Cardiac arrest treatment, to date, has been focused on high quality chest compressions and defibrillation, with pharmacological adjuncts (such as adrenaline) administered at the scene of cardiac arrest. For patients who do not promptly achieve return of spontaneous circulation (ROSC) with these measures and in whom cardiac arrest becomes refractory, brain and end‐organ dysfunction progresses and survival with good neurological outcomes becomes extremely uncommon.1,2 With increased availability of mechanical cardiopulmonary resuscitation (CPR), which enables continued mechanical chest compressions while transporting or treating the patient, new treatment pathways have emerged for cardiac arrest systems.3 Venoarterial extracorporeal membrane oxygenation (ECMO) is a circulatory support technology that provides oxygenation and perfusion of the coronary arteries, brain, and other vital organs while cardiac recovery or treatment is completed.4 The use of ECMO during cardiac arrest is termed “extracorporeal cardiopulmonary resuscitation” (ECPR).
ECPR can be offered for patients with both in‐hospital cardiac arrest (IHCA) and out‐of‐hospital cardiac arrest (OHCA). For patients with OHCA, ECPR is most commonly implemented after a patient is extricated from the scene and transported to an ECPR‐capable hospital — a process known as hospital‐based ECPR. Other models of ECPR delivery include i) pre‐hospital ECPR, where ECPR is established at the scene of the cardiac arrest and the patient is transported to a major ECMO centre, and ii) rendezvous ECPR, where a mobile ECPR team meets the ambulance team at the nearest available hospital, establishes ECPR support, and then retrieves the patient to an ECMO centre (Box 1, A–C).
The use of ECPR in cardiac arrest has increased at least eightfold for OHCA and tenfold for IHCA5 over the past 15 years in the United States. Data from the global Extracorporeal Life Support Organization (ELSO) Registry report an increase in annual ECPR cases from less than 100 in 2009 to more than 1500 in 2019.6 The number of hospitals offering ECPR for either IHCA or OHCA in Australia has increased from three to 11 in the past five years, with at least another five hospitals considering service provision. Despite this growth in ECPR, there remain significant questions as to its efficacy, generalisability, cost‐effectiveness, optimal delivery strategy, and its place in the chain of survival.7 Therefore, the aim of this narrative review is to summarise the potential need and evidence for ECPR, with a specific focus on its place in the Australian OHCA landscape, and discuss ongoing clinical and research questions to be considered in the development of ECPR in Australia.
Methods
We searched the MEDLINE database to identify relevant articles on OHCA and ECPR using the keywords “extracorporeal membrane oxygenation”, “ECMO”, “ECMO cardiopulmonary resuscitation”, “ECPR”, “out of hospital cardiac arrest” and “OHCA”, with the most recent search done in May 2023. We also identified relevant guidelines and reviews, including the guidelines from the American Heart Association, the European Society of Cardiology, the European Resuscitation Council, and the International Liaison Committee on Resuscitation and reviewed their reference lists. Direct communication with state‐based representatives was completed to ascertain past and present hospital numbers that offer ECPR. Discussions between the broader working group and international collaborators were used to summarise the key challenges for ECPR (Box 2) and activities required in ECPR (Box 3).
Cardiac arrest in Australia and potential ECPR patients
The exact number of patients who may benefit from ECPR for either OHCA or IHCA is yet to be elucidated. Over 25 000 OHCA events occur each year in Australia, of those where the emergency medical service attempts resuscitation, only 13% of patients survive to hospital discharge.8 When currently used ECPR inclusion criteria are applied to OHCA, for example, refractory cardiac arrest (ie, failure to achieve ROSC after 15 minutes of CPR or three defibrillation attempts), witnessed, shockable and with bystander CPR present, and age less than 70 years, the number of arrests that would be deemed to be ECPR‐eligible has been estimated internationally to between 4% and 11% of the total OHCA population.9,10,11 This estimate equates to approximately 1200–3500 OHCA patients each year in Australia who would be eligible for ECPR based on the current criteria. The exact number in Australia is not known and may actually be less.
IHCA numbers in Australia, and the number that may benefit from an ECPR program, are even more difficult to quantify. The overall frequency of IHCA is reported at about two per 1000 admissions, or about 3000 IHCA events per year, with significant variation in published frequency.12,13 The number of these events that would be appropriate for ECPR is only beginning to be elucidated, with recent work suggesting that one in six IHCA cases meet the current ECPR inclusion criteria.14
The characteristics of patients with OHCA and IHCA who require ECPR have generally been viewed as distinct. Refractory OHCA cases are predominantly driven by underlying coronary disease,15 while IHCA cases are more likely to be older patients with comorbid conditions and with higher rates of diabetes, heart disease, chronic obstructive pulmonary disease, and non‐shockable rhythms.16 However, a recent analysis of the Danish cardiac arrest registry reported no differences in demographic characteristics, comorbid conditions, and initial cardiac rhythm for patients with IHCA or OHCA.17 Systematic review data report a wide range of aetiologies of IHCA, with coronary disease representing 14% of cases,18 whereas coronary disease predominates in refractory OHCA, with rates of significant disease in 50% or more of cases.15
Rationale for ECPR in cardiac arrests
Optimal CPR and chest compression only supplies about 25–30% of the normal cardiac output,19 which is insufficient to prevent neurological and end‐organ damage, particularly in prolonged cardiac arrests. In venoarterial ECMO, blood is drained from the central venous system, passed through a gas exchange membrane, and returned at systemic pressure to the arterial system (Box 4). During ECPR, this is implemented during cardiac arrest, before ROSC. With the application of ECPR, near normal cerebral, coronary and end‐organ perfusion is possible, preventing and/or reducing organ dysfunction and increasing the likelihood of ROSC while awaiting cardiac recovery or definitive treatment (Box 4).
