [84.1%] |
62 [13%] |
||||||||||
|
Anti‐epileptics (N03A) |
764 |
461 (3.4%) |
48 (38–59) |
266 [57.7%] |
75 [16%] |
||||||||||
|
Angiotensin II receptor blockers, plain (C09C) |
530 |
437 (3.2%) |
66 (55–78) |
319 [73.0%] |
58 [13%] |
||||||||||
|
Blood glucose‐lowering agents, excl. insulins (A10B) |
732 |
405 (3.0%) |
62 (52–71) |
322 [79.5%] |
63 [16%] |
||||||||||
|
Corticosteroids for systemic use, plain (H02A) |
506 |
348 (2.6%) |
65 (48–76) |
224 [64.4%] |
52 [15%] |
||||||||||
|
Angiotensin II receptor blockers, combinations (C09D) |
400 |
333 (2.5%) |
63 (54–73) |
261 [78.4%] |
32 [10%] |
||||||||||
|
Hormonal contraceptives for systemic use (G03A) |
379 |
325 (2.4%) |
30 (22–39) |
— |
39 [12%] |
||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Dispensing of medicines in class for which estimated duration of therapy included the date of death. † Individuals dispensed at least one medicine from the class, and estimated duration of therapy included date of death. ‡ Individuals dispensed at least one medicine from the class, and poisoning with any medicine was deemed to have contributed to their death. |
|||||||||||||||
Box 4 – The twenty medicines most frequently dispensed around the time of death to 13 541 people who died by suicide in Australia, 1 July 2013 – 10 October 2019
|
Medicine |
Dispensing frequency* |
Case frequency† |
Median age, years (IQR) |
Men |
Poisoning with medicines‡ |
||||||||||
|
|
|||||||||||||||
|
Diazepam |
2687 |
1466 (10.8%) |
45 (35–55) |
939 [64.1%] |
197 [13%] |
||||||||||
|
Mirtazapine |
1203 |
871 (6.4%) |
52 (40–63) |
607 [69.7%] |
81 [9%] |
||||||||||
|
Temazepam |
1325 |
861 (6.4%) |
54 (41–68) |
563 [65.4%] |
102 [12%] |
||||||||||
|
Quetiapine |
1176 |
673 (5.0%) |
43 (33–55) |
390 [57.9%] |
124 [18%] |
||||||||||
|
Escitalopram |
807 |
588 (4.3%) |
44 (33–55) |
410 [69.7%] |
44 [8%] |
||||||||||
|
Esomeprazole |
769 |
562 (4.2%) |
60 (48–72) |
371 [66.0%] |
99 [18%] |
||||||||||
|
Venlafaxine |
871 |
555 (4.1%) |
47 (37–59) |
335 [60.4%] |
71 [13%] |
||||||||||
|
Oxycodone |
953 |
494 (3.6%) |
56 (42–70) |
323 [65.4%] |
114 [23%] |
||||||||||
|
Atorvastatin |
602 |
479 (3.5%) |
67 (55–79) |
391 [81.6%] |
63 [13%] |
||||||||||
|
Codeine/paracetamol |
708 |
478 (3.5%) |
47 (37–59) |
303 [63.4%] |
76 [16%] |
||||||||||
|
Sertraline |
673 |
477 (3.5%) |
46 (32–59) |
311 [65.2%] |
52 [11%] |
||||||||||
|
Pantoprazole |
603 |
469 (3.5%) |
63 (51–75) |
344 [73.3%] |
72 [15%] |
||||||||||
|
Desvenlafaxine |
665 |
468 (3.5%) |
46 (35–55) |
320 [68.4%] |
32 [7%] |
||||||||||
|
Pregabalin |
748 |
430 (3.2%) |
51 (41–64) |
275 [64.0%] |
91 [21%] |
||||||||||
|
Olanzapine |
613 |
415 (3.1%) |
47 (36–58) |
305 [73.5%] |
37 [9%] |
||||||||||
|
Amitriptyline |
713 |
394 (2.9%) |
52 (42–63) |
222 [56.3%] |
97 [25%] |
||||||||||
|
Paracetamol |
508 |
353 (2.6%) |
70 (57–81) |
230 [65.2%] |
61 [17%] |
||||||||||
|
Rosuvastatin |
412 |
336 (2.5%) |
64 (54–75) |
248 [73.8%] |
47 [14%] |
||||||||||
|
Fluoxetine |
481 |
332 (2.5%) |
44 (28–55) |
190 [57.2%] |
46 [14%] |
||||||||||
|
Oxazepam |
518 |
310 (2.3%) |
55 (44–68) |
177 [57.1%] |
62 [20%] |
