Clinical record
A 39‐year‐old, fully independent woman with a past medical history of migraines, managed with rizatriptan as required, presented to the emergency department (ED) with a 2‐week history of mild right‐sided neck pain. The pain started after a rapid head turn to the left upon waking from sleep. It had initially improved but later worsened after another rapid head rotation to the left. This resulted in a sudden, sharp, right‐sided posterior neck pain, a throbbing headache, and paraesthesiae of the right arm and leg. The headache resembled her usual migraine symptoms of pulsatile pain and photophobia, so she took rizatriptan. She presented to the ED due to sensory symptoms that were not normally part of her migraine attacks. In the ED, she developed right upper and lower limb weakness and worsening paraesthesiae.
On initial assessment, she had a normal neurological examination except for reduced light touch sensation in her right upper and lower limbs. However, on re‐assessment 4 hours later, she had developed mild pyramidal weakness, affecting the right upper and lower limbs. She also had right‐sided finger to nose and heel to shin dysmetria, and right upper limb drift, in addition to persisting right‐sided sensory deficit. There were no abnormal neurological signs in the left upper or lower limbs. Gait was slow and tentative due to right leg sensory ataxia. Cranial nerve examination remained normal, with no facial weakness or sensory deficit.
Investigation with computed tomography (CT) scan of the brain did not reveal any intracranial abnormalities, but a computed tomography angiogram (CTA) showed a small calibre right vertebral artery (Box). A magnetic resonance imaging (MRI) scan of the neck and a magnetic resonance angiography were performed and confirmed a hypoplastic right vertebral artery with dissection causing a right posterolateral cervical cord infarct at the level of C2. A further contrast MRI scan of the brain and the cervical spine did not reveal any other lesions. There was no contrast enhancement in the cervical cord lesion to suggest an acute inflammatory process.
Blood tests for stroke risk factors including diabetes mellitus, dyslipidaemia, thrombophilias and vasculitic disorders were negative. She was commenced on high dose statin and dual antiplatelet therapy. Due to her symptoms of fatigue, right‐sided weakness and impaired gait, she spent 4 days in inpatient rehabilitation.
A repeat MRI scan performed 3 months after dissection showed a persistent hypoplastic right vertebral artery and subtle hyperintensity on T2‐weighted‐fluid‐attenuated inversion recovery in the right posterior hemicord, consistent with a resolving right hemicord infarction.
On review at that time, she reported symptoms improvement overall but was experiencing ongoing right upper and lower limb paraesthesiae, mild weakness in the right lower limb, and fatigue. Nine months after the dissection, she had returned to her office‐based employment.
Discussion
This case highlights a rare but important diagnostic challenge. A known migraineur presented with symptoms of her typical migraine but developed ipsilateral limb sensory and motor deficits without facial involvement. Although these symptoms may be present in migraine with aura,1 in this case, they were due to vertebral artery dissection leading to cervical cord infarction.
In migraine with sensory aura, headache and/or neck pain and limb heaviness tend to be ipsilateral. Conversely, in most brain lesions, including some strokes, pain from the lesion itself, or from arterial dissection leading to infarction, is usually contralateral to the weak and/or numb side. In this case, the diseased right vertebral artery was first detected on a brain CTA performed as an urgent investigation for stroke. The sensory and motor signs were ipsilateral to the vertebral artery dissection, motivating the clinical team to consider upper cervical cord infarction. Right dorsal cervical cord infarction was confirmed on MRI. Because the central nervous system territory involved is caudal to the sensory and motor decussations in the lower medulla, limb weakness was ipsilateral to the infarct. The infarct was dorsal within the cord, so dorsal column (uncrossed) sensory pathway disruption caused ipsilateral sensory loss.
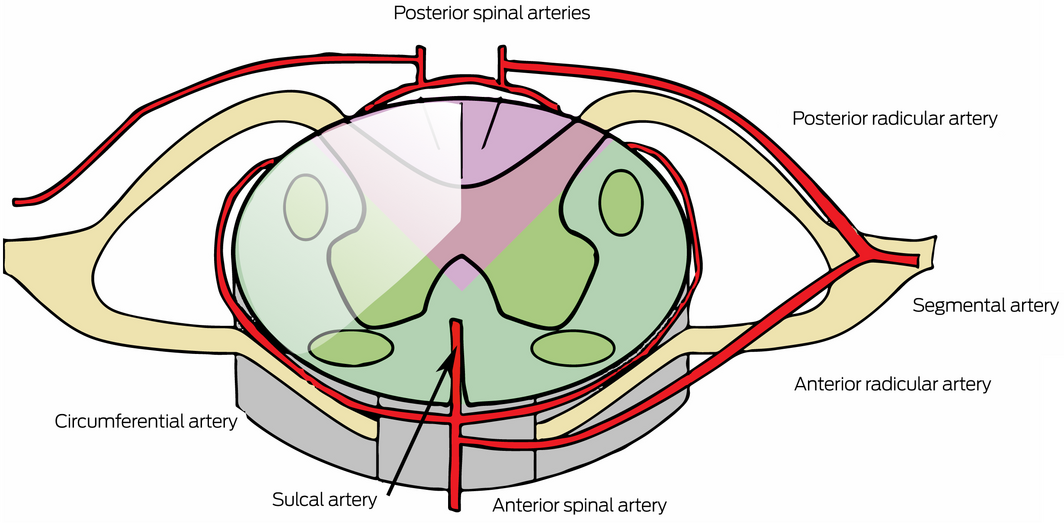
Spinal cord infarction is uncommon — estimated to account for only 1% of strokes.2 Although 11% of cord infarctions in one large series related to vertebral artery dissection, none of these was referrable to posterior spinal arteries, reflecting the rarity of this clinical syndrome.2 The posterior third of the cord — the site of the infarct in this case — is supplied by the single or paired posterior spinal arteries (Box), which arise from the distal vertebral arteries and are variably augmented in many vertebral segments by paired posterior radicular arteries.3 In this case, vertebral dissection is likely to have led to occlusion of the origin of the right posterior spinal artery and/or one or more high cervical posterior radicular branches. Cervical cord infarcts have the potential to cause significant disability.4 They should be considered in individuals presenting with neck pain or headache with ipsilateral neurological signs or symptoms. This case serves as a reminder that vertebral artery dissection and cervical cord infarction are diagnoses not to be missed.
Lessons from practice
- Careful clinical assessment is indicated in migraineurs to differentiate between migraine and more serious neurological pathologies.
- In migraine with sensory aura, headache and/or neck pain and limb heaviness tend to be ipsilateral.
- Stroke is sometimes associated with pain, but this is usually contralateral to the limb symptoms.
- Spinal cord infarction secondary to vertebral artery dissection should be considered in individuals who present with neck pain, headache and ipsilateral motor and sensory symptoms.
Provenance: Not commissioned; externally peer reviewed.
- 1. Di Stefano V, Rispoli MG, Pellegrino N, et al. Diagnostic and therapeutic aspects of hemiplegic migraine. J Neurol Neurosurg Psychiatry 2020; 91: 764‐771.
- 2. Weidauer S, Nichtweiß M, Hattingen E, Berkefeld J. Spinal cord ischemia: aetiology, clinical syndromes and imaging features. Neuroradiology 2015; 57: 241‐257.
- 3. Kramer CL. Vascular disorders of the spinal cord. Continuum (Minneap Minn) 2018; 24: 407‐426.
- 4. Hsu JL, Cheng MY, Liao MF, et al. The etiologies and prognosis associated with spinal cord infarction. Ann Clin Transl Neurol 2019; 6: 1456‐1464.






Open access
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
No relevant disclosures.