Summary of current evidence for ECPR
ECPR for OHCA
Currently, most evidence for ECPR for OHCA is derived from hospital‐based ECPR programs. This evidence, until recently, was predominantly from single centre observational data with heterogenous inclusion criteria, in differing health systems delivering variable survival outcomes. Observational studies and the ELSO Registry report survival rates of 25–50%,15,20,21,22,23,24 well above reported survival rates of comparable prolonged, conventionally treated cardiac arrests (< 5%), defined as more than 30 minutes resuscitation without ROSC9,25,26 (Box 5). In contrast, the largest registry study of OHCA in Paris,27 patients who received ECPR (n = 525) did not report a significant difference in survival compared with conventionally treated cardiac arrests (n = 12 666), 8.4% versus 8.6% respectively, including on multivariate or propensity matching.
More recently, three randomised control trials (Box 6) compared conventional advanced cardiac life support against expedited intra‐arrest transfer to hospital‐based ECPR. ARREST, a small single centre randomised clinical trial in Minnesota, United States, used a Bayesian trial design and was stopped early after meeting pre‐specified stop rules owing to efficacy of ECPR over conventional management (43% [n = 6/14] v 7% [n = 1/15]; risk difference, 36.2%; 95% confidence interval [CI], 3.7–59.2).28 This trial was completed in a well organised and mature cardiac arrest system where ECPR has previously been associated with documented survival rates of up to 50% in observational studies.15,21 The external generalisability of these findings is not clear.
A single centre study from Prague, Czech Republic, compared rapid intra‐arrest transport, in‐hospital ECPR, and invasive coronary angiography (n = 124) with standard advanced cardiac life support (n = 132). The trial was stopped at the recommendation of the data and safety monitoring board when pre‐specified criteria for futility of conventional treatment were met in a group of patients with resuscitation exceeding 30 minutes.29 On a post hoc as‐treated analysis of patients who did not achieve pre‐hospital ROSC, only one out of 81 patients (1.2%) treated with conventional advanced cardiac life support survived compared with 22/92 (23.9%) treated with ECPR (log‐rank; P < 0.001).30
Most recently, the INCEPTION trial (the Netherlands) randomly assigned selected patients with OHCA to receive either rapid transfer from the scene for hospital ECPR or standard advanced cardiac life support across ten cardiosurgical centres and 12 emergency medical services.31 No significant difference in favourable neurologic survival was seen at 30 days between the ECPR group (14 patients, 20%) and the conventional CPR group (10 patients [16%]; odds ratio, 1.4; 95% CI, 0.5–3.5; P = 0.52). Of note, in this study the low flow time, defined as the time from OHCA to ECMO flow, which is a known important prognostic indicator (Box 5), was prolonged (median, 74 minutes; interquartile range [IQR], 63–87 minutes), and many sites had minimal ECPR experience before the start of the trial. Moreover, survival in patients who actually received ECPR was five out of 52 (9.6%), which is significantly lower than the other studies and registries: ARREST trial 46%, PRAGUE study 31.5%, current ELSO Registry data 29%.
Currently published Australian data22,23,32 as well as contemporaneous data from the national ECMO Registry33 report that the survival to hospital discharge is between 20% and 45%. The available data suggest potential benefit of ECPR for carefully selected patients with refractory OHCA over conventional CPR in well developed cardiac arrest systems, where the arrest to ECMO flow time is minimised.
Alternative models of delivery of ECPR for OHCA
Favourable outcomes with ECPR in refractory cardiac arrest reduce as low flow time (the time from cardiac arrest to initiation of ECMO) increases (Box 5) and it is recommended that ECMO support commences within one hour from cardiac arrest.34 The obligate response time of emergency medical services, initial treatment, extrication and transport to the nearest ECPR hospital, as well as the time needed to initiate ECMO, make achieving this time point very challenging and limits the geographical area and population that can be covered by hospital‐based ECPR. These challenges are demonstrable; data from Victoria, on 223 ECPR‐eligible patients, reported a median time to hospital of 63.9 minutes (IQR, 54.3–82.0 minutes) to an ECPR centre and 67.8 minutes (IQR, 57.0–82.2 minutes) to non‐ECPR centres.35 An analysis of OHCA events in Brisbane, Queensland, identified that only 11% of ECPR‐eligible patients were able to reach the ECPR‐capable hospital in less than one hour,36 and only 1.68% of patients with OHCA in the US were eligible for ECPR based on transfer to an ECMO‐ready centre model.37 A further challenge with this approach is that transportation of patients while CPR is ongoing may reduce the quality of CPR and possibly survival.38
In an effort to reduce low flow time, alternative ECPR delivery strategies such as pre‐hospital ECPR and rendezvous ECPR are being used and trialled. These services have the added potential benefit of having single or smaller number of staff, thereby reducing training requirements and rostering complexities while also ensuring staff are well exposed to a relative infrequently performed procedure. Existing evidence for the efficacy of pre‐hospital ECPR is limited. A recent systematic review identified only four studies with a total of 222 patients receiving pre‐hospital ECPR, with an overall survival rate at discharge of 23.4%.39 The largest observational study of pre‐hospital ECPR has been undertaken in Paris, in which 114 patients in refractory arrest who had ECMO commencing after 30 minutes of CPR were compared with 42 patients who were placed on ECMO commencing after 20 minutes of CPR at scene.40 The probability of survival to intensive care unit discharge with good neurological function was significantly higher in patients placed on ECMO earlier (29% v 8%; P < 0.001), and when stringent patient selection was used with an aggressive strategy, the probability of survival in patients with a shorter CPR duration increased to 38%.40
In addition to efficacy data, the optimal make‐up and location of the pre‐hospital team, is yet to be elucidated. Hospital‐based teams who leave their home hospital to attend an OHCA event are being trialled (Melbourne; ACTRN12619000303145), as are pre‐hospital emergency clinicians trained in the provision of ECPR cannulation and support (France,1 the Netherlands [ClinicalTrials.gov Identifier NCT04620070] and London [ClinicalTrials.gov Identifier NCT03700125]). The ability to scale and sustain either option and the cost of this are yet to be assessed.
