Healthy is one of the seven domains outlined in the Future Healthy Countdown 2030 framework on children and young people's health and wellbeing. The Countdown's framework draws on the Nest, a framework of wellbeing developed by the Australian Research Alliance for Children and Youth.1 In the 2021 iteration of the Nest, a new generation of child and youth voices defined healthy children and young people as those who “have their physical, mental, and emotional health needs met” and “receive appropriate health services, including preventative measures to address potential or emerging physical, emotional and mental health concerns”.1
The physical health and mental health of young Australians continue to benefit from advances in public health, modern medicine, preventive interventions such as vaccination, and a strong universal health care system. However, health inequities remain and the social determinants of health (eg, economic, commercial and structural factors) are strongly at play. Differential outcomes in children's and young people's health and wellbeing are recognised to be “unjust, unnecessary, systematic and preventable”.2 For these reasons, attempts to improve health outcomes in Australia and around the world must ensure that children and young people aged 0–24 years — particularly priority groups (eg, those who are Aboriginal and/or Torres Strait Islander and those living in low income households) — are front and centre of policy decisions aimed at reducing inequities.
A broad range of indicators can be used to track the health and wellbeing of young populations. Among these, unhealthy weight (overweight and obesity) and mental health problems and disorders are leading examples of health conditions that remain unacceptably high in young populations globally. These conditions are also inequitably distributed and significant risk factors for wider diseases and disorders across the lifespan.3 Weight problems often begin in the developmental years of childhood and adolescence.4,5 Similarly, half of mental health problems emerge by 18 years of age and almost two‐thirds emerge by 24 years of age.6 Addressing these two health priorities alone would reap major benefits, including improved quality of life and reduced risk of physical disease, with implications within and across generations.3 However, intervening to prevent weight and mental health problems early in the life course necessitates accurate population and clinical data on both of these outcomes, around aspects of public health and health services, ideally from early childhood through to young adulthood (ages 0–24 years).
Currently, there is no single survey system in Australia that provides these insights. However, Australia does have three survey systems that could be better integrated to regularly provide an epidemiological profile of the developmental years of Australians. These are the National Health Study (NHS; which collects data on Australians aged 2 years or older), the Australian Child and Adolescent Survey of Mental Health and Wellbeing (which collects data on 4–17‐year‐olds) and the National Study of Mental Health and Wellbeing (which collects data on Australians aged 16 years or older). Broader data capture across each survey system (including measures of social determinants and healthy development) has the potential to provide a more comprehensive and sustainable survey system for tracking the health of young populations. Furthermore, triennial administration of each survey could provide the necessary frequency for “state of the nation” reports that could enhance investments in timely, evidence‐based policy and practice decisions that are intended to improve the health of children and young people across our nation.
Tracking data on overweight and obesity in young populations
Current generations of children and young people are more likely to live with overweight or obesity than people at the same age in previous generations (Box 1).7 This burden is even greater among particular populations, such as those aged 5–14 years who live in the lowest socio‐economic areas (28%) or are of Aboriginal and/or Torres Strait Islander origin (38%).7 The National Obesity Strategy 2022–2032 has set a target of reducing overweight and obesity in 2–17‐year‐olds by at least 5% by 2030.8
If we are serious about reducing overweight and obesity by 5%, we need to reliably measure weight in young populations and its determinants to track progress and evaluate intervention and policy efforts. High quality and frequently collected data on body mass index (BMI; height and weight) of children and young people are available in the NHS, from in‐person objective measurements taken every three to four years (except in 2020–21 due to the coronavirus disease 2019 [COVID‐19] pandemic).9 The most recent NHS data, from 2017–18, estimated that almost one in four 5–14‐year‐old Australians (24%) and two in five 15–24‐year‐old Australians (41%) were either overweight or obese.7 In the 22 years since data were first collected, in 1995, these rates have risen by 20% for those aged 5–14 years and 46% for those aged 15–24 years (Box 1).
We also need to regularly measure key risk factors and protective factors for overweight and obesity, such as physical activity, sleep and nutrition. The National Nutrition and Physical Activity Survey was completed during the period 2011–2012 and is being administered again in 2023 — a decade later.10 We suggest that more frequent data on these key factors are needed to better track the results of previous policy and intervention decisions.
