The mental health of children and adolescents was harmed by the coronavirus disease 2019 (COVID‐19) pandemic, partly because of reduced access to social and wider family support networks and disruptions to school‐based services.1 The prescribing of psychotropic medications by general practitioners, 84.7% of mental health‐related prescribing in Australia,2 is a key indicator of mental health care activity.
We examined rates of psychotropic medication prescribing (antidepressants, antipsychotics, anxiolytics, psychostimulants, and hypnotics and sedatives) by general practitioners for children and adolescents aged 5–19 years in two metropolitan primary health networks (PHNs) in New South Wales (272 general practices) and one regional and two metropolitan PHNs in Victoria (388 general practices) during 1 January 2018 – 30 November 2021. Outcome Health used the POpulation Level Analysis and Reporting tool (POLAR) to extract medications and patient data from general practice electronic health records. POLAR is used in primary health networks for decision support during consultations (for example, prompts for missing patient details, algorithms for risk of hospital admission, vaccination advice) and for quality care initiatives.3 The practice data we analysed is routinely collected for quality assurance, clinical governance, and approved research purposes. We fitted a seasonally adjusted autoregressive integrated moving average (SARIMA) model to pre‐pandemic prescribing data (1 January 2018 – 29 February 2020) and used it to forecast prescribing during the pandemic period (1 March 2020 – 30 November 2021) (further details: Supporting Information). The Royal Australian College of General Practitioners national research and evaluation ethics committee approved data collection (17‐008), the Macquarie University human research ethics committee approved the study (52020675617176).
A total of 1 423 518 children (720 980 boys, 51%) had consultations at the 660 included practices during the study period; antidepressants were prescribed for 22 479 (1.6%), antipsychotics for 5247 (0.4%), hypnotics and sedatives for 6582 (0.5%), anxiolytics for 3321 (0.2%), and psychostimulants for 7450 children and adolescents (0.5%) (Supporting Information, tables 1 and 2). Prescribing rates during the COVID‐19 pandemic period were higher for all psychotropic types than predicted by SARIMA modelling of 2018–20 data. Increased prescribing of antidepressants and stimulants was most marked for children aged 5–9 years; psychostimulant prescribing peaked during March 2020 for older children (10–14 years) and adolescents (15–19 years). Increased prescribing of anxiolytic medications was most marked for younger children and adolescents. The increase in antipsychotic prescribing was more marked for children (5–14 years) than for adolescents; prescribing of hypnotics and sedatives increased for younger children and adolescents during the second half of 2020 (Box). The proportion of prescriptions with five repeats markedly increased from 8721 of 89 651 (9.7%) in February 2020 to 15 579 of 106 176 (14.7%) in March 2020, while the proportion without repeats declined from 62 391 (69.6%) to 67 948 (64.1%) (Supporting Information, figure 1).
Limitations of our study include the uncertain representativeness of the analysed data, our reporting of rates for 5‐year age groups rather than individual years, and the fact that some psychotropic medications can be prescribed for reasons other than mental health care. We had no information about whether prescribed medications were dispensed or taken, nor about prescribing by other medical practitioners (apart from prescriptions by general practitioners in shared care or similar arrangements with specialists).
We found that the prescribing of psychotropic medications for children and adolescents in general practice has increased since 2018. Particularly marked increases were noted during the COVID‐19 pandemic, consistent with its impact on mental health. Another Australian study reported that prescribing of antidepressants (all age groups) was 68% higher in March 2020 than in February 2020 (and dispensing 15% higher).4 Increased prescribing in general practice may be partly explained by the increased burden on other mental health services; longer waiting times and more difficult access to paediatric psychologist and psychiatric services led to greater reliance on general practitioners.5 The move to telehealth consultations may also have altered general practitioners’ prescribing behaviour.
Our findings suggest that the capacity of the Australian health care system to increase mental health care provision during a time of crisis is inadequate, the consequently key role of general practice in this area, and the particular importance of improving mental health support for children and adolescents.
Data availability
The study data cannot be publicly shared for reasons of ethics and privacy. Access, however, may be granted upon request to Rae‐Anne Hardie if deemed appropriate.
Box – Prescribing of psychotropic medications to children and adolescents at 272 New South Wales and 388 Victorian general practices, 1 January 2018 – 30 November 2021: monthly rates, by medication type and age group*
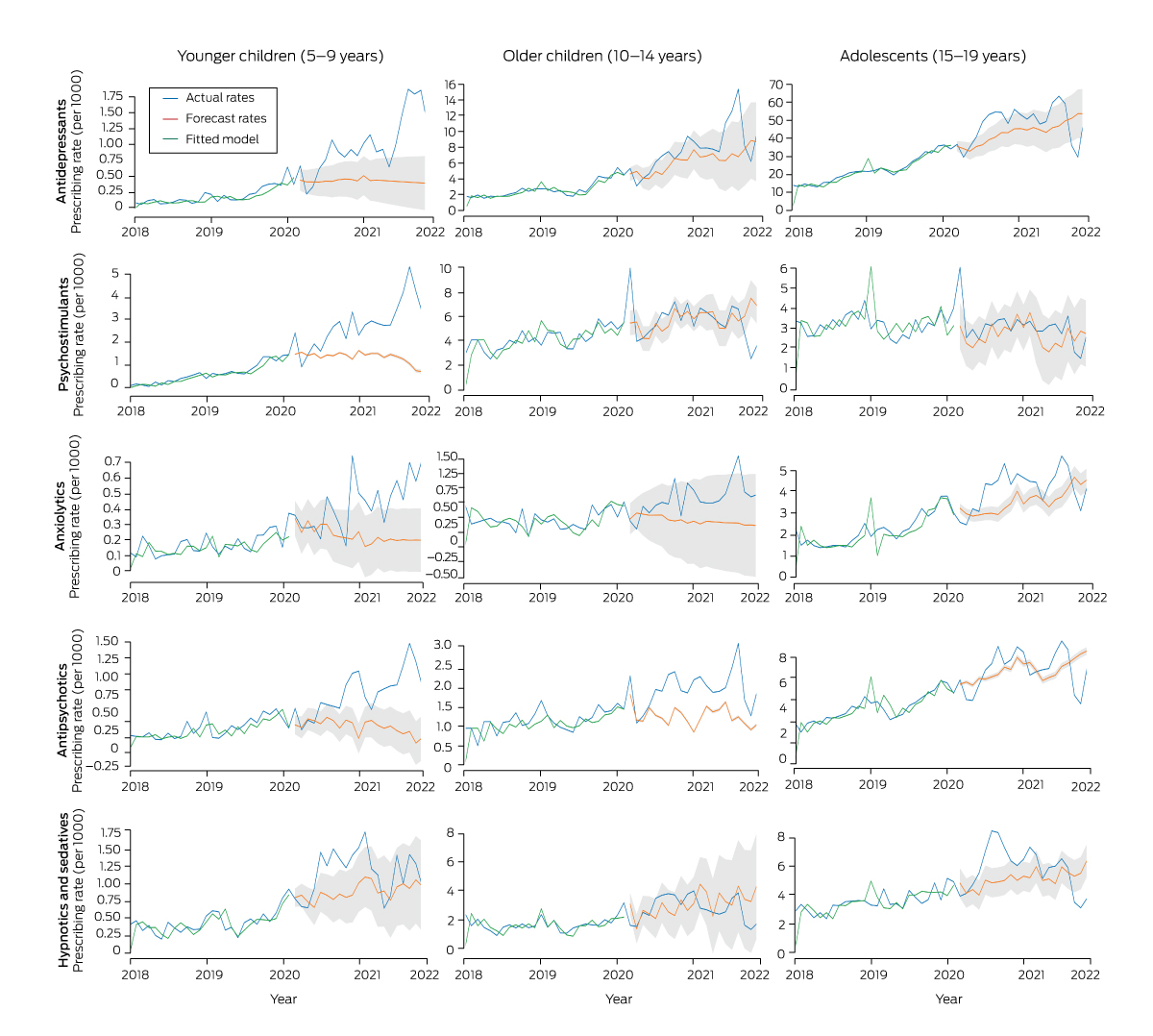
* Forecast rates during the coronavirus disease (COVID‐19) pandemic period (with 95% confidence interval shadowed) are based on the seasonally adjusted autoregressive integrated moving average (SARIMA) model fitted to the prescribing data for January 2018 – February 2021.
Received 25 October 2022, accepted 5 April 2023
- 1. Lee J. Mental health effects of school closures during COVID‐19. Lancet Child Adolesc Health 2020; 4: 421.
- 2. Australian Institute of Health and Welfare. Mental health: mental health‐related prescriptions. Updated 30 Jan 2023. https://www.aihw.gov.au/mental‐health/topic‐areas/mental‐health‐prescriptions (viewed Apr 2023).
- 3. Pearce C, McLeod A, Rinehart N, et al. What a comprehensive, integrated data strategy looks like: the Population Level Analysis and Reporting (POLAR) program. Stud Health Technol Inform 2019; 264: 303‐307.
- 4. Tscharke BJ, Hollingworth S, van Driel ML, et al. The impact of COVID‐19 on antidepressant sales and prescription dispensing in Australia [letter]. Aust N Z J Psychiatry 2022; 56: 871‐872.
- 5. Australian Psychological Society. 1 in 3 psychologists are unable to see new clients, but Australians need help more than ever [news]. 24 Feb 2022. https://psychology.org.au/for‐members/publications/news/2022/australians‐need‐psychological‐help‐more‐than‐ever (viewed Apr 2023).






Open access
Open access publishing facilitated by Macquarie University, as part of the Wiley – Macquarie University agreement via the Council of Australian University Librarians.
The study was funded by the Digital Health Cooperative Research Centre (grant DHCRC‐01180), which is funded by the Australian government through the Cooperative Research Centres (CRC) Program. The funders played no role in the design or interpretation of the findings and researchers were independent from the funder.
No relevant disclosures.