||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Dispensing of medicines in class for which estimated duration of therapy included the date of death; multiple dispensing to individuals is possible. † Individuals dispensed at least one medicine from the class, and estimated duration of therapy included date of death. ‡ Individuals dispensed medicines for whom poisoning with any medicine was deemed to have contributed to their death. |
|||||||||||||||
Box 5 – The twenty medicines most frequently detected post mortem but not dispensed around the time of death for 13 541 people who died by suicide in Australia, 1 July 2013 – 10 October 2019
|
|
Number of people |
|
|||||||||||||
|
Medicine/metabolites |
Medicine/metabolites detected |
Medicine dispensed outside exposure period |
Comments |
||||||||||||
|
|
|||||||||||||||
|
Paracetamol/metabolites |
1377 |
478 (34.7%) |
Available without prescription |
||||||||||||
|
Diazepam/metabolites |
1051 |
571 (54.3%) |
Often prescribed pro re nata |
||||||||||||
|
Morphine/metabolites |
862 |
27 (3.1%) |
Administered before or during hospitalisation for pain; can be detected as metabolite of codeine or heroin |
||||||||||||
|
Temazepam |
820 |
268 (32.7%) |
Often prescribed pro re nata; can also be detected as metabolite of diazepam |
||||||||||||
|
Oxazepam |
778 |
106 (13.6%) |
Often prescribed pro re nata, can also be detected as metabolite of diazepam |
||||||||||||
|
Codeine/metabolites |
659 |
245 (37.2%) |
Available without prescription until February 2018 |
||||||||||||
|
Doxylamine/metabolites |
542 |
< 6 |
Available without prescription, not subsidised by PBS |
||||||||||||
|
Ibuprofen/metabolites |
511 |
22 (4.3%) |
Available without prescription |
||||||||||||
|
Nortriptyline/metabolites |
474 |
15 (3.2%) |
Can be detected as metabolite of amitriptyline |
||||||||||||
|
Midazolam |
332 |
< 6 |
Almost exclusively administered in hospital or by paramedics to people with seizures, agitation |
||||||||||||
|
Quetiapine |
302 |
144 (47.7%) |
Used for many off‐label indications not subsidised by the PBS |
||||||||||||
|
Metoclopramide |
301 |
98 (33%) |
Used in hospitals as an anti‐emetic; available without prescription |
||||||||||||
|
Oxycodone |
277 |
140 (50.5%) |
|
||||||||||||
|
Clonazepam/metabolites |
261 |
17 (6.5%) |
Often prescribed pro re nata |
||||||||||||
|
Mirtazapine |
221 |
147 (66.5%) |
Often prescribed privately |
||||||||||||
|
Phenobarbitone |
216 |
< 6 |
|
||||||||||||
|
Promethazine |
199 |
< 6 |
Available without prescription |
||||||||||||
|
Olanzapine |
199 |
103 (51.8%) |
|
||||||||||||
|
Quinine |
183 |
< 6 |
|
||||||||||||
|
Metoprolol |
183 |
< 6 |
|
||||||||||||
|
|
|||||||||||||||
|
PBS = Pharmaceutical Benefits Scheme. * A comprehensive list of medicines detected post mortem but not dispensed around the time of death is included in the Supporting Information, table 1. |
|||||||||||||||
Box 6 – Nervous system medicine classes dispensed to or detected post mortem in 13 541 people who died by suicide in Australia, 1 July 2013 – 10 October 2019
|
Medicine class (ATC third level class) |
Frequency* (proportion of people) |
Poisoning with medicines† |
|||||||||||||
|
|
|||||||||||||||
|
Antidepressant (N06A) |
|
|
|||||||||||||
|
Dispensed or detected‡ |
5152 (38.0%) |
634 (12.3%) |
|||||||||||||
