Self‐harm and suicide by young people are major problems,1 and they are more frequent among people known to child protection services,2,3 especially those placed in out‐of‐home care.4 We used record linkage to quantify the cumulative incidence of self‐harm and suicidal ideation in a population sample of New South Wales children and adolescents aged 0–17 years with differing levels of child protection contact during 2003–21.
We analysed data for the 91 597 participants in wave 3 of the New South Wales Child Development Study5 (http://nsw‐cds.com.au). First incidents of self‐harm (International Classification of Diseases, tenth revision, Australian modification [ICD‐10‐AM] codes X60–X84, T14.91, Y87.0) or suicidal ideation (ICD‐10‐AM codes R45.81, R45.851) during 1 January 2000 – 31 March 2021 were identified in linked health records in the NSW and Australian Capital Territory emergency department, admitted patient, and mental health ambulatory data collections. Record linkage was conducted by the Centre for Health Record Linkage (http://www.cherel.org.au), with an estimated false positive linkage rate of 0.5%. Young people with records of both self‐harm and suicidal ideation were included in the self‐harm group.
Child protection contact was identified in the NSW Department of Communities and Justice ChildStory database6 (1 July 1998 – 31 July 2021). Each participant was assigned to one of four categories of child protection contact according to the highest level: out‐of‐home care, substantiated report of child abuse or neglect non‐substantiated/non‐threshold report of child abuse or neglect, and no child protection contact. The cumulative incidence of first incidents of self‐harm and suicidal ideation was calculated for each child protection level, based on the cumulative number of people at each year of age in the study sample (further details: Supporting Information). The NSW Population and Health Services, ACT Health, and Calvary Public Hospital human research ethics committees approved the study (HREC/18/CIPHS/49).
By age 17 years, incidents of self‐harm or suicidal ideation were recorded in medical records for 2233 study participants (2.4%) (Box 1); 866 incidents involved self‐harm, 1367 involved suicidal ideation (without self‐harm). By age 17, incidents had been recorded for 1505 girls (incidence, 3.4%) and 728 boys (incidence, 1.5%). Contact with child protection services was recorded for 1671 young people with records of self‐harm or suicidal ideation incidents (74.8%). The cumulative incidence of self‐harm or suicidal ideation by 17 years was 13.0% for young people with out‐of‐home care placements, 10.4% for those with substantiated reports, 4.6% for those with non‐substantiated/non‐threshold reports, and 0.9% for those who had not come into contact with child protection services (Box 2). A similar pattern pertained to separate analyses of self‐harm and suicidal ideation (Box 2), and to separate analyses by gender (Supporting Information, figure).
Not all incidents of self‐harm or suicidal ideation will have been captured in administrative health records.7 Our study is descriptive and no causal inferences should be drawn with regard to the impact of child protection service contact on the likelihood of self‐harm or suicidal ideation. We could not determine whether contact with child protection services preceded individual incidents, but 21 223 child protection contact episodes took place before the age of twelve years (79.3%), while 2139 first self‐harm and suicidal ideation incidents (95.7%) happened after age eleven years.
As almost three‐quarters of recorded self‐harm and suicidal ideation incidents requiring health care support involved young people who had experienced contact with child protection services, targeted prevention and intervention strategies are needed. Children and adolescents who have had contact with child protection services may benefit from screening for mental health problems, particularly for risks of self‐harm and suicidal ideation. The high incidence of self‐harm and suicidal ideation among young people who have contact with child protection services confirms that child maltreatment is an important public health concern.
