Otitis media and associated hearing loss are highly prevalent in Indigenous Australian children.1 Most relevant prevalence studies have been undertaken in rural and remote regions, although most Indigenous children live in urban areas.2 One prospective cohort study found that hearing loss was frequent in young Aboriginal children in a semi‐arid zone of Western Australia,3 but its prevalence in Aboriginal infants in urban areas has not been investigated.4 We therefore estimated the prevalence of hearing loss in Aboriginal infants in Perth, Western Australia, enrolled in the Djaalinj Waakinj cohort study (2017–2021),5 and examined the association between otitis media and hearing responses.
The Djaalinj Waakinj methodology has been described in detail elsewhere.5 Infants underwent routine ear health screenings in their homes at 2–4, 6–8, and 12–18 months of age. A formal hearing assessment was conducted at 9–12 months of age, using free‐field visual reinforcement audiometry in a sound‐treated room to determine hearing responses at 500, 1000, 2000, and 4000 Hz.6 The mean hearing response for the more sensitive ear was classified as normal (25 dB), mild (26–40 dB), moderate (41–60 dB) and severe hearing loss (61 dB or more).7
The presence of middle ear effusion was assessed using tympanometry. Findings were classified by an audiologist: type A tympanograms were deemed to indicate normal middle ear function (no otitis media), type B tympanograms probable otitis media, and type C tympanograms probable Eustachian tube dysfunction. The Djaalinj Waakinj study was approved by the Western Australian Aboriginal Human Ethics Committee (WAAHEC #759) and the Child and Adolescent Health Services Human Ethics Research Committee (CAHS HREC #12).
Sixty‐seven of the 125 enrolled infants completed formal hearing assessments (mean age, 12.1 months; standard deviation, 2.3 months; range, 9–21 months); 41 were boys (61%). Twenty‐one of the 67 infants (31%) had normal hearing, 46 (69%) had some degree of hearing loss (mean response, 36.0 dB; 95% confidence interval [CI], 33.3–38.7 dB), including 22 with mild (33%) and 24 with moderate hearing loss (36%). Mean hearing responses were poorer for the 35 infants with abnormal tympanograms at the time of hearing assessment (40.7 dB; 95% CI, 37.0–44.9 dB) than for the 30 infants with normal tympanograms (30.9 dB; 95% CI, 27.8–33.6 dB) (Box).
Our finding that 69% of urban Aboriginal infants in our study had hearing loss at about twelve months of age is comparable with that of a similar study in Kalgoorlie (65%).3 Hearing assessments in infants are based on minimum response levels rather than hearing thresholds,6 which probably explains the apparent mild hearing loss in infants with normal tympanograms. The mean hearing response in these children was nevertheless about 10 dB better than in infants with abnormal tympanograms.