|
Dispensed and detected |
3523 (26.0%) |
423 (12.0%) |
|||||||||||||
|
Detected, not dispensed§ |
1534 (11.3%) |
272 (17.7%) |
|||||||||||||
|
Dispensed, not detected |
890 (6.6%) |
98 (11%) |
|||||||||||||
|
Antipsychotic (N05A) |
|
|
|||||||||||||
|
Dispensed or detected‡ |
2172 (16.0%) |
285 (13.1%) |
|||||||||||||
|
Dispensed and detected |
1021 (7.5%) |
150 (14.7%) |
|||||||||||||
|
Detected, not dispensed§ |
786 (5.8%) |
110 (14.0%) |
|||||||||||||
|
Dispensed, not detected |
611 (4.5%) |
71 (12%) |
|||||||||||||
|
Anxiolytic (N05B) |
|
|
|||||||||||||
|
Dispensed or detected‡ |
3453 (25.5%) |
525 (15.2%) |
|||||||||||||
|
Dispensed and detected |
1569 (11.6%) |
232 (14.8%) |
|||||||||||||
|
Detected, not dispensed§ |
2098 (15.5%) |
342 (16.3%) |
|||||||||||||
|
Dispensed, not detected |
299 (2.2%) |
41 (14%) |
|||||||||||||
|
Opioids (N02C) |
|
|
|||||||||||||
|
Dispensed or detected‡ |
2878 (21.3%) |
558 (19.4%) |
|||||||||||||
|
Dispensed and detected |
848 (6.3%) |
203 (23.9%) |
|||||||||||||
|
Detected, not dispensed§ |
1928 (14.2%) |
393 (20.4%) |
|||||||||||||
|
Dispensed, not detected |
671 (5.0%) |
96 (14%) |
|||||||||||||
|
Sedatives/hypnotics (N05C) |
|
|
|||||||||||||
|
Dispensed or detected‡ |
2719 (20.1%) |
552 (20.3%) |
|||||||||||||
|
Dispensed and detected |
629 (4.6%) |
104 (16.5%) |
|||||||||||||
|
Detected, not dispensed§ |
1840 (13.6%) |
447 (24.3%) |
|||||||||||||
|
Dispensed, not detected |
359 (2.7%) |
26 (7.2%) |
|||||||||||||
|
|
|||||||||||||||
|
* Unique individuals dispensed the medicine around time of death or in whom medicine was detected post mortem; multiple categories within drug class possible. † Proportion of unique individuals to whom the medicine was dispensed or in whom it was detected post mortem for whom poisoning with any medicines contributed to death. ‡ As several medicines may have been dispensed from the same class or detected post mortem for an individual, the value for this category is not the sum of the following two categories. § Dispensing records for detected medicines during the year before death but not during the estimated period of exposure were: antidepressant, 825 (53.8%); antipsychotic, 339 (43.1%); anxiolytic, 700 (33.4%); opioid, 495 (25.7%); and sedative, 307 (16.7%). |
|||||||||||||||
Received 3 November 2022, accepted 11 April 2023
- Kate M Chitty1,2
- Nicholas A Buckley1,3
- Jessy Lim1
- Zein Ali1
- Jennifer L Schumann4,5,6
- Rose Cairns1,3
- Benjamin Daniels7
- Sallie A Pearson7
- David B Preen2
- Andrea L Schaffer8
- 1 The University of Sydney, Sydney, NSW
- 2 The University of Western Australia, Perth, WA
- 3 Poisons Information Centre, Children's Hospital at Westmead, Sydney, NSW
- 4 Victorian Institute of Forensic Medicine, Monash University, Melbourne, VIC
- 5 Monash Addiction Research Centre, Monash University, Melbourne, VIC
- 6 Monash University, Melbourne, VIC
- 7 The University of New South Wales, Sydney, NSW
- 8 The Bennett Institute of Applied Data Science, University of Oxford, Oxford, United Kingdom
Open access:
Open access publishing facilitated by The University of Sydney, as part of the Wiley – The University of Sydney agreement via the Council of Australian University Librarians.