Rendezvous ECPR, where the pre‐hospital ECPR team “rendezvous” with the emergency medical services at the nearest hospital and implements ECMO at that hospital before retrieving the patient back to a large ECMO centre,41 is thus far limited in Minnesota, with promising favourable survival rates of 43% (CI, 31–56%) at three months. The operational challenges and processes of planning and enabling ECPR at hospitals that have limited experience to ECMO across large metropolitan areas are complex.
ECPR for in‐hospital cardiac arrests
The evidence of ECPR in IHCA is very limited and no randomised control trials exist. Patients with IHCA treated with ECPR have documented survival rates between 20% and 40%.42,43,44,45 Propensity matched data43 reported significantly better survival to hospital discharge of ECPR over conventional CPR, a finding confirmed on a 2013 analysis44 and on a subsequent meta‐analysis.45 Recently, adult patients treated with ECPR for IHCA were identified from the American Heart Association Get With the Guidelines – Resuscitation Registry, where there was a 28% survival among 1075 IHCA ECPR cases from 219 centres.46 The current Australian and New Zealand Bi‐national registry IHCA ECPR survival rate to hospital discharge is 67%.33
Of note, for both IHCA and OHCA, most studies have reported a relatively binary outcome, with either early death or having a relatively good neurological outcome (cerebral performance categories 1–2).47 Concerns over ECPR producing increased survival but with profound neurological deficit, thus far, have not been borne out in the literature.
ECPR cost effectiveness
ECPR is resource‐intensive, with a cost per hospital‐based ECPR patient of about $75 000.48 Although expensive, cost‐effectiveness for both IHCA and OHCA has been confirmed within Australia and internationally,48,49,50 with ECPR adding four quality‐adjusted life‐years per patient at $18 829 over 15 years and incremental cost‐effectiveness ratios below common accepted willingness‐to‐pay thresholds.49,51 However, all these studies were completed in well established systems and do not assess the cost effectiveness of establishing new ECPR programs, the system level impacts of ECPR, nor pre‐hospital ECPR. The workforce implications, sustainability and scalability of new models of care and the opportunity cost of resources placed into ECPR versus other forms of cardiac arrest interventions have not been assessed, nor the impact of ECPR programs on hospital bed stays and other planned interventions or procedures, given substantial resources are required for each patient.
International guidelines on ECPR
Given the predominance of heterogenous observational and randomised studies that are often single centre with significant methodological flaws, international guidelines have reported insufficient evidence to recommend the routine use of ECPR for patients with cardiac arrest,52 with ECPR considered a rescue therapy for selected patients when conventional CPR is failing (weak recommendation, very low certainty evidence).53,54 A recent updated systematic review from the International Liaison Committee on Resuscitation55 including randomised controlled trial data suggests a benefit of ECPR, but the certainty of evidence remains low, with a lack of clarity as to which patients may benefit from ECPR.
ECPR in Australia
ECPR in Australia, thus far, has been limited to a small number of large metropolitan hospitals and is hospital‐based. Studies report a survival to hospital discharge with favourable neurological outcome between 25% and 45% both for IHCA and OHCA.22,23,24 Existing services are limited to Sydney (four hospitals all OHCA and IHCA), Melbourne (four IHCA, two OHCA), Geelong (one), Brisbane (three hospitals for IHCA, one OHCA), the Gold Coast (IHCA and OHCA), Adelaide (two hospitals IHCA and OHCA) and Perth (one hospital IHCA and OHCA). Several additional hospitals are considering ECPR for OHCA and IHCA or will complete ECPR on an ad hoc basis if resources are available. Of note, only two hospitals in Australia are able to resource and offer an ECPR service 24 hours a day 7 days, with remaining ECPR‐capable hospitals limited to when appropriate resources are available (around office hours). ECPR‐capable hospitals have traditionally been established ECMO referral hospitals; however, this has expanded outside of these hospitals to include hospitals that initiate ECPR or ECMO in a timely manner and then transfer the patient to larger ECMO referral centres as part of state‐based referral networks. Pre‐hospital feasibility trials are underway in Melbourne (CHEER 3 Trial; ACTRN12619000303145) and planned in Sydney.
The access of the current ECPR delivery system has been assessed using geographic information system and transport accessibility principles in Sydney.56 This modelling reported that the current hospital‐based ECPR system for OHCA is the most inefficient in terms of patient access, with limited incremental value in patient access with the addition of more ECPR‐capable hospitals.56 Alternative delivery methods, rendezvous and pre‐hospital ECPR were shown to significantly increase patient access (Box 7), even with the most conservative of models, with findings consistent with international modelling research.58,59
ECPR unanswered questions and evolution in Australia
There are several unanswered questions with regards to cardiac arrest systems that include ECPR, highlighted by a recent clinician survey60 and from OHCA survivors and consumers (Box 2), including equity of access, which remains a significant challenge. About 50% of IHCA61 and over 60% of OHCA events occur after hours or on the weekend,62 when most existing ECPR hospitals do not have the required resources to cannulate and establish ECPR emergently. For OHCA, when this is combined with the very limited catchment area where OHCA cases are able to get to an ECPR‐capable hospital within 45 minutes to allow ECMO support to commence within less than one hour, the number of patients with OHCA who could benefit from the current model of service is limited to a very small number, predominantly during office hours, at or very near a few limited hospitals, which is a substantial inequity of service. The same issue exists for IHCA. Owing to the resources and skill sets required to initiate and maintain ECMO support, it is very unlikely ECPR will be offered at a majority or all hospitals, let alone regional and rural hospitals and communities. Only patients who have an IHCA in or around office hours at select hospitals have access to a potentially life‐saving therapy. To improve equity of access, alternate modes of delivery, training and systems are required, but challenges remain substantial, otherwise the inequity seen between geographical and social groups are likely to widen.
