Invasive group A streptococcal (iGAS) disease is an important cause of morbidity and mortality in the Northern Territory, particularly among people who require dialysis.1 iGAS disease has been notifiable in the NT since 2011,2 and nationally since July 2021.3
Since November 2014, people undergoing haemodialysis in the Top End region of the NT during the wet season (November–April) have routinely received antibiotic prophylaxis for melioidosis (supervised oral trimethoprim–sulfamethoxazole [TMP/SMX] 160/800 mg after dialysis, three times per week),4 which may also prevent iGAS disease.5 We therefore reviewed the incidence of iGAS disease in the NT over ten years and assessed the impact of TMP/SMX prophylaxis on its incidence among people undergoing dialysis.
We identified cases of iGAS disease diagnosed during 1 May 2011 – 30 April 2021 in the NT Notifiable Diseases System, and retrieved the corresponding electronic health records. The iGAS case definition required isolation of GAS from a normally sterile site or the site of necrotising fasciitis, confirmed by culture or nucleic acid testing. Severe iGAS disease was defined as including pneumonia, meningitis, necrotising fasciitis, toxic shock syndrome, or another manifestation requiring intensive care admission or causing death. Antibiotic prescribing data were obtained from the NT Enterprise Data Warehouse. Population data were retrieved from the NT Health Renal Unit and Population and Digital Health Unit.6 Our study was approved by the NT Human Research Ethics Committee (2021‐4125).
A total of 692 cases of iGAS disease were identified; 511 patients were Indigenous Australians (74%), 380 were women (55%), and 131 were receiving haemodialysis (19%). The median age at diagnosis was 50 years (interquartile range, 37–63 years). GAS was cultured from blood in 652 cases (94%). Of the 378 cases for which severity was reported, 135 met the criteria for severe iGAS disease (36%). Thirty‐day all‐cause mortality was 6% (40 deaths).
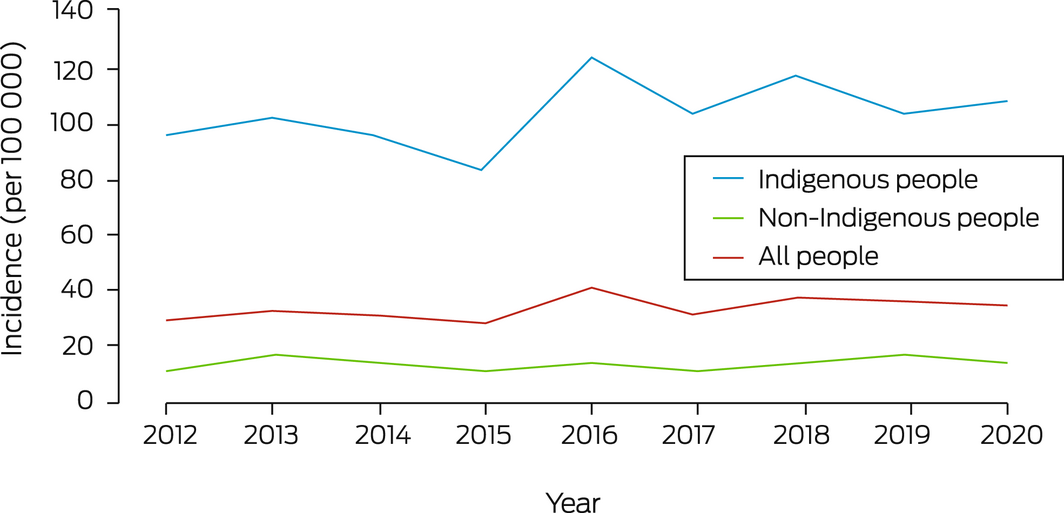
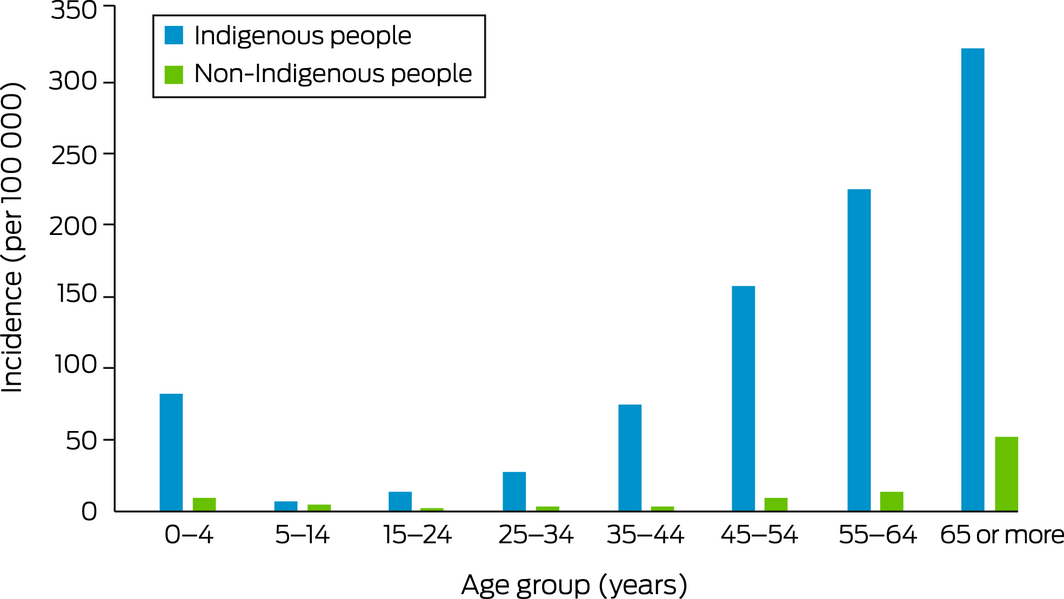
The overall age‐standardised incidence of iGAS disease in the NT during the study period was 34.3 (95% confidence interval [CI], 31.4–37.1) cases per 100 000 population (Box 1). The incidence was fairly stable over time (Box 2), but increased with age group, and was higher for Indigenous than non‐Indigenous Territorians in all age groups (Box 3).
