Australia has effectively instituted a vaccination mandate while maintaining critical workforce capacity in aged care
Older people living in residential care in Australia and many other countries have been particularly affected by coronavirus disease 2019 (COVID‐19), because older people are at increased risk of severe illness and death. Vaccination of both residents and staff in residential care settings is a crucial measure to protect older members of the community.
On 28 June 2021, Australia's National Cabinet endorsed the introduction of mandatory COVID‐19 vaccinations for workers in residential aged care facilities (RACFs), with all staff required to receive a first dose by 17 September 2021.1 At the time, debate around mandatory vaccination for health and social care workers was evolving in many countries, with common concerns about practical, ethical, legal and human rights implications.2,3 Few countries had moved to implement vaccine mandates, with little COVID‐19 specific evidence or experience to draw on, although many had previously implemented mandatory staff vaccination initiatives for other vaccine‐preventable diseases in residential aged care settings, especially seasonal influenza.4
In Australia, views on vaccine mandates were mixed, with concerns regarding vaccine supply and logistics as well as the potential impact of such demands on goodwill, compliance and workforce availability. While Australian employers have a responsibility to eliminate or minimise the risk of exposure to COVID‐19 in the workplace, these requirements stopped short of mandatory vaccination policies.5 Polling reportedly suggested over 75% of Australians agreed with mandatory COVID‐19 vaccination for “frontline workers in aged care and other vulnerable settings”, with agreement slightly higher among older respondents.6 However, legal questions, including human rights and the right to bodily autonomy, were raised along with practical issues such as the possibility of medical contraindications among workers.7
Despite evidence that vaccination of workers in residential care settings provides indirect protection of residents at high risk,8 coverage rates are commonly low and campaigns to increase coverage are often unsuccessful.9,10 Mandatory vaccination has been proposed as a mechanism for increasing vaccination coverage rates,10 especially when coverage rates remain low, and justified on the basis of shielding susceptible residents and protecting workers from occupational exposure to vaccine‐preventable diseases.11 However, mandates should follow less restrictive, non‐coercive measures, ideally occurring after other options have been exhausted; should take place in consultation with those affected; should be clearly justified and take account of individual consequences; and should not be used as a solution for access issues or in response to vaccine hesitancy.12
Australia was one of the first countries internationally to mandate COVID‐19 vaccination. In April 2021, Italy became the first European country to mandate vaccination for health care workers, including those working in aged care, through a governmental emergency decree.13 In July, Greece, France and the United Kingdom followed, announcing vaccination requirements coming into effect over the period to October 2021.14 Other countries such as Saudi Arabia, Turkmenistan, Indonesia and New Zealand mandated vaccination for a broader range of workers or for all adults.15,16
While some countries exercised a more cautious approach, Australia acted decisively to protect vulnerable RACF residents, based on emerging evidence about the effectiveness of COVID‐19 vaccines to reduce transmission as well as to protect against severe disease.17 Studies have demonstrated the effectiveness of vaccinating workers in aged and other long term care facilities,18,19,20 although continued vigilance around non‐pharmaceutical infection prevention and control interventions was also required to mitigate transmission and optimise outcomes for residents.21,22 A resurgence of COVID‐19 infection among vaccinated health care workforces was also reported, potentially linked to waning immunity and the need to maintain vaccination status.23
Planning and preparation
Following advice from the Australian Health Protection Principal Committee and the Aged Care Advisory Group, the National Cabinet assessed potential timing of a vaccination mandate. Key challenges for the program included the demanding nature of decision making, requiring a balance between ethical concerns and public health imperatives, and the need to respond rapidly to evolving pandemic conditions. The health and wellbeing of aged care residents had become an appropriately high stakes issue following several highly publicised outbreaks in RACFs, leading to elevated levels of community concern with little tolerance for placing any residents at further risk and calls for government intervention.