Patient selection remains a significant challenge to ensure appropriate sensitivity and specificity to ensure the suitable application of resources. Traditional selection criteria for ECPR have been based on OHCA data. It is possible that different patient selection criteria of IHCA are appropriate, given the likely different patient profile, increased rates of witnessed arrests, bystander CPR and shorter arrest to ECMO flow times seen in IHCA.63
Future developments for ECPR in Australia
ECPR has undergone several different phases in Australia. The first phase included observational studies from the initial experience of several large ECPR centres in metropolitan areas (phase 1, 2010–2020). Phase 2, from 2018 to 2022, has seen the growth in the number of ECPR sites for IHCA and OHCA services, along with improved reporting and data sharing through the national ECMO Registry. Phase 3 (from 2019 to 2023) is seeing development of pre‐hospital ECPR feasibility studies, with two pilot feasibility studies currently underway. Phase 4 (from 2023 onwards) will likely see the expansion in the number of sites doing hospital‐based ECPR for ICHA and OHCA and may see expansion of pre‐hospital ECPR depending on current pilot work. To ensure appropriate patient selection and service expansion, much needed collaborative research will be required to inform the role, evidence base and cost‐effectiveness of ECPR in Australia.
Summary of recommendations and future
In response to the many challenges in delivering ECPR outlined above, we propose a proactive systematic approach to development of ECPR evidence systems and processes, moving away from a more reactive approach. This includes better integration of pre‐hospital care into hospital care and the development of a coordinated approach within states and to maximise data efficacy. We propose the key activities described in Box 3 to ensure, where appropriate, the evidence‐based application of ECPR in the most efficacious manner and minimising wasted health care expenditure. The importance of additional randomised controlled trial data6 and health economic data has been made a priority6,53 by international groups and guidelines bodies.
Conclusions
Patients with refractory cardiac arrest have an unmet need, and a cardiac arrest system with ECPR integrated is a promising intervention for these patients. Important questions remain pertaining to the best delivery and management of ECPR, cost‐effectiveness, and integration into the broader OHCA and IHCA survival chain. A coordinated national approach to these challenging and relatively infrequent events is required.
Box 1 – Different extracorporeal cardiopulmonary resuscitation (ECPR) delivery strategies for out‐of‐hospital cardiac arrest (OHCA)*
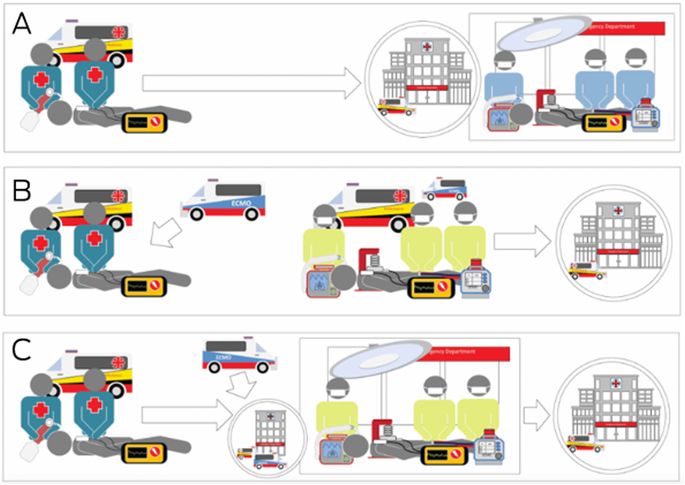
* (A) Hospital‐based ECPR: the patient is transported from scene of the OHCA event to the nearest ECPR hospital. (B) Pre‐hospital ECPR: a mobile ECPR team is dispatched and institutes ECPR support at the site of OHCA. (C) Rendezvous ECPR: a mobile team meets the patient and paramedics at any nearest hospital, implements ECPR, and transfers the patient back to an extracorporeal membrane oxygenation centre.