This study was funded by grants from the National Health and Medical Research Council (NHMRC; 1157757, 196900) and the Translational Australian Clinical Toxicology Research Group (TACT). Kate Chitty (1122362) and Andrea Schaffer (1158763) are supported by NHMRC Early Career Fellowships. Rose Cairns is supported by an NHMRC Investigator Grant (1196516). Benjamin Daniels is supported by a Cancer Institute NSW Early Career Fellowship (ECF1381). The funding organizations played no part in the design of the study, nor in the preparation, review, or approval of the manuscript.
We thank the National Coronial Information System (NCIS), managed by the Victorian Department of Justice and Community Safety, the Centre for Health Record Linkage (CHeReL), and the NSW Ministry of Health for their support for this investigation. We thank Services Australia for supplying the PBS data. We also thank the research assistants who aided the project: Daniel Chong, Jacob Crouse, Annabelle Chidiac, and Melissa Barron (University of Sydney).
No relevant disclosures.
If you or anyone you know is experiencing distress, please call Lifeline on 13 11 14 (www.lifeline.org.au) or Beyond Blue (www.beyondblue.org.au) on 1300 22 46 36.
- 1. Too LS, Spittal MJ, Bugeja L, et al. The association between mental disorders and suicide: a systematic review and meta‐analysis of record linkage studies. J Affect Disord 2019; 259: 302‐313.
- 2. Ferrari AJ, Norman RE, Freedman G, et al. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PLoS One 2014; 9: e91936.
- 3. Ahmedani BK, Peterson EL, Hu Y, et al. Major physical health conditions and risk of suicide. Am J Prev Med 2017; 53: 308‐315.
- 4. Miller TR, Swedler DI, Lawrence BA, et al. Incidence and lethality of suicidal overdoses by drug class. JAMA Netw 2020; 3: e200607.
- 5. Cairns R, Karanges EA, Wong A, et al. Trends in self‐poisoning and psychotropic drug use in people aged 5–19 years: a population‐based retrospective cohort study in Australia. BMJ Open 2019; 9: e026001.
- 6. Saini P, Chantler K, Kapur N. GPs’ views and perspectives on patient non‐adherence to treatment in primary care prior to suicide. J Ment Health 2018; 27: 112‐119.
- 7. Courtet P, Lopez‐Castroman J. Antidepressants and suicide risk in depression. World Psychiatry 2017; 16: 317‐318.
- 8. Molero Y, Larsson H, D'Onofrio BM, et al. Associations between gabapentinoids and suicidal behaviour, unintentional overdoses, injuries, road traffic incidents, and violent crime: population based cohort study in Sweden. BMJ 2019; 365: l2147.
- 9. Oliveira JM, Sobreira G, Velosa J, et al. Association of isotretinoin with depression and suicide: a review of current literature. J Cutan Med Surg 2018; 22: 58‐64.
- 10. Samyde J, Petit P, Hillaire‐Buys D, Faillie JL. Quinolone antibiotics and suicidal behavior: analysis of the World Health Organization's adverse drug reactions database and discussion of potential mechanisms. Psychopharmacology 2016; 233: 2503‐2511.
- 11. O'Neill S, Graham B, Ennis E. Prescribed pain and mental health medication prior to suicide: a population based case control study. J Affect Disord 2019; 246: 195‐200.
- 12. Reneflot A, Kaspersen SL, Hauge LJ, Kalseth J. Use of prescription medication prior to suicide in Norway. BMC Health Serv Res 2019; 19: 215.
- 13. Sinyor M, Howlett A, Cheung AH, Shayfer A. Substances used in completed suicide by overdose in Toronto: an observational study of coroner's data. Can J Psychiatry 2012; 57: 184‐191.
- 14. Methling M, Krumbiegel F, Hartwig S, et al. Toxicological findings in suicides: frequency of antidepressant and antipsychotic substances. Forensic Sci Med Pathol 2019; 15: 23‐30.
- 15. Chitty KM, Schumann JL, Schaffer A, et al. Australian Suicide Prevention using Health‐Linked Data (ASHLi): protocol for a population‐based case series study. BMJ Open 2020; 10: e038181.
- 16. Mellish L, Karanges EA, Litchfield MJ, et al. The Australian Pharmaceutical Benefits Scheme data collection: a practical guide for researchers. BMC Res Note 2015; 8: 634.
- 17. Australian Bureau of Statistics. 1270.0.55.005. Australian Statistical Geography Standard (ASGS), volume 5: remoteness structure, July 2016. 16 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005 (viewed Dec 2022).