Of 626 people receiving haemodialysis in the Top End, 506 (81%) were prescribed TMP/SMX melioidosis prophylaxis during 1 November 2014 – 30 April 2018. The annual proportion has increased since the initiation of routine prescribing (data not shown). TMP/SMX was prescribed on 183 625 of 451 346 wet season haemodialysis patient‐days (41%).
No cases of iGAS disease were recorded for dialysis patients prescribed regular TMP/SMX during the wet season melioidosis prophylaxis period. Wet season iGAS disease incidence among Top End people receiving haemodialysis but not prescribed TMP/SMX at diagnosis was 1122 (95% CI, 412–2441) cases per 100 000 patients.
The persistently high rates of iGAS disease in the NT indicate that an intersectoral response to improving the social determinants of skin health is needed, particularly in remote communities. The recent listing of iGAS disease as nationally notifiable is an important step toward reducing the burden of GAS‐related disease in Australia. As the people at greatest risk of iGAS disease may benefit from antibiotic prophylaxis, we recommend that a prospective trial and holistic cost–benefit analysis be undertaken.
Box 1 – Invasive group A streptococcal disease in the Northern Territory, 1 May 2011 – 30 April 2021
|
|
Northern Territory |
Top End |
Central Australia |
||||||||||||
|
Population group |
Number |
Incidence (95% CI) |
Number |
Incidence (95% CI) |
Number |
Incidence (95% CI) |
|||||||||
|
|
|||||||||||||||
|
All persons* |
692 |
34.3 (31.4–37.1) |
386 |
23.2 (20.6–25.8) |
306 |
82.2 (71.8–92.7) |
|||||||||
|
Women* |
380 |
37.3 (33.2–41.4) |
188 |
22.1 (18.7–25.5) |
192 |
98.5 (83.2–114) |
|||||||||
|
Men* |
312 |
31.6 (27.5–35.6) |
198 |
24.2 (20.3–28.0) |
114 |
66.3 (51.5–81.0) |
|||||||||
|
Indigenous Australians* |
511 |
106 (95.0–117) |
256 |
71.5 (61.3–81.7) |
255 |
172 (148–197) |
|||||||||
|
Non‐Indigenous Australians* |
181 |
14.0 (11.7–16.3) |
130 |
11.7 (9.4–13.9) |
51 |
28.0 (19.2–36.7) |
|||||||||
|
People receiving haemodialysis† |
131 |
1643 (1374–1950) |
50 |
1120 (831–1476) |
81 |
2041 (1621–2537) |
|||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Age‐standardised incidence (per 100 000 population), based on 2001 Australian census data as the reference population,7 and corrected for partial years of population in 2011 (244 days included) and 2021 (119 days included). † Crude incidence. [Correction added on 11 October 2022 after first online publication: the incidence (95% CI) values for Northern Territory, Top End and Central Australia for all population groups except people receiving haemodialysis have been updated.] |
|||||||||||||||
Received 9 March 2022, accepted 7 September 2022
- 1. Boyd R, Patel M, Currie BJ, et al. High burden of invasive group A streptococcal disease in the Northern Territory of Australia. Epidemiol Infect 2016; 144: 1018‐1027.
- 2. Minister for Health (Northern Territory of Australia). Notifiable Diseases Act. Notifiable diseases: amendment of information to be given by laboratories. Government Gazette, 11 May 2011; p. 9. https://nt.gov.au/__data/assets/pdf_file/0007/197278/g19.pdf (viewed Sept 2022).
- 3. Communicable Diseases Network Australia. Invasive group A streptococcal (iGAS) disease: surveillance case definition. Updated 25 June 2021. https://www.health.gov.au/resources/collections/cdna‐surveillance‐case‐definitions?utm_source=health.gov.au&utm_medium=callout‐auto‐https://www.health.gov.au/resources/publications/invasive‐group‐a‐streptococcal‐disease‐igas‐surveillance‐case‐definition (viewed Jan 2022).
- 4. Majoni SW, Hughes JT, Heron B, Currie BJ. Trimethoprim+sulfamethoxazole reduces rates of melioidosis in high‐risk hemodialysis patients. Kidney Int Rep 2018; 3: 160‐167.
- 5. Bowen AC, Lilliebridge RA, Tong SYC, et al. Is Streptococcus pyogenes resistant or susceptible to trimethoprim‐sulfamethoxazole? J Clin Microbiol 2012; 50: 4067‐4072.
- 6. Population and Digital Health (NT Health). Northern Territory Health District resident population estimates 1971–2021 [internal document]. Updated July 2022.
- 7. Australian Bureau of Statistics. 2001 Census data. Canberra: ABS, 2001. Updated June 2017. https://www.abs.gov.au/websitedbs/censushome.nsf/home/historicaldata2001?opendocument&navpos=280 (viewed Aug 2022).





We thank all Northern Territory Health clinical and laboratory staff involved in the patients’ care. We acknowledge Kimberley McMahon (NT Centre for Disease Control) and Nancy Merridew (NT Health) for their valued contributions to the iGAS public health response in the NT, which prompted this investigation. For assistance with data extraction we thank Emidio Coccetti (NT Health), and for assistance with data analysis Chris Lowbridge (Menzies School of Health Research) and Ramakrishna Chondur, Libby Morris, and Karen Dempsey (NT Public Health and Digital Team).
No relevant disclosures.