Once announced, a lead time of almost 12 weeks was provided to ensure sufficient notice for people to navigate concerns and arrange vaccination, and to allow an iterative process of layered implementation with development of an evolving narrative around the case for vaccination. Two weeks ahead of the announcement, mandatory reporting requirements were introduced through new federal legislation, requiring all RACFs to report on staff vaccination rates. This was an important foundation for subsequent policy implementation and provided visibility on progress leading up to the effective date of the mandate (Box 1). Staff vaccination rates were available at facility, organisation and primary health network level.
A key operational risk identified during planning included the possibility of reflexive workforce shock or attrition in response to the burden placed on individual staff. The Australian aged care sector employs a large cohort of casual staff; many work multiple jobs and have few leave entitlements to accommodate vaccine side effects.24 Announcement of the vaccination mandate was accompanied by an $11 million Residential Aged Care COVID‐19 Employee Vaccination Support Grant to assist RACFs with costs associated with arranging off‐site vaccinations for staff.25 Government in‐reach clinics were also offered to all RACFs, so that workers could access vaccination at their workplace. In addition, workers had priority access to vaccinations through dedicated hubs, primary care (general practice and Commonwealth vaccination centres), and state and territory mass vaccination clinics. The national COVID‐19 Vaccine Claims Scheme26 provided additional assurance that financial support would be available if people experienced serious side effects from vaccination.
Communication and engagement
Preparations were supplemented by targeted communications to the aged care sector, ensuring that workers and facilities understood the implications of the mandate, as well as where and how they could be vaccinated. A series of webinars allowed workers in each state and territory to ask questions of representatives from the Commonwealth, state/territory governments, and their unions. A national evidence‐based communications campaign, developed in consultation with relevant unions and the community, disseminated written resources via employer organisations. This included resources in languages other than English, acknowledging the cultural and linguistic diversity of much of the aged care workforce.
Aged care provider organisations were actively engaged and highly supportive throughout the implementation process. State offices of the Australian Government Department of Health and Aged Care established phone contact with every approved provider to confirm plans for vaccinating their workforce, and to clarify local issues and constraints. Over 2500 calls were made to key organisational contacts; these links generated a two‐way information flow and provided practical support. Despite strong links to organisations, policymakers also partnered with peak bodies and unions to directly engage individual members of the aged care workforce. Relevant unions were engaged and supportive, providing crucial messaging about the importance and safety of vaccination, advocating for the requirements of the sector, and supporting workers in decision making.
Vaccination delivery
Recognising the importance of providing individuals with adequate opportunities to resolve uncertainties and concerns, and be vaccinated voluntarily before enforcement of a mandate, substantial effort was directed towards optimising access and availability — making it easier to be vaccinated.27 A range of options and opportunities were offered, including a telephone helpline, workplace clinics run either by the Australian Government or aged care provider organisations, and vaccination through primary care providers and state or territory vaccination hubs. Operation COVID Shield,28 the national vaccine rollout taskforce in operation until 1 August 2022, ensured all workers had access to vaccination before the September 2021 deadline.
Most workers received vaccines through mainstream providers, such as local general practices and mass vaccination hubs. While large scale RACF in‐reach activities were initially considered and conducted, these proved more complex and time consuming than anticipated and potentially compromised staff availability for resident care. Subsequently, aged care providers could tender to vaccinate their workers on site, with 1145 clinics conducted across 545 facilities by 30 contracted providers to the end of September 2021. Ultimately, many primary care practices prioritised vaccination of RACF workers; some jurisdictions offered fast‐track lanes and priority access at state vaccination hubs. Financial support was also offered to general practices to voluntarily provide in‐reach services,29 with 482 vaccination clinics provided to 226 RACFs in this way as of September 2021.