- 18. Wylie CE, Daniels B, Brett J, et al. A national study on prescribed medicine use in Australia on a typical day. Pharmacoepidemiol Drug Saf 2020; 29: 1046‐1053.
- 19. Australian Institute of Health and Welfare. Suicide and self‐harm monitoring: Patterns of health service use in the last year of life among those who died by suicide. Updated Mar 2023. https://www.aihw.gov.au/suicide‐self‐harm‐monitoring/data/deaths‐by‐suicide‐in‐australia/health‐service‐use‐in‐the‐last‐year‐of‐life (viewed Jan 2023).
- 20. Australian Institute of Health and Welfare. Australia's health, 2014 (AIHW Cat. no. AUS 178). 25 June 2014. https://www.aihw.gov.au/reports/australias‐health/australias‐health‐2014/overview (viewed Jan 2023).
- 21. Valuck RJ, Orton HD, Libby AM. Antidepressant discontinuation and risk of suicide attempt: a retrospective, nested case–control study. J Clin Psychiatry 2009; 70: 1069‐1077.
- 22. Oliva EM, Bowe T, Manhapra A, et al. Associations between stopping prescriptions for opioids, length of opioid treatment, and overdose or suicide deaths in US veterans: observational evaluation. BMJ 2020; 368: m283.
- 23. Sørensen A, Juhl Jørgensen K, Munkholm K. Clinical practice guideline recommendations on tapering and discontinuing antidepressants for depression: a systematic review. Ther Adv Psychopharmacol 2022; 12: 20451253211067656.
- 24. Gomes T, Juurlink DN, Mamdani JM, et al. Prevalence and characteristics of opioid‐related deaths involving alcohol in Ontario, Canada. Drug Alcohol Depend 2017; 179: 416‐423.
- 25. Drummer OH, Kennedy B, Bugeja L, et al. Interpretation of postmortem forensic toxicology results for injury prevention research. Inj Prev 2013; 19: 284‐289.
- 26. Kennedy M. Interpreting postmortem drug analysis and redistribution in determining cause of death: a review. Pathol Lab Med Int 2015; 7: 55‐62.
- 27. Saar E, Gerostamoulos D, Drummer OH, Beyer J. Assessment of the stability of 30 antipsychotic drugs in stored blood specimens. Forensic Sci Int 2012; 215: 152‐158.






Abstract
Objectives: To determine the numbers and types of medicines dispensed around the time of death to people who die by suicide; to compare the medicines recently dispensed and those recorded in post mortem toxicology reports.
Design, setting, participants: Analysis of linked National Coronial Information System (NCIS) and Pharmaceutical Benefits Scheme (PBS) data from the Australian Suicide Prevention using Health Linked Data (ASHLi) study, a population‐based case series study of closed coronial cases for deaths of people in Australia aged ten years or more during 1 July 2013 – 10 October 2019 deemed by coroners to be the result of intentional self‐harm.
Main outcome measures: Proportions of people to whom medicines were dispensed around the time of death, by medicine group, class, and specific medicine; comparison of medicines recently dispensed and those detected by post mortem toxicology.
Results: Toxicology reports were available for 13 541 of 14 206 people who died by suicide (95.3%; 10 246 men, 75.7%); poisoning with medicines contributed to 1163 deaths (8.6%). At least one PBS‐subsidised medicine had been dispensed around the time of death to 7998 people (59.1%). For three medicine classes, the proportions of people in whom the medicines were detected post mortem and their death was deemed medicine‐related were larger for those without records of recent dispensing than for people for whom they had been dispensed around the time of death: antidepressants (17.7% v 12.0%), anxiolytics (16.3% v 14.8%), and sedatives/hypnotics (24.3% v 16.5%). At least one recently dispensed medicine not detected post mortem was identified for 6208 people (45.8%).
Conclusions: A considerable proportion of people who died by suicide were not taking psychotropic medicines recently dispensed to them, suggesting non‐adherence to pharmacotherapy, and a smaller than expected proportion were using antidepressants. Conversely, medicines that had not recently been dispensed were detected post mortem in many people for whom poisoning with medicines was a contributing factor, suggesting medicine stockpiling.