Box 2 – Outstanding questions and challenges pertaining to extracorporeal cardiopulmonary resuscitation (ECPR) in Australia
Technical questions | System level questions | ||||||||||||||
|
| ||||||||||||||
ECMO = extracorporeal membrane oxygenation; PCO2 = partial pressure of carbon dioxide; PO2 = partial pressure of oxygen. | |||||||||||||||
Box 3 – Key extracorporeal cardiopulmonary resuscitation (ECPR) activities required in Australia
- Detailed needs analysis of potential ECPR patients throughout Australia including in‐hospital cardiac arrest
- Phase 3 randomised controlled trial including hospital‐based ECPR, pre‐hospital ECPR, and advanced cardiac life support
- Detailed health economic assessment ideally based on randomised controlled trial data, that includes assessment of scalability and intervention versus other arrest interventions
- Integration of ECPR strategies into the survival chain pathway based on the data above
Box 4 – Venoarterial extracorporeal membrane oxygenation (ECMO) using a peripheral configuration with femoral vessel cannulation*
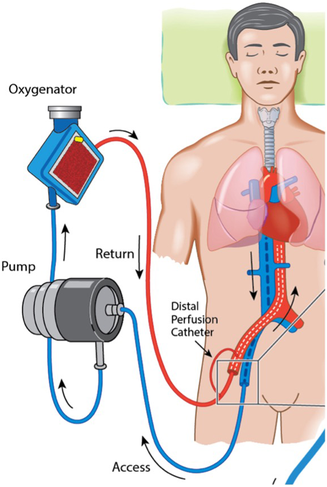
* Venous blood (blue) is drained via a cannula with the tip positioned near the inferior vena cava to the right atrial junction, and passes through the blood pump and extracorporeal membrane, where uptake of oxygen and removal of carbon dioxide occurs. The now oxygenated blood (red) is returned via a “return” cannula positioned in the common iliac artery or descending aorta. Reproduced with permission from Dennis et al.4
Box 5 – Relation between low flow duration in minutes and hospital survival in percentage in adult patients treated with extracorporeal cardiopulmonary resuscitation (red diagonal line), conventional cardiopulmonary resuscitation (CCPR) due to shockable initial cardiac rhythms (blue parabola), and CCPR due to non‐shockable initial cardiac rhythms (yellow dots, no line)
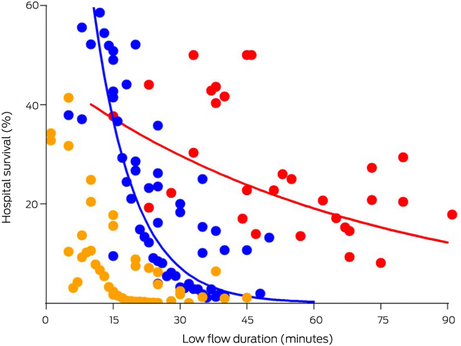
Adapted with permission from Mandigers et al.26
Box 6 – Summary of available extracorporeal cardiopulmonary resuscitation (ECPR) randomised control trials
Study | ECPR patients in study | Median age (years) | Initial rhythm on inclusion | Median low flow time (min) | Survival in ECPR arm | Survival in control arm | Number of ECPR centres | ||||||||
ARREST (2020)28 | 15 | 59 | VT/VF | 59 | 43% | 7% | 1 | ||||||||
PRAGUE OHCA (2022)29 | 124 | 58 | VT/VF/PEA/asystole | 61 | 31% | 22.0% | 1 | ||||||||
INCEPTION (2023)31 | 52 | 54 | VT/VF | 74 | 20% | 16% | 10 | ||||||||
PEA = pulseless electrical activity; VF = ventricular fibrillation; VT = ventricular tachycardia. | |||||||||||||||
Box 7 – (A) Map depicting the current extracorporeal cardiopulmonary resuscitation (ECPR)‐capable hospitals in Sydney, Australia. The small blue islands represent where patients would have a survival benefit over conventional resuscitation assuming a time limit of one hour to implementation of ECPR support. (B) With the application of a single pre‐hospital team in addition to the existing five hospitals, pre‐hospital ECPR adds significant amount of coverage (green) and potential survival benefit57
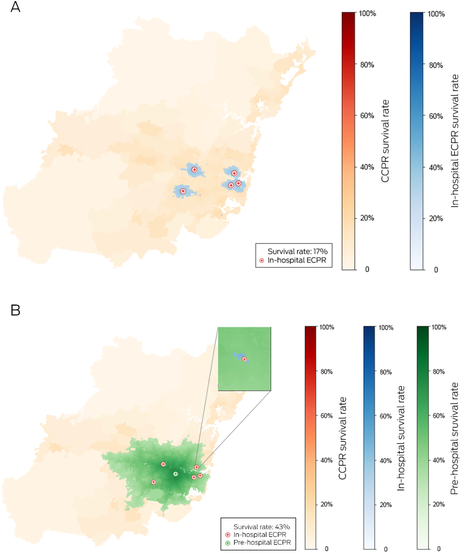
Adapted and used with permission from Song et al.56
Provenance: Not commissioned; externally peer reviewed.
- Mark Dennis1,2
- Kiran Shekar3,4
- Aidan JC Burrell5,6
- For the National ECPR Working Group
- 1 Royal Prince Alfred Hospital, Sydney, NSW
- 2 University of Sydney, Sydney, NSW
- 3 Prince Charles Hospital, Brisbane, QLD
- 4 Critical Care Research Group and Centre of Research Excellence for Advanced Cardio‐respiratory Therapies Improving Organ Support, University of Queensland, Brisbane, QLD
- 5 Alfred Health, Melbourne, VIC
- 6 Monash University, Melbourne, VIC
Open access:
Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Mark Dennis is supported by a Post‐Doctoral Scholarship (Ref: 105849) from the National Heart Foundation of Australia. The National Heart Foundation had no role in the study design, collection, analysis or interpretation of the data nor in writing of the data and submission of the article.