Implementation of the mandate occurred at a time when vaccine hesitancy was being reported in Australia, despite a background of relatively high vaccination rates. This particularly occurred in response to emerging data and complex messaging around the risks of thrombosis with thrombocytopenia syndrome following receipt of Vaxzevria (AstraZeneca). The introduction of Comirnaty (Pfizer–BioNTech) in early July 2021 alleviated some of these concerns. Comirnaty was made available to all RACF workers as a priority group, regardless of age, and despite limited availability of initial supplies and age restrictions on eligibility. Widespread, freely available vaccines, with choice of vaccine and provider, were important counterpoints to promote acceptance and balance introduction of the mandate.
Supporting and monitoring progress
Regular interaction occurred between the Commonwealth and state and territory jurisdictions, which each developed public health orders outlining vaccination requirements and timing, sometimes providing grace periods to achieve compliance. Provider organisations worked diligently to engage staff and offer positive support for decision making, although it was reported that some staff delayed vaccination, or chose to stop working in this setting rather than be vaccinated. Based on mandatory reporting data, the national RACF workforce reduced in size by about 4.1% between 1 September and 1 October 2021, compared with a reduction of 0.4% between 16 July and 16 August. While around 42.5% of these departures occurred between 16 and 20 September, total staffing numbers quickly stabilised from October onwards (Australian Government Department of Health and Aged Care, My Aged Care service provider portal, unpublished data, March 2022).
Vaccination data were actively tracked, using targeted contact with provider organisations to monitor and drive uptake. Healthdirect, the national health advice line, was engaged to make over 7000 calls to 2800 RACFs to promote data integrity and maximise reporting accuracy. Data were shared collaboratively with primary health networks and state and territory health services that were active locally, providing support to vaccination providers and RACFs. First dose vaccination rates by facility were published;30 a powerful strategy that garnered media attention and provided transparency to RACF residents, families and the broader community.
On 17 September 2021, as the mandate came into effect, 97.8% of 261 732 reported RACF workers had received at least a first dose of COVID‐19 vaccine (Box 2); by 14 October this had risen to 99.8%, with 91.8% having received two doses of a vaccine, and 726 (0.3%) meeting exemption criteria,30 which were determined by states and territories in line with individual public health orders.31 Ongoing monitoring data at 21 March 2022 are reported in Box 3; in October 2022, over 99% of Australian aged care workers remain vaccinated with at least two doses.