Box 1 – Characteristics of the New South Wales Child Development Study (wave 3) participants
|
Characteristic |
Value |
||||||||||||||
|
|
|||||||||||||||
|
Number of people aged 0–17 years |
91 597 |
||||||||||||||
|
Gender (boys) |
47 381 (51.7%) |
||||||||||||||
|
Aboriginal or Torres Strait Islander |
7970 (8.7%) |
||||||||||||||
|
Child protection contact (highest level) |
|
||||||||||||||
|
None |
64 851 (70.8%) |
||||||||||||||
|
Non‐substantiated/non‐threshold report of abuse/neglect |
20 083 (21.9%) |
||||||||||||||
|
Substantiated report of abuse/neglect |
4325 (4.7%) |
||||||||||||||
|
Out‐of‐home care |
2338 (2.6%) |
||||||||||||||
|
Recorded incidents of self‐harm or suicidal ideation (by 17 years of age) |
2233 (2.4%) |
||||||||||||||
|
Any self‐harm |
866 (0.9%) |
||||||||||||||
|
Any suicidal ideation* |
1367 (1.5%) |
||||||||||||||
|
|
|||||||||||||||
|
* Excludes people with recorded incidents of self-harm. |
|||||||||||||||
Box 2 – Cumulative relative incidence of first incidents of self‐harm and suicidal ideation recorded in health care records of the 91 597 participants in the New South Wales Child Development Study (wave 3)
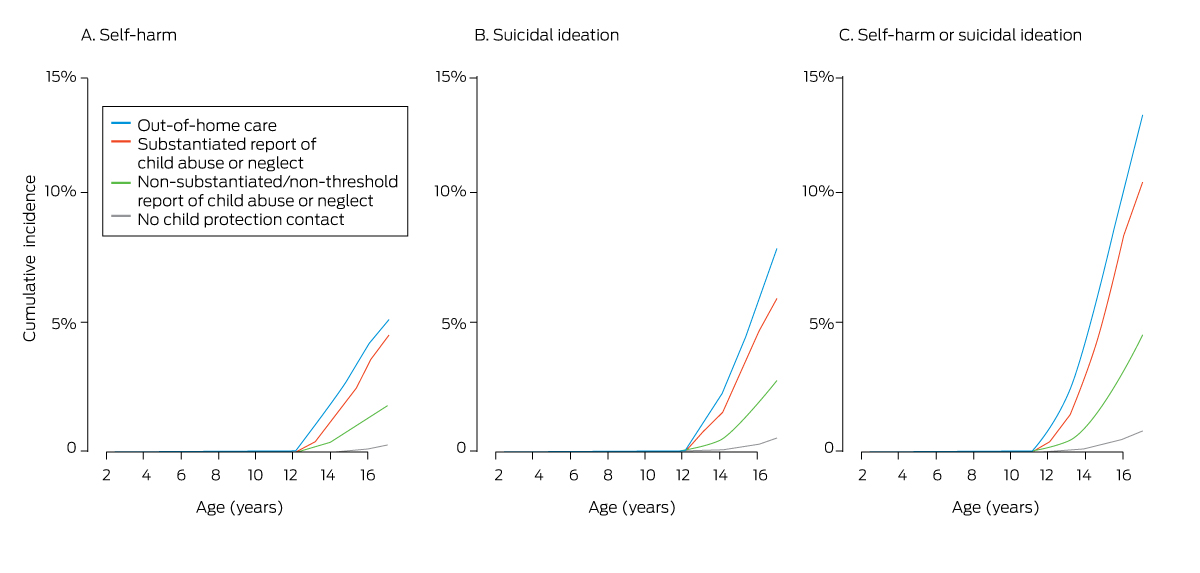
* The data on which these graphs are based are provided in the Supporting Information, table 1.
Received 12 December 2022, accepted 27 February 2023
- 1. Knipe D, Padmanathan P, Newton‐Howes G, et al. Suicide and self‐harm. Lancet 2022; 399: 1903‐1916.
- 2. Palmer L, Prindle J, Putnam‐Hornstein E. A population‐based case control study of suicide among youth reported for abuse and neglect. Child Abuse Negl 2021; 117: 105060.
- 3. Green MJ, Hindmarsh G, Kariuki M, et al. Mental disorders in children known to child protection services during early childhood. Med J of Aust 2020; 212: 22‐28. https://www.mja.com.au/journal/2020/212/1/mental‐disorders‐children‐known‐child‐protection‐services‐during‐early‐childhood
- 4. Evans R, White J, Turley R, et al. Comparison of suicidal ideation, suicide attempt and suicide in children and young people in care and non‐care populations: systematic review and meta‐analysis of prevalence. Children and Youth Services Review 2017; 82: 122‐129.
- 5. Green MJ, Harris F, Laurens KR, et al. Cohort profile: the New South Wales Child Development Study (NSW‐CDS). Wave 2 (child age 13 years). Int J Epidemiol 2018; 47: 1396‐1397k.
- 6. NSW Department of Communities and Justice. ChildStory. Updated 24 Sept 2019. https://www.facs.nsw.gov.au/families/childstory (viewed Feb 2023).
- 7. McMahon EM, Keeley H, Cannon M, et al. The iceberg of suicide and self‐harm in Irish adolescents: a population‐based study. Soc Psychiatry Psychiatr Epidemiol 2014; 49: 1929‐1935.






Open access
Open access publishing facilitated by University of New South Wales, as part of the Wiley ‐ University of New South Wales agreement via the Council of Australian University Librarians.
We analysed population data owned by the New South Wales Department of Communities and Justice, the NSW Ministry of Health, and ACT Health. The findings and views reported are those of the authors and should not be attributed to these departments or the ACT or NSW governments. The study was conducted at the University of New South Wales with financial support from a National Health and Medical Research Council Project Grant (APP1148055). The funding source played no role in the study design, data collection, analysis or interpretation, reporting or publication of this study.
No relevant disclosures.