We acknowledge the Australian ECPR Working Group contributors: Danielle Austin (Liverpool Hospital, Sydney), David Anderson (Ambulance Victoria and The Alfred Hospital, Melbourne), Stephen Bernard (The Alfred Hospital and Monash University, Melbourne), Emma Bosley (Queensland Ambulance Service and Queensland University of Technology, Brisbane), Brian Burns (New South Wales Ambulance and University of Sydney, Sydney), Hergen Buscher (St Vincent's Hospital Sydney and University of New South Wales, Sydney), Gayle Christie (St John Western Australia and Curtin University, Perth), Luke Collett (Royal Adelaide Hospital, Adelaide), Andrew Coggins (Westmead Hospital and University of Sydney, Sydney), Tan Doan (Queensland Ambulance Service, Queensland Government Department of Health, Brisbane; Royal Melbourne Hospital, University of Melbourne, Melbourne; Australian Institute of Tropical Health and Medicine, James Cook University, Townsville), Jayesh Dhanani (University of Queensland Centre of Clinical Research and Royal Brisbane and Women's Hospital, Brisbane), Judith Finn (Monash University, Melbourne; Curtin University and St John Western Australia, Perth), Caleb Fisher (Austin Health and University of Melbourne Melbourne), Ian Ferguson (NSW Ambulance and Liverpool Hospital, Sydney), Paul Forrest (Royal Prince Alfred Hospital and University of Sydney, Sydney), Denzil Gill (Prince Charles Hospital, Brisbane), Emily Granger (St Vincent's Hospital, Sydney), Lisa Higgins (Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne), Carol Hodgson (Alfred Hospital and Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne), Daryl Jones (Austin Health, Monash University and University of Melbourne, Melbourne), Natalie Kruit (NSW Ambulance, Westmead Hospital, and University of Sydney, Sydney), Andre La Gerche (Baker Heart and Diabetes Institute, National Centre for Sports Cardiology, and St Vincent's Hospital Melbourne, Melbourne), Silvana Marasco (Alfred Hospital and Monash University, Melbourne), Kevin Maruno (St Vincent's Hospital, Sydney), Peter McCanny (Liverpool Hospital, Sydney), Emily Moylan (University of Sydney, Sydney), Vinod Nanjayya (Alfred Hospital, Melbourne), Priya Nair (St Vincent's Hospital and University of New South Wales, Sydney), Alistair Nichol (Alfred Hospital, and Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne), Matthew Oliver (Royal Prince Alfred Hospital and Faculty of Medicine, University of Sydney, Sydney), Vin Pellegrino (Alfred Hospital and Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne), Brian Plunkett (Royal Prince Alfred Hospital and University of Sydney, Sydney), Mahesh Ramanan (Prince Charles Hospital and University of Queensland, Brisbane), Sacha Richardson (Alfred Hospital, Melbourne), Timothy J Southwood (Royal Prince Alfred Hospital and University of Sydney, Sydney), Kiran Shekar (Prince Charles Hospital and University of Queensland, Brisbane), Mark Sackley (consumer representative and cardiac arrest survivor), Christopher Semsarian (Agnes Ginges Centre for Molecular Cardiology, Centenary Institute and University of Sydney, Sydney), Richard Totaro (Royal Prince Alfred Hospital and University of Sydney, Sydney), James Winearls (Gold Coast University Hospital, Gold Coast).
No relevant disclosures.
- 1. Goto Y, Funada A, Goto Y. Relationship between the duration of cardiopulmonary resuscitation and favorable neurological outcomes after out‐of‐hospital cardiac arrest: a prospective, nationwide, population‐based cohort study. J Am Heart Assoc 2016; 5: e002819.
- 2. Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in‐hospital cardiac arrest: an observational study. Lancet 2012; 380: 1473‐1481.
- 3. Poole K, Couper K, Smyth MA, et al. Mechanical CPR: Who? When? How? Crit Care 2018; 22: 140.
- 4. Dennis M, Lal S, Forrest P, et al. In‐depth extracorporeal cardiopulmonary resuscitation in adult out‐of‐hospital cardiac arrest. J Am Heart Assoc 2020; 9: e016521.
- 5. Hadaya J, Dobaria V, Aguayo E, et al. National trends in utilization and outcomes of extracorporeal support for in‐ and out‐of‐hospital cardiac arrest. Resuscitation 2020; 151: 181‐188.
- 6. Abrams D, MacLaren G, Lorusso R, et al. Extracorporeal cardiopulmonary resuscitation in adults: evidence and implications. Intensive Care Med 2022; 48: 1‐15.
- 7. MacLaren G, Masoumi A, Brodie D. ECPR for out‐of‐hospital cardiac arrest: more evidence is needed. Crit Care 2020; 24: 7.
- 8. Bray J, Howell S, Ball S, et al. The epidemiology of out‐of‐hospital cardiac arrest in Australia and New Zealand: A binational report from the Australasian Resuscitation Outcomes Consortium (Aus‐ROC). Resuscitation 2022; 172: 74‐83.
- 9. Reynolds JC, Grunau BE, Elmer J, et al. Prevalence, natural history, and time‐dependent outcomes of a multi‐center North American cohort of out‐of‐hospital cardiac arrest extracorporeal CPR candidates. Resuscitation 2017; 117: 24‐31.
- 10. Grunau B, Scheuermeyer FX, Stub D, et al. Potential candidates for a structured Canadian ECPR program for out‐of‐hospital cardiac arrest. CJEM 2016; 18: 453‐460.
- 11. Reynolds JC, Frisch A, Rittenberger JC, Callaway CW. Duration of resuscitation efforts and functional outcome after out‐of‐hospital cardiac arrest: when should we change to novel therapies? Circulation 2013; 128: 2488‐2494.
- 12. Fennessy G, Hilton A, Radford S, et al. The epidemiology of in‐hospital cardiac arrests in Australia and New Zealand. Intern Med J 2016; 46: 1172‐1181.
- 13. Jones D PG, Eastwood G, Hodgson C. Estimate of annual in‐hospital cardiac arrests in Australia. Crit Care Resus 2021; 23: 427.