Beyond individual factors, we need to measure the key social, structural and commercial determinants of obesity, such as community factors. Community differences in the number of child development risk factors (eg, neighbourhood alcohol availability, school suspension, family conflict and peer bullying) predict significant increases in child weight status (eg, four or more risk factors increase the odds of a child being overweight by 50%) and other outcomes such as poor mental health.11 Broader structural factors offer policy targets that can have far reaching consequences. For example, a tax on sugary sweetened beverages alone is estimated to help reduce obesity rates at the population level by at least 2%.12 To be maximally effective in supporting evidence‐based decision making, we need to find ways of capturing macro level policy settings to help reduce obesogenic environments.
Tracking data on mental health difficulties and disorders in young populations
Young Australians continue to rate mental health concerns as a major challenge for their generation,13 with some groups dealing with greater burden than others (eg, LGBQTI+ and Aboriginal and Torres Strait Islander children and young people).14,15 Despite this, nationally representative and community data on mental health are collected too infrequently to develop the coherent picture of developmental years that is needed to evaluate current policies and inform approaches to mental health promotion in young populations.
Like the NHS, the Australian Child and Adolescent Survey of Mental Health and Wellbeing and the National Study of Mental Health and Wellbeing have the potential to provide a continuous picture of mental health difficulties and disorders across the developmental years. These population representative mental health survey systems collect data on mental health difficulties (distress) and mental disorders (clinical conditions).
In the most recent Australian Child and Adolescent Survey of Mental Health and Wellbeing, which was administered a decade ago (during the period 2013–2014), one in five 11–17‐year‐olds (20%) reported high or very high levels of psychological distress using the Kessler 10 Psychological Distress Scale (K10)16 (no equivalent data are available for children younger than 11 years). This compares to almost one in seven 4–17‐year‐olds (14%) who were classified as having a diagnosable mental disorder in the previous 12 months using the Diagnostic Interview Schedule for Children version IV (DISC‐IV).16 The absence of a more recent survey means that there is a striking gap in data for one of the most important public health and health service priorities for children and young people.17
More recent estimates of mental health difficulties are available for those aged 16 years or older in the larger national cohort (2020–2021). However, estimates of psychological distress are presented within wide age bands (16–34 years) which are not likely to represent those aged 16–24 years.18 Tighter age disaggregation is available for mental disorders (rather than mental health distress), with two in five 16–24‐year‐olds (40%) classified as having a mental disorder in the previous 12 months using the Composite International Diagnostic Interview (CIDI).19 In this age group, anxiety and affective disorders have steadily increased since national data were first collected in 1997 (Box 2), while substance use disorders have substantially declined.19,20,21
Driving responsive and accountable action for physical and mental health
An important picture of physical health (overweight and obesity) and mental health (distress and disorder) in young populations can be assembled by bringing together data from the NHS, the Australian Child and Adolescent Survey of Mental Health and Wellbeing, and the National Study of Mental Health and Wellbeing. However, these important and high quality survey systems are not currently designed to “talk with each other” and thereby fail to provide a single, coherent picture of health and development in young populations at regular intervals.
In addition, there is an important gap in data relating to early childhood and there is no tracking of positive health and developmental outcomes, including good general health, pro‐social behaviour and pro‐environmental behaviour. Yet, measuring the development of these positive types of behaviour has the potential to provide a crucial read on the key attitudes and behaviours that we need to nurture in young populations to ensure kinder, more peaceful societies and a healthier planet into the future.
Similarly, the broader social determinants of both positive and problematic outcomes are not assessed. Beyond tracking mental health outcomes, tracking modifiable risk factors and protective factors provides specific targets for public health investments in preventive interventions in addition to health services.