The mean hearing response in infants with abnormal tympanograms was 40.7 dB, a level at which they would not hear normal voices clearly, with implications for later speech, language, and behavioural development.8 Our findings support early monitoring of otitis media and hearing loss in Indigenous children, with prompt referral for audiological assessment as recommended by Australian otitis media guidelines.1
Box – Mean frequency‐specific hearing responses (with 95% confidence intervals) for Aboriginal infants (about twelve months of age), by tympanogram type*
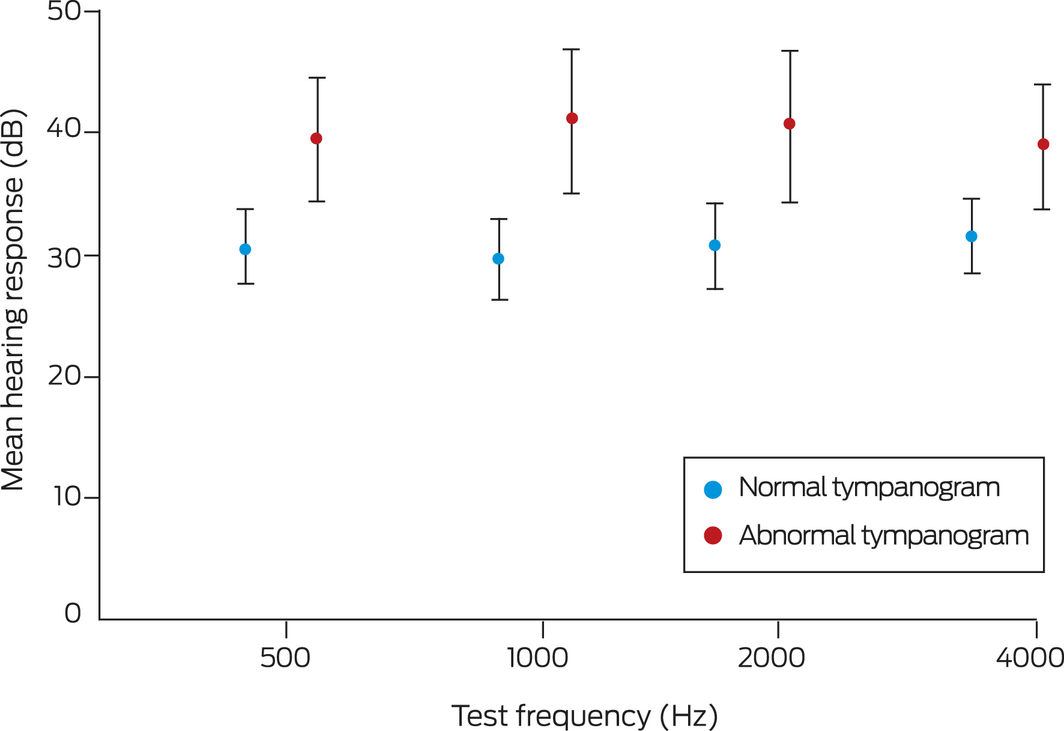
* Normal: type A tympanogram (30 infants); abnormal: type B (30 infants) or type C (five infants). Tympanograms were not available for two infants. Visual reinforcement audiometry was performed with GSI 61 (Grason–Stadler), Equinox (Interacoustics), and Avant (MedRx) audiometers, using pure tone, warble, or filtered narrowband noise stimuli through loudspeakers one metre from the child’s ear at an angle of 90°. Tympanometry was conducted using either Titan Middle Ear Analyser (Interacoustics) or GSI 39 or MI 44 tympanometers (Maico).
Received 7 February 2022, accepted 11 April 2022
- 1. Leach AJ, Morris PS, Coates HL, et al. Otitis media guidelines for Australian Aboriginal and Torres Strait Islander children: summary of recommendations. Med J Aust 2021; 214: 228‐233. https://www.mja.com.au/journal/2021/214/5/otitis‐media‐guidelines‐australian‐aboriginal‐and‐torres‐strait‐islander
- 2. Jennings W, Spurling G, Shannon B, et al. Rapid review of five years of Aboriginal and Torres Strait Islander health research in Australia: persisting under‐representation of urban populations. Aust N Z J Public Health 2021; 45: 53‐58.
- 3. Lehmann D, Weeks S, Jacoby P, et al; Kalgoorlie Otitis Media Research Project Team. Absent otoacoustic emissions predict otitis media in young Aboriginal children: a birth cohort study in Aboriginal and non‐Aboriginal children in an arid zone of Western Australia. BMC Pediatrics 2008; 8: 32.
- 4. Kaspar A, Leach AJ. Hearing loss among Australian Aboriginal infants and toddlers: a systematic review. Public Health in Practice 2020; 1: 100048.
- 5. Swift VM, Doyle JE, Richmond HJ, et al. Djaalinj Waakinj (listening talking). Rationale, cultural governance, methods, population characteristics: an urban Aboriginal birth cohort study of otitis media. Deafness and Education International 2020; 22: 255‐274.
- 6. Widen JE, Folsom RC, Cone‐Wesson B, et al. Identification of neonatal hearing impairment: hearing status at 8 to 12 months corrected age using a visual reinforcement audiometry protocol. Ear Hear 2000; 21: 471‐487.
- 7. Clark JG. Uses and abuses of hearing loss classification. ASHA 1981; 23: 493–500.
- 8. Olusanya BO, Davis AC, Hoffman HJ. Hearing loss grades and the International classification of functioning, disability and health. Bull World Health Organ 2019; 97: 725‐728.






Open access
Open access publishing facilitated by The University of Western Australia, as part of the Wiley ‐ The University of Western Australia agreement via the Council of Australian University Librarians.