- 14. Pound G, Eastwood GM, Jones D, Hodgson CL; ANZ‐CODE Investigators. Potential role for extracorporeal membrane oxygenation cardiopulmonary resuscitation (E‐CPR) during in‐hospital cardiac arrest in Australia: a nested cohort study. Crit Care Resus 2023; 2: 90‐96.
- 15. Yannopoulos D, Bartos JA, Raveendran G, et al. Coronary artery disease in patients with out‐of‐hospital refractory ventricular fibrillation cardiac arrest. J Am Coll Cardiol 2017; 70: 1109‐1117.
- 16. Andersson A, Arctaedius I, Cronberg T, et al. In‐hospital versus out‐of‐hospital cardiac arrest: Characteristics and outcomes in patients admitted to intensive care after return of spontaneous circulation. Resuscitation 2022; 176: 1‐8.
- 17. Høybye M, Stankovic N, Holmberg M, et al. In‐hospital vs. out‐of‐hospital cardiac arrest: patient characteristics and survival. Resuscitation 2021; 158: 157‐165.
- 18. Allencherril J, Lee PYK, Khan K, et al. Etiologies of In‐hospital cardiac arrest: A systematic review and meta‐analysis. Resuscitation 2022; 175: 88‐95.
- 19. Lurie KG, Nemergut EC, Yannopoulos D, Sweeney M. The physiology of cardiopulmonary resuscitation. Anesth Analg 2016; 122: 767‐783.
- 20. Downing J, Al Falasi R, Cardona S, et al. How effective is extracorporeal cardiopulmonary resuscitation (ECPR) for out‐of‐hospital cardiac arrest? A systematic review and meta‐analysis. Am J Emerg Med 2022; 51: 127‐138.
- 21. Yannopoulos D, Bartos JA, Martin C, et al. Minnesota Resuscitation Consortium's advanced perfusion and reperfusion cardiac life support strategy for out‐of‐hospital refractory ventricular fibrillation. J Am Heart Assoc 2016; 5: e003732.
- 22. Dennis M, Buscher H, Gattas D, et al. Prospective observational study of mechanical cardiopulmonary resuscitation, extracorporeal membrane oxygenation and early reperfusion for refractory cardiac arrest in Sydney: the 2CHEER study. Crit Care Resusc 2020; 22: 26‐34.
- 23. Dennis M, McCanny P, D'Souza M, et al. Extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest: a multicentre experience. Int J Cardiol 2017; 231: 131‐136.
- 24. Stub D, Bernard S, Pellegrino V, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation 2015; 86: 88‐94.
- 25. Goto Y, Funada A, Goto Y. Duration of prehospital cardiopulmonary resuscitation and favorable neurological outcomes for pediatric out‐of‐hospital cardiac arrests: a nationwide, population‐based cohort study. Circulation 2016; 134: 2046‐2059.
- 26. Mandigers L, Boersma E, den Uil CA, et al. Systematic review and meta‐analysis comparing low‐flow duration of extracorporeal and conventional cardiopulmonary resuscitation. Interact Cardiovasc Thorac Surg 2022; 35: ivac219.
- 27. Bougouin W, Dumas F, Lamhaut L, et al. Extracorporeal cardiopulmonary resuscitation in out‐of‐hospital cardiac arrest: a registry study. Eur Heart J 2019; 41: 1961‐1971.
- 28. Yannopoulos D, Bartos J, Raveendran G, et al. Advanced reperfusion strategies for patients with out‐of‐hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open‐label, randomised controlled trial. Lancet 2020; 396: 1807‐1816.
- 29. Belohlavek J, Smalcova J, Rob D, et al. Effect of intra‐arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out‐of‐hospital cardiac arrest: a randomized clinical trial. JAMA 2022; 327: 737‐747.
- 30. Belohlavek J, Yannopoulos D, Smalcova J, et al. Intraarrest transport, extracorporeal cardiopulmonary resuscitation, and early invasive management in refractory out‐of‐hospital cardiac arrest: an individual patient data pooled analysis of two randomised trials. EClinicalMedicine 2023; 59: 101988.
- 31. Suverein MM, Delnoij TSR, Lorusso R, et al. Early extracorporeal CPR for refractory out‐of‐hospital cardiac arrest. N Engl J Med 2023; 388: 299‐309.
- 32. Stub D, Bernard S, Pellegrino V, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation 2015; 86: 88‐94.
- 33. Monash University. EXCEL — the Australian and New Zealand Extracorporeal Membrane Oxygenation Registry [website]. Melbourne: Monash University, 2023. https://www.monash.edu/medicine/sphpm/registries/excel (viewed June 2023).
- 34. Richardson ASC, Tonna JE, Nanjayya V, et al. Extracorporeal cardiopulmonary resuscitation in adults. Interim guideline consensus statement from the Extracorporeal Life Support Organization. ASAIO J 2021; 67: 221‐228.
- 35. Bernard SA, Hopkins SJ, Ball JC, et al. Outcomes of patients with refractory out‐of‐hospital cardiac arrest transported to an ECMO centre compared with transport to non‐ECMO centres. Crit Care Resusc 2022; 24: 7‐13.
- 36. Ramanan M, Gill D, Doan T, et al. Assessing need for extracorporeal cardiopulmonary resuscitation for out‐of‐hospital cardiac arrest using Power BI for data visualisation. Emerg Med Australas 2021; 33: 685‐690.
- 37. Gottula AL, Shaw CR, Gorder KL, et al. Eligibility of out‐of‐hospital cardiac arrest patients for extracorporeal cardiopulmonary resuscitation in the United States: a geographic information system model. Resuscitation 2022; 180: 111‐120.
- 38. Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation 2013; 128: 417‐435.