Despite concerns about the risk of workforce attrition and absenteeism affecting service delivery capability, mandatory vaccination was successfully implemented in the nation's aged care sector, demonstrating the commitment of Australia's aged care workforce to the safety of residents. While the imminent mandate was an important policy driver, the iterative and layered nature of the road to implementation was equally important. Vaccination mandates were subsequently recommended for disability workers and in‐home aged care workers,32,33 and for health care workers in some states and territories.
Box 1 – Implementation timeline for mandatory vaccination in residential aged care during 2021
|
Date |
Milestone |
||||||||||||||
|
|
|||||||||||||||
|
June |
|
||||||||||||||
|
8 |
Operation COVID Shield announced, coordinated by National COVID Vaccine Taskforce |
||||||||||||||
|
15 |
Mandatory reporting requirements legislated — all RACFs required to report on staff vaccination rates, although individual staff could not be forced to disclose vaccination status |
||||||||||||||
|
28 |
National Cabinet agreed to mandate first dose vaccination for RACF workers, effective 17 September 2021 |
||||||||||||||
|
July |
|
||||||||||||||
|
1 |
Residential Aged Care COVID‐19 Employee Vaccination Support Grant announced |
||||||||||||||
|
7 |
Primary care clinics commenced administering Comirnaty (Pfizer–BioNTech) vaccinations, prioritising RACF workers; dedicated vaccination clinics, including in‐reach clinics for RACF workers and residents not yet vaccinated, commenced |
||||||||||||||
|
9 |
All RACF workers became eligible for Comirnaty vaccine regardless of age |
||||||||||||||
|
18 |
Hotline for aged care worker vaccination support opened |
||||||||||||||
|
19 |
Twice‐weekly meetings with unions and peak representative bodies commenced |
||||||||||||||
|
22 |
RACF workers able to access disability clinics for vaccination |
||||||||||||||
|
August |
|
||||||||||||||
|
6 |
Government support for primary care vaccine providers to deliver dedicated workplace‐based clinics began |
||||||||||||||
|
9 |
Western Australia: public health orders introduced, effective 17 Sept — first dose by 17 Sept, fully vaccinated by 17 Nov, detailed exemptions |
||||||||||||||
|
11 |
South Australia: public health orders introduced, effective 17 Sept — first dose by 17 Sept, with evidence of a second dose booking, detailed exemptions |
||||||||||||||
|
14 |
Victoria: public health orders introduced, effective 14 Oct — at least first dose by 17 Sept, with booking for second dose by 15 Nov, or booking for first dose by 1 Oct, detailed exemptions |
||||||||||||||
|
15 |
Tasmania: public health orders introduced, effective 17 Sept — all required doses by 17 Sept, detailed exemptions |
||||||||||||||
|
17 |
Queensland: mandate introduced — first dose by 16 Sept, all prescribed doses by 31 Oct, detailed exemptions |
||||||||||||||
|
19 |
Northern Territory: mandate introduced — first dose by 17 Sept, second dose by 31 Oct, no exemptions |
||||||||||||||
|
22 |
Interactive map released showing national RACF workforce vaccination |
||||||||||||||
|
24 |
Australian Capital Territory: mandate introduced — first dose by 16 Sept, no second dose determination, few exemptions and medical evidence required |
||||||||||||||
|
25 |
Targeted projects to locally engage low‐uptake or at‐risk providers established |
||||||||||||||
|
26 |
New South Wales: mandate introduced — first dose before 17 Sept, second dose by 25 Oct, medical exemptions only |
||||||||||||||