For this Countdown series, we suggest connecting these three important Australian survey systems to assemble an early life course national data system capable of providing continuous developmental data (up to age 24 years) on indicators of both physical and mental health. We also suggest more frequent administration of surveys (eg, triennially) with particular attention to measuring the primary social determinants of health and wellbeing and positive measures. Capitalising on the strengths of these national survey systems would address a major gap in data using expertise and infrastructure already in place within a nationally funded system. This could be done in a way that builds on existing assets (adding brief and reliable measures) but does not interfere with the core elements of these surveys which enable international comparisons.
Beyond these potential data capture extensions, there is a broader question of data utilisation, particularly concerns about how effectively population data are used. One important barrier to data utilisation relates to the ease with which non‐scientific audiences can make sense of complex, multidimensional data, in ways that lead to clarity about how and when to invest for maximum impact. With this in mind, we further suggest investment in a centralised data visualisation capability that places data on a single platform, to create a single “point of truth” that can be accessed by a broad range of end users. A leading example of this has been developed by the Institute for Health Metrics and Evaluation to visualise Global Burden of Disease estimates.
Summary and recommendations
The current state of play is summarised in Box 3. We make the following three recommendations around strengthening existing surveillance platforms and building new surveillance capabilities to help improve physical and mental health of young Australians.
1. Track BMI and mental health difficulties and disorders in young populations every three years
- Continue regular ongoing reporting of physical health, including overweight and obesity (BMI) from the NHS (measured from 2 years of age onward).
- Integrate child, adolescent and adult mental health and wellbeing survey data to provide a single, coherent picture of the early life course (up to age 24 years).
- Increase the frequency of mental health survey administration to match the triennial frequency of the NHS to ensure best practice coverage of major shifts in population health.
2. Extend and enrich surveys to assess modifiable developmental determinants
- Lower the starting age of the Australian Child and Adolescent Survey of Mental Health and Wellbeing to match that of the NHS (from two years of age onward, parent report up to age ten years) to ensure better coverage of young children.
- Extend the scope of mental health assessment to include brief high level indicators of positive development, including pro‐social and pro‐environmental behaviour.
- Enrich monitoring with regular population reads on common, modifiable determinants (individual, relational and contextual risk factors, protective factors and structural influences).
- Continue to ensure oversampling of priority groups and communities to drive more equitable health outcomes based on proportionate universalism.22
3. Invest in platforms that developmentally connect and visualise data