- 39. Kruit N, Rattan N, Tian D, et al. Prehospital extracorporeal cardiopulmonary resuscitation for out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. J Cardiothorac Vasc Anesth 2023; 37: 748‐754.
- 40. Lamhaut L, Hutin A, Puymirat E, et al. A pre‐hospital extracorporeal cardio pulmonary resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: an observational study and propensity analysis. Resuscitation 2017; 117: 109‐117.
- 41. Bartos JA, Frascone RJ, Conterato M, et al. The Minnesota mobile extracorporeal cardiopulmonary resuscitation consortium for treatment of out‐of‐hospital refractory ventricular fibrillation: program description, performance, and outcomes. EClinicalMedicine 2020; 29‐30: 100632.
- 42. D'Arrigo S, Cacciola S, Dennis M, et al. Predictors of favourable outcome after in‐hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta‐analysis. Resuscitation 2017; 121: 62‐70.
- 43. Chen YS, Lin JW, Yu HY, et al. Cardiopulmonary resuscitation with assisted extracorporeal life‐support versus conventional cardiopulmonary resuscitation in adults with in‐hospital cardiac arrest: an observational study and propensity analysis. Lancet 2008; 372: 554‐561.
- 44. Shin TG, Jo IJ, Sim MS, et al. Two‐year survival and neurological outcome of in‐hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol 2013; 168: 3424‐3430.
- 45. Ouweneel DM, Schotborgh JV, Limpens J, et al. Extracorporeal life support during cardiac arrest and cardiogenic shock: a systematic review and meta‐analysis. Intensive Care Med 2016; 42: 1922‐1934.
- 46. Tonna JE, Selzman CH, Girotra S, et al; American Heart Association Get With the Guidelines – Resuscitation Investigators. Resuscitation Using ECPR During In‐Hospital Cardiac Arrest (RESCUE‐IHCA) mortality prediction score and external validation. JACC Cardiovasc Interv 2022; 15: 237‐247.
- 47. Edgren E, Hedstrand U, Kelsey S, et al. Assessment of neurological prognosis in comatose survivors of cardiac arrest. BRCT I Study Group. Lancet 1994; 343: 1055‐1059.
- 48. Dennis M, Zmudzki F, Burns B, et al. Cost effectiveness and quality of life analysis of extracorporeal cardiopulmonary resuscitation (ECPR) for refractory cardiac arrest. Resuscitation 2019; 139: 49‐56.
- 49. Doan TN, Rashford S, Pincus J, Bosley E. Cost‐effectiveness of extracorporeal cardiopulmonary resuscitation for refractory out‐of‐hospital cardiac arrest: a modelling study. Resusc Plus 2022; 12: 100309.
- 50. Addison D, Cheng E, Forrest P, et al. Cost‐effectiveness of extracorporeal cardiopulmonary resuscitation for adult out‐of‐hospital cardiac arrest: a systematic review. Resuscitation 2022; 178: 19‐25.
- 51. Gravesteijn BY, Schluep M, Voormolen DC, et al. Cost‐effectiveness of extracorporeal cardiopulmonary resuscitation after in‐hospital cardiac arrest: a Markov decision model. Resuscitation 2019; 143: 150‐157.
- 52. Panchal AR, Bartos JA, Cabanas JG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020; 142 (Suppl): S366‐S468.
- 53. Berg KM, Soar J, Andersen LW, et al. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2020; 142 (Suppl): S92‐S139.
- 54. Soar J, Bottiger BW, Carli P, et al. European Resuscitation Council guidelines 2021: adult advanced life support. Resuscitation 2021; 161: 115‐151.
- 55. Holmberg MJ, Granfeldt A, Guerguerian AM, et al. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: an updated systematic review. Resuscitation 2022; 182: 109665.
- 56. Song C, Dennis M, Burns B, et al. Improving access to extracorporeal membrane oxygenation for out of hospital cardiac arrest: pre‐hospital ECPR and alternate delivery strategies. Scand J Trauma Resusc Emerg Med 2022; 30: 77.
- 57. Pozzi M, Cesareo E, Pinero D, et al. Pre‐hospital extracorporeal cardiopulmonary resuscitation for refractory out‐of‐hospital cardiac arrest: preliminary results of a multidisciplinary approach. Resuscitation 2022; 176: 19‐20.
- 58. Spigner M, Braude D, Pruett K, et al. The use of predictive modeling to compare prehospital eCPR strategies. Prehosp Emerg Care 2022; 27: 184‐191.
- 59. Vos IA, Deuring E, Kwant M, et al. What is the potential benefit of pre‐hospital extracorporeal cardiopulmonary resuscitation for patients with an out‐of‐hospital cardiac arrest? A predictive modelling study. Resuscitation 2023; https://doi.org/10.1016/j.resuscitation.2023.109825 [Epub ahead of print].
- 60. Dennis M, Southwood TJ, Oliver M, et al. Extracorporeal membrane oxygenation and extracorporeal membrane oxygenation cardiopulmonary resuscitation (ECPR) research priorities in Australia: a clinician survey. Aust Crit Care 2023; 36: 828‐831.
- 61. Ofoma UR, Basnet S, Berger A, et al; American Heart Association Get With the Guidelines – Resuscitation Investigators. Trends in survival after in‐hospital cardiac arrest during nights and weekends. J Am Coll Cardiol 2018; 71: 402‐411.
- 62. Bagai A, McNally BF, Al‐Khatib SM, et al. Temporal differences in out‐of‐hospital cardiac arrest incidence and survival. Circulation 2013; 128: 2595‐2602.
- 63. Wengenmayer T, Rombach S, Ramshorn F, et al. Influence of low‐flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care 2017; 21: 157.






Summary