|
25‐27 |
State‐based webinar series for RACF workers in WA, SA, Queensland and Tasmania conducted |
||||||||||||||
|
September |
|
||||||||||||||
|
1‐10 |
State‐based webinar series for RACF workers in NSW, ACT, NT and Victoria conducted |
||||||||||||||
|
7 |
Residential aged care staff exemption reporting commenced; Victorian public health order rolling series effective |
||||||||||||||
|
16 |
ACT public health order effective 11.59 pm |
||||||||||||||
|
17 |
Mandatory vaccinations for residential aged care workers commenced; Tasmania, NT and SA public health orders effective; WA public health order effective 12.01 am; NSW public health order effective 9 am |
||||||||||||||
|
23 |
Commonwealth compliance program commenced — support for RACFs to plan for compliance, educate and recruit staff including focus on second dose rates |
||||||||||||||
|
30 |
Queensland public health order effective 1.00 am; Victorian public health order grace period ends |
||||||||||||||
|
|
|||||||||||||||
|
RACF = residential aged care facility. |
|||||||||||||||
Box 2 – Progressive change in vaccination status for the Australian aged care workforce using mandatory reporting data
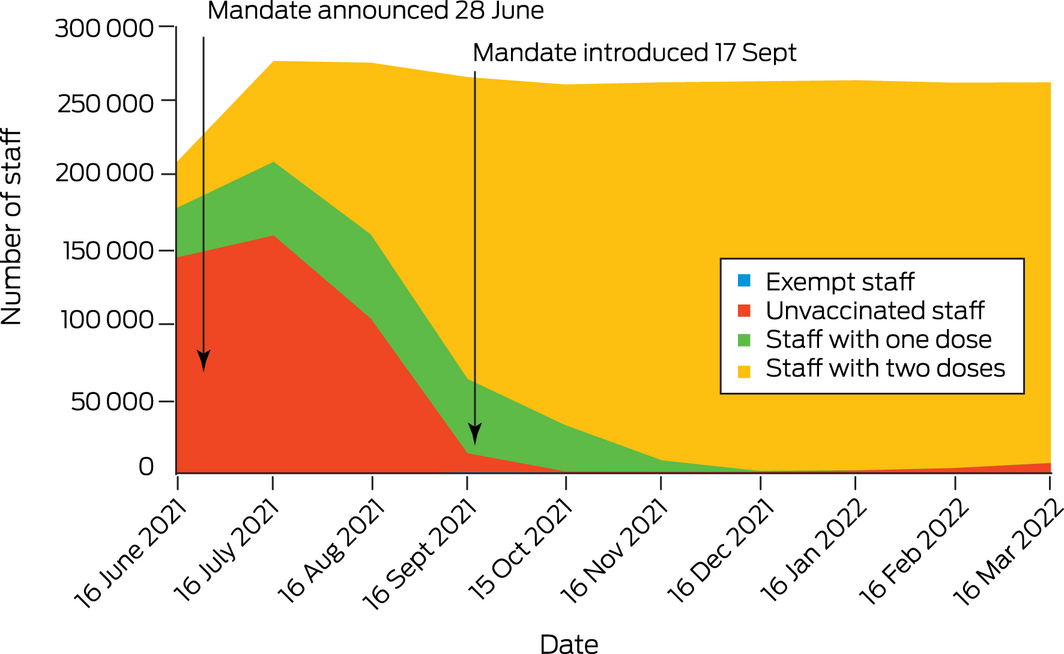
Source: Australian Government Department of Health and Aged Care, My Aged Care service provider portal, unpublished data, March 2022.
Box 3 – Staff vaccination progress at 21 March 2022
- 2845 residential aged care facilities reporting data for 261 851 aged care workers
- 458 staff (0.2%) exempt from vaccination
- 690 789 doses administered
- 255 036 (97.6%) staff had received dose 1
- 254 987 (97.6%) had received dose 2
- 180 766 (69.2%) had received boosters
Provenance: Not commissioned; externally peer reviewed., doi:
- 1. Morrison S. National Cabinet statement, 28 June 2021. PM Transcripts: Transcripts from the Prime Ministers of Australia. https://pmtranscripts.pmc.gov.au/release/transcript‐44077 (viewed Oct 2022).
- 2. Frati P, La Russa R, Di Fazio N, et al. Compulsory vaccination for healthcare workers in Italy for the prevention of SARS‐CoV‐2 infection. Vaccines (Basel) 2021; 9: 966.
- 3. Gostin LO, Salmon DA, Larson HJ. Mandating COVID‐19 vaccines. JAMA 2021; 325: 532‐533.
- 4. Maltezou HC, Botelho‐Nevers E, Brantsæter AB, et al. Vaccination of healthcare personnel in Europe: update to current policies. Vaccine 2019; 37: 7576‐7584.
- 5. Safe Work Australia. Aged care vaccination. https://covid19.swa.gov.au/covid‐19‐information‐workplaces/industry‐information/aged‐care/vaccination (viewed Oct 2022).
- 6. Martin S. More than 75% of Australians support compulsory Covid vaccines for aged care staff. The Guardian 2021; 7 June. https://www.theguardian.com/australia‐news/2021/jun/07/more‐than‐75‐of‐australians‐support‐compulsory‐covid‐vaccines‐for‐aged‐care‐staff (viewed Oct 2022).
- 7. Kevat DA, Panaccio DC, Pang SC, et al. Medico‐legal considerations of mandatory COVID‐19 vaccination for high risk workers. Med J Aust 2021; 215: 22‐24. https://www.mja.com.au/journal/2021/215/1/medico‐legal‐considerations‐mandatory‐covid‐19‐vaccination‐high‐risk‐workers
- 8. van Delden, JJ, Ashcroft, R, Dawson, A, et al. The ethics of mandatory vaccination against influenza for health care workers. Vaccine 2008; 26: 5562‐5566.