- Ensure that data can be visualised easily and developmentally (eg, use fine‐grained age disaggregation and community profiles) to ensure optimal data utilisation by governments, researchers and community leaders.
- Ensure that data on modifiable determinants of positive and problematic health outcomes are likewise easily accessible to optimise intervention planning.
- Ensure that all data collected are aligned with FAIR (findable, accessible, interoperable and reusable) and Open Science principles for data access and utilisation.
We believe that such improvements would build a foundation for responsive and accountable actions towards improving the physical and mental health of young Australians.
Box 1 – Proportion of children, adolescents and young adults aged 5–24 years living with overweight or obesity, by birth cohort and age group (measured in 1995, 2007–08 and 2017–18)
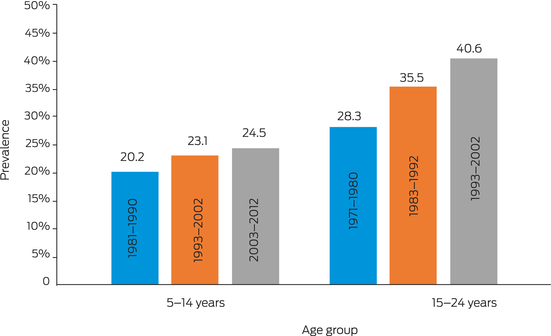
Source: Adapted from the Australian Institute of Health and Welfare.7
Box 2 – Prevalence of 12‐month mental disorders in young people aged 16–24 years, by time (1997, 2007, 2020–21)*
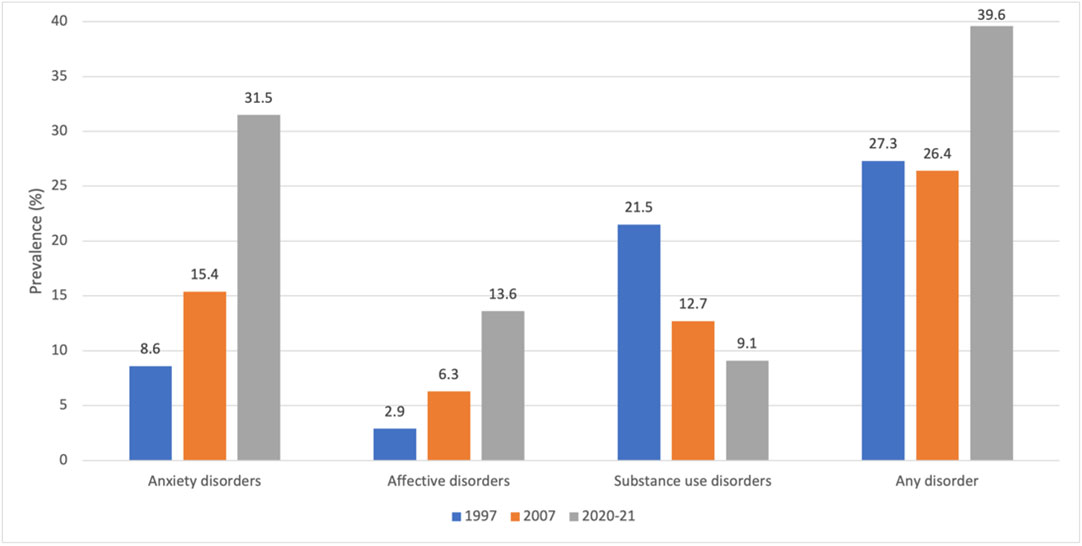
* Original figure produced using the data sources below. Data from 1997 are not directly comparable to data from 2007 and 2020–21 because the 1997 data are based on sampling of Australians aged 18–24 years old (not 16–17 years old) using an earlier version of the Composite International Diagnostic Interview (CIDI). Source: ABS National Study of Mental Health and Wellbeing, measured in 1997, 2007 and 2020–21.19,20,21
Box 3 – Pressing issues and key indicators of physical and mental health of Australians aged 0–24 years
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
Provenance: Commissioned; externally peer reviewed.
- 1. Goodhue R, Dakin P, Noble K. What's in the Nest? Exploring Australia's wellbeing framework for children and young people. Canberra: Australian Research Alliance for Children and Youth, 2021. https://www.aracy.org.au/documents/item/700 (viewed July 2023).
- 2. Royal Australasian College of Physicians. Inequities in child health position statement. Sydney: RACP, 2018. https://www.racp.edu.au/docs/default‐source/advocacy‐library/racp‐inequities‐in‐child‐health‐position‐statement.pdf (viewed July 2023).
- 3. Patton GC, Olsson CA, Skirbekk V, et al. Adolescence and the next generation. Nature 2018; 554: 458‐466.
- 4. Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011; 365: 1876‐1885.
- 5. World Health Organization. Noncommunicable diseases: childhood overweight and obesity. https://www.who.int/news‐room/questions‐and‐answers/item/noncommunicable‐diseases‐childhood‐overweight‐and‐obesity (viewed July 2023).
- 6. Solmi M, Radua J, Olivola M, et al. Age at onset of mental disorders worldwide: large‐scale meta‐analysis of 192 epidemiological studies. Mol Psychiatry 2022; 27: 281‐295.
- 7. Australian Institute of Health and Welfare. Overweight and obesity among Australian children and adolescents [Cat. No. PHE 274]. Canberra: AIHW, 2020. https://www.aihw.gov.au/getmedia/ac61b7d7‐7991‐4e15‐8fa6‐a7973479fa8b/aihw‐phe‐274.pdf?inline=true (viewed July 2023).
- 8. Health Ministers Meeting. The National Obesity Strategy 2022–2032: at a glance. Commonwealth of Australia, 2022. https://www.health.gov.au/sites/default/files/documents/2022/03/national‐obesity‐strategy‐2022‐2032‐at‐a‐glance‐summary‐with‐a‐strategy‐map_1.pdf (viewed July 2023).
