In December 2022, rising numbers of group A Streptococcus (GAS) infections were reported in the United Kingdom, Europe, and the United States.1 Clinical syndromes caused by GAS range from pharyngitis and scarlet fever to necrotising fasciitis and toxic shock syndrome. The mortality rate among people with invasive GAS (iGAS) infections, in which GAS can be isolated from a normally sterile tissue (eg, blood), is 12%.2 GAS infections are seasonal, their number rising in winter and peaking in spring.1 During the 2020–2021 coronavirus disease 2019 (COVID‐19)‐related restrictions, GAS infection rates fell to very low levels in many countries.1 Outbreaks in the northern hemisphere in 2022 may reflect an early return to pre‐pandemic seasonal patterns, or a post‐pandemic change in the epidemiology of GAS infection.
Corresponding data for southern hemisphere countries have not been reported. On 23 December 2022, the Victorian Department of Health issued an advisory notice regarding rising iGAS case numbers in Victoria and overseas.3 However, longitudinal public health data are limited. iGAS has been nationally notifiable since 1 July 2021,4 and notifications have been received in Victoria since February 2022. Only limited data on non‐invasive GAS infection are available, as it is not notifiable.
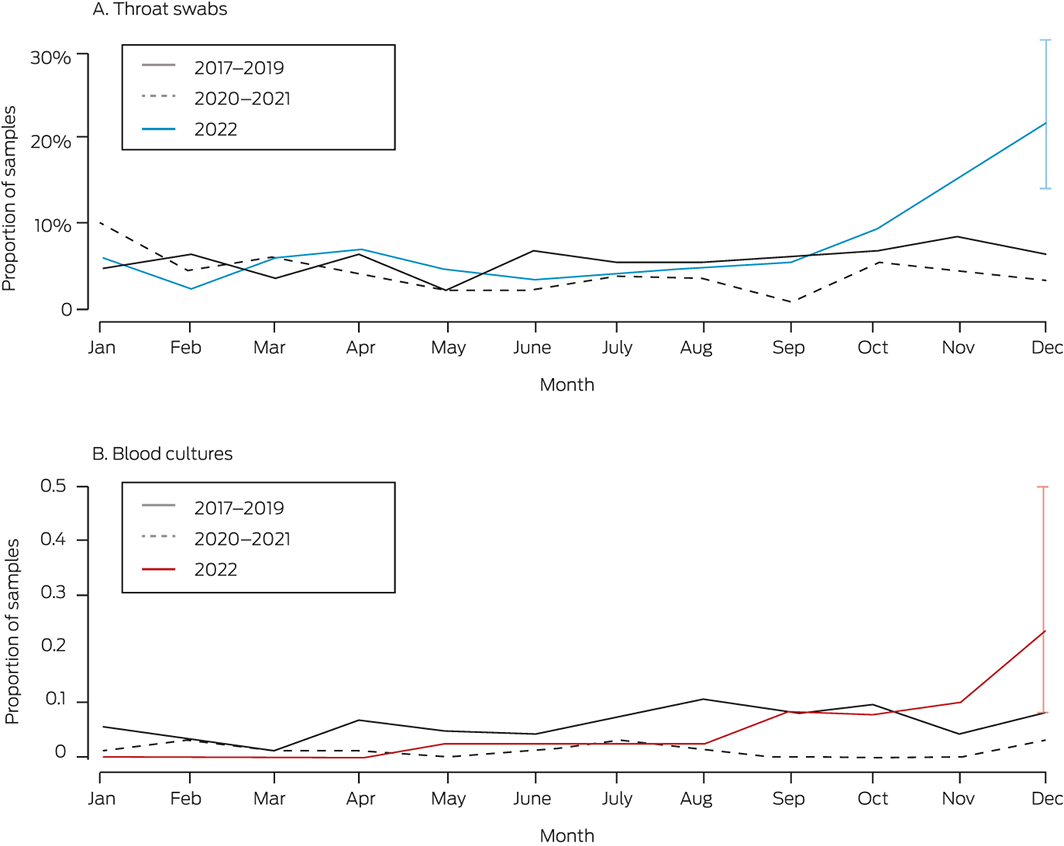
We examined the results of throat swabs and blood cultures processed by Monash Pathology during 1 January 2017 – 20 December 2022. Monash Pathology provides services to a catchment area of about 1.5 million people in Melbourne, including the Monash Health network with its more than 2000 hospital beds (adult and children) and outpatient services. We compared monthly GAS isolation rates during 2022 with the mean monthly rates for 2017–2019 (ie, three years preceding the COVID‐19 period) and the mean monthly rates during 2020–2021 (ie, two years during which social distancing restrictions applied). We estimated 95% confidence intervals using the Clopper–Pearson exact method. All analyses were performed in Stata 17.0. The Monash Health Ethics Advisory Group approved our analysis as a minimum risk/quality assurance study (QA/94180/MonH‐2023‐352627(v1)).
Rates of GAS isolation in Melbourne began to rise in November 2022, and were substantially higher than pre‐pandemic levels in December 2022. During 1–20 December 2022, GAS was isolated from 20 of 92 throat swabs (22%) and six of 2597 blood cultures (0.2%); during the corresponding months of 2017–2019 it had been isolated from 13 of 193 swabs (6.7%; v 2022) and nine of 11 013 blood cultures (0.08%) (Box; Supporting Information, table 1). Most GAS‐positive samples were collected in hospital emergency departments or wards (throat swabs: 252 of 296, 85%; blood cultures: 113 of 114, 99%).
During 2017–2022, the median age of people with streptococcal throat infections was eight years (interquartile range [IQR], 5–21 years), of those with bacteraemia 48 years (IQR, 33–65 years). During 2022, the median age of people with positive swabs was eight years (IQR, 5–23 years), of those with positive blood cultures 52 years (IQR, 18–68 years) Four of the twenty bacteraemia cases in 2022 were in children under ten years of age (Supporting Information, figure 1). During the December 2022 surge, the median age of people with positive throat swabs was six years (IQR, 4.5–15 years; sixteen under 18 years, ten aged five years or younger); the median age of those with positive blood cultures was 43 years (IQR, 11–64 years; two under 18 years, none aged five years or less).
The twenty blood culture isolates collected during 2022 were subjected to M‐protein gene (emm) typing, a technique for defining the clonal structure of GAS populations.5 emm type diversity (ten emm types) indicated a non‐clonal outbreak; the most frequent type was emm 1.0 (five isolates). There were four emm types in the six blood culture isolates of December 2022.
The role of viral co‐infection, reduced GAS exposure, and reduced accrual of natural immunity during 2020–2021 (including 263 days of stay‐at‐home orders) in this rise in GAS disease in Melbourne warrant further investigation. Respiratory viral infection case numbers fell to very low levels, then rose after restrictions were lifted.6 A spike in GAS infection numbers during 2017 (in our catchment area: lower than the December 2022 rise; Supporting Information, figure 2) coincided with high rates of influenza A infection.7
Overseas media attention during December 2022 may have contributed to increased case finding (ascertainment bias), but GAS test numbers during 2022 were similar to the pre‐pandemic numbers (Supporting Information, table 2). More comprehensive data from Victoria and elsewhere should be examined.
Our single laboratory analysis found that the numbers of GAS isolates from throat swabs markedly increased in December 2022, reaching triple the mean pre‐pandemic December rate and double the mean pre‐pandemic winter and spring peak rates (6.7% for June 2017–2019; 8.4% for November 2017–2019). This suggests a surge in GAS throat infections, primarily in children. A parallel spike in invasive disease affecting both children and older adults was also noted. Our findings, together with northern hemisphere reports, possibly reflect a worldwide increase in GAS disease. Clinicians should be alert to clinical syndromes of GAS/iGAS infection, and be familiar with recommendations for treating infected people and with chemoprophylaxis for their close contacts.
Received 10 January 2023, accepted 20 March 2023
- 1. Venkatesan P. Rise in group A streptococcal infections in England. Lancet Respir Med 2023; 11: e16.
- 2. Nelson GE, Pondo T, Toews KA, et al. Epidemiology of invasive group A streptococcal infections in the United States, 2005–2012. Rev Infect Dis 2016; 63: 478‐486.
- 3. Victorian Department of Health. Health warning on invasive group A streptococcal disease 2022. Updated 23 Dec 2022. https://www.health.vic.gov.au/health‐advisories/health‐warning‐on‐invasive‐group‐a‐streptococcal‐disease (viewed Jan 2023).
- 4. Australian Department of Health and Aged Care. Group A streptococcal disease – invasive (iGAS). Updated 14 June 2022. https://www.health.gov.au/diseases/group‐a‐streptococcal‐disease‐invasive‐igas?language=en (viewed Jan 2023).
- 5. Miller KM, Lamagni T, Cherian T, et al. Standardization of epidemiological surveillance of invasive group A streptococcal infections. Open Forum Infect Dis 2022; 9 (Suppl 1): S31‐S40.
- 6. Victorian Department of Health. Victoria, local public health areas and local government areas surveillance summary report 2023. Updated 8 Aug 2022. https://www.health.vic.gov.au/infectious‐diseases/local‐government‐areas‐surveillance‐report (viewed Jan 2023).
- 7. Oliver J, Wilmot M, Strachan J, et al. Recent trends in invasive group A Streptococcus disease in Victoria. Commun Dis Intel (2018) 2019; 43.






Open access
Open access publishing facilitated by Monash University, as part of the Wiley – Monash University agreement via the Council of Australian University Librarians.
We thank the Microbiological Diagnostic Unit Public Health Laboratory, Melbourne, for performing emm typing of blood culture isolates.
No relevant disclosures.