- 9. Boey, L, Roelants, M, Vandermeulen, C. Increased vaccine uptake and less perceived barriers toward vaccination in long‐term care facilities that use multi‐intervention manual for influenza campaigns. Hum Vaccin Immunother 2021; 17: 673‐680.
- 10. FitzSimons D, Hendrickx G, Lernout T, et al. Incentives and barriers regarding immunization against influenza and hepatitis of health care workers. Vaccine 2014; 32: 4849‐4854.
- 11. Maltezou, HC, Poland, GA. Vaccination policies for healthcare workers in Europe. Vaccine 2014; 32: 4876‐4880.
- 12. Leask J, Seale H, Williams JH, et al. Policy considerations for mandatory COVID‐19 vaccination from the Collaboration on Social Science and Immunisation. Med J Aust 2021; 215: 499‐503. https://www.mja.com.au/journal/2021/215/11/policy‐considerations‐mandatory‐covid‐19‐vaccination‐collaboration‐social
- 13. Paterlini, M. Covid‐19: Italy makes vaccination mandatory for healthcare workers. BMJ 2021; 373: n905.
- 14. Wise J. Covid‐19: France and Greece make vaccination mandatory for healthcare workers. BMJ 2021; 374: n1797.
- 15. Reuters. FACTBOX – Countries making COVID‐19 vaccines mandatory. Thomson Reuters Foundation News, 8 Oct 2021. https://news.trust.org/item/20210804140458‐ari9l (viewed Nov 2021).
- 16. Employment New Zealand. Vaccines and the workplace. https://www.employment.govt.nz/leave‐and‐holidays/other‐types‐of‐leave/coronavirus‐workplace/covid‐19‐vaccination‐and‐employment (viewed Nov 2021).
- 17. Haas EJ, Angulo FJ, McLaughlin JM, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS‐CoV‐2 infections and COVID‐19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet 2021; 397: 1819‐1829.
- 18. Muhsen K, Maimon N, Mizrahi A, et al. Effectiveness of BNT162b2 mRNA COVID‐19 vaccine against acquisitions of SARS‐CoV‐2 among health care workers in long‐term care facilities: a prospective cohort study. Clin Infect Dis 2022; 75: e755‐e763.
- 19. Cavanaugh AM, Fortier S, Lewis P. COVID‐19 outbreak associated with a SARS‐CoV‐2 R.1 lineage variant in a skilled nursing facility after vaccination program — Kentucky, March 2021. MMWR Morb Mortal Wkly Rep 2021; 70: 639‐643.
- 20. Moustsen‐Helms IR, Emborg H‐D, Nielsen J, et al. Vaccine effectiveness after 1 dose of the BNT162b2 mRNA Covid‐19 vaccine in long‐term care facility residents and healthcare workers – a Danish cohort study [preprint]. medRxiv 2021.03.08.21252200; 9 Mar 2021. https://doi.org/10.1101/2021.03.08.21252200 (viewed Oct 2022).
- 21. Love J, Keegan LT, Angulo FJ, et al. Continued need for non‐pharmaceutical interventions after COVID‐19 vaccination in long‐term‐care facilities. Sci Rep 2021; 11: 18093.
- 22. Westhölter D, Taube C. SARS‐CoV‐2 outbreak in a long‐term care facility after vaccination with BNT162b2. Clin Infect Dis 2021; 73: 2147‐2148.
- 23. Keehner J, Horton L, Binkin N, et al. Resurgence of SARS‐CoV‐2 infection in a highly vaccinated health system workforce. N Engl J Med 2021; 385: 1330‐1332.
- 24. Hall Dykgraaf S, Desborough J, Kelaher C et al. COVID 19 highlights risks of healthcare and social care workers attending work while ill. Aust J Gen Pract 2020; 49; doi: https://doi.org/10.31128/AJGP‐COVID‐23.
- 25. Australian Government Department of Health and Aged Care. New: Residential Aged Care COVID‐19 Employee Vaccination Support Grant. 2 July 2021. https://www.health.gov.au/news/newsletters/new‐residential‐aged‐care‐covid‐19‐employee‐vaccination‐support‐grant (viewed Mar 2022).
- 26. Australian Government Department of Health and Aged Care. COVID‐19 vaccine claims scheme. https://www.health.gov.au/initiatives‐and‐programs/covid‐19‐vaccine‐claims‐scheme (viewed Dec 2021).
- 27. Seale H. Evidence supports mandatory COVID vaccination for aged care workers. But we need to make it easier too. The Conversation 2021; 29 June. https://theconversation.com/evidence‐supports‐mandatory‐covid‐vaccination‐for‐aged‐care‐workers‐but‐we‐need‐to‐make‐it‐easier‐too‐163569 (viewed Mar 2022).
- 28. Australian Government Department of Health and Aged Care. Op COVID Shield: National COVID Vaccine Campaign Plan. Canberra: Australian Government, 2021. https://www.health.gov.au/resources/publications/op‐covid‐shield‐national‐covid‐vaccine‐campaign‐plan (viewed Oct 2022).
- 29. Australian Government Department of Health and Aged Care. COVID‐19 vaccination – Practice Incentives Program COVID‐19 in‐reach vaccination payment guidelines. https://www.health.gov.au/resources/publications/covid‐19‐vaccination‐practice‐incentives‐program‐covid‐19‐in‐reach‐vaccination‐payment‐guidelines (viewed Mar 2022).
- 30. Australian Government Department of Health and Aged Care. Residential aged care worker COVID‐19 vaccination rates map. https://www.health.gov.au/resources/apps‐and‐tools/residential‐aged‐care‐worker‐covid‐19‐vaccination‐rates‐map/residential‐aged‐care‐worker‐covid‐19‐vaccination‐rates‐map (accessed Mar 2022).
- 31. Australian Government Department of Health and Aged Care. Mandatory COVID‐19 vaccination in aged care. https://www.health.gov.au/initiatives‐and‐programs/covid‐19‐vaccines/information‐for‐aged‐care‐providers‐workers‐and‐residents‐about‐covid‐19‐vaccines/mandatory‐covid‐19‐vaccination‐in‐aged‐care#temporary‐exemptions‐to‐covid19‐vaccination (viewed July 2022).
- 32. Australian Government Department of Health. Australian Health Protection Principal Committee (AHPPC) statement on mandating vaccination for disability support workers. 10 Nov 2021. https://www.health.gov.au/news/australian‐health‐protection‐principal‐committee‐ahppc‐statement‐on‐mandating‐vaccination‐for‐disability‐support‐workers (viewed Mar 2022).
- 33. Australian Government Department of Health and Aged Care. Australian Health Protection Principal Committee (AHPPC) statement on mandatory vaccination of aged care in‐home and community aged care workers. 10 Nov 2021. https://www.health.gov.au/news/australian‐health‐protection‐principal‐committee‐ahppc‐statement‐on‐mandatory‐vaccination‐of‐aged‐care‐in‐home‐and‐community‐aged‐care‐workers (viewed Mar 2022).






Open access
Open access publishing facilitated by Australian National University, as part of the Wiley ‐ Australian National University agreement via the Council of Australian University Librarians.
We acknowledge the contribution of members of the Australian Government Department of Health and Aged Care vaccine rollout branch and the National COVID‐19 Vaccine Taskforce disability and aged care rollout division, as well as the Australian Health Protection Principal Committee, whose work underpins the policy responses described in this paper.
Paul Kelly and Michael Kidd are employed by the Australian Government Department of Health and Aged Care, and were instrumental in development of policy measures described in the article. Sally Hall Dykgraaf, Jane Desborough, Anne Parkinson and Elizabeth Sturgiss are, or have been, seconded to the Australian Government Department of Health and Aged Care, undertaking embedded action research, including the preparation of this article.