- 9. Australian Institute of Health and Welfare. Overweight and obesity: technical notes. https://www.aihw.gov.au/reports/overweight‐obesity/overweight‐and‐obesity/contents/technical‐notes (viewed July 2023).
- 10. Australian Bureau of Statistics. Intergenerational Health and Mental Health Study (IHMHS). https://www.abs.gov.au/about/key‐priorities/ihmhs (viewed Sept 2023).
- 11. Williams JW, Canterford L, Toumbourou JW, et al. Social development measures associated with problem behaviours and weight status in Australian adolescents. Prev Sci 2015; 16: 822‐831.
- 12. Australian Medical Association. A tax on sugar‐sweetened beverages: modelled impacts on sugar consumption and government revenue. Canberra: AMA, 2021. https://www.ama.com.au/articles/tax‐sugar‐sweetened‐beverages‐what‐modelling‐shows‐0 (viewed Sept 2023).
- 13. Leung S, Brennan N, Freeburn T, et al. Youth survey report 2022. Sydney: Mission Australia, 2022. https://www.missionaustralia.com.au/what‐we‐do/research‐impact‐policy‐advocacy/youth‐survey (viewed July 2023).
- 14. Brennan N, Beames JR, Kos A, et al. Psychological distress in young people in Australia. Fifth biennial youth mental health report: 2012–2020. Sydney: Mission Australia, 2021. https://apo.org.au/sites/default/files/resource‐files/2021‐09/apo‐nid313947.pdf (viewed July 2023).
- 15. Strauss P, Cook A, Winter S, et al. Trans Pathways: the mental health experiences and care pathways of trans young people. Summary of results. Perth: Telethon Kids Institute, 2017. https://www.telethonkids.org.au/globalassets/media/documents/brain‐‐behaviour/trans‐pathwayreport‐web.pdf (viewed July 2023).
- 16. Lawrence D, Johnson S, Hafekost J, et al. The mental health of children and adolescents. Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Canberra: Department of Health, 2015. https://www.health.gov.au/sites/default/files/documents/2020/11/the‐mental‐health‐of‐children‐and‐adolescents_0.pdf (viewed July 2023).
- 17. Australian Psychological Society. Aussie kids’ mental health and wellbeing. https://psychology.org.au/for‐members/news‐and‐updates/news/2022/aussie‐kids‐mental‐health‐and‐wellbeing (viewed July 2023).
- 18. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020; 7: 883‐892.
- 19. Australian Bureau of Statistics. National Study of Mental Health and Wellbeing (reference period: 2020–2022). https://www.abs.gov.au/statistics/health/mental‐health/national‐study‐mental‐health‐and‐wellbeing/latest‐release (viewed July 2023).
- 20. McLennan W. Mental health and wellbeing: profile of adults, Australia 1997 (ABS Cat. No. 4326.0). Canberra: Australian Bureau of Statistics, 1998. https://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/CA25687100069892CA25688900233CAF/$File/43260_1997.pdf (viewed July 2023).
- 21. Australian Bureau of Statistics. National Study of Mental Health and Wellbeing: summary of results (reference period: 2007). https://www.abs.gov.au/statistics/health/mental‐health/national‐study‐mental‐health‐and‐wellbeing/2007 (viewed July 2023).
- 22. Marmot M, Allen J, Boyce T, et al. Health equity in England: the Marmot Review 10 years on. London: Institute of Health Equity, 2020. https://www.instituteofhealthequity.org/resources‐reports/marmot‐review‐10‐years‐on/the‐marmot‐review‐10‐years‐on‐full‐report.pdf (viewed Sept 2023).






Open access:
Open access publishing facilitated by Deakin University, as part of the Wiley – Deakin University agreement via the Council of Australian University Librarians.
This article is part of the MJA supplement on the Future Healthy Countdown 2030, which was funded by the Victorian Health Promotion Foundation (VicHealth) — a pioneer in health promotion that was established by the Parliament of Victoria as part of the Tobacco Act 1987, and an organisation that is primarily focused on promoting good health and preventing chronic disease for all. VicHealth has played a convening role in scoping and commissioning the articles contained in the supplement.
No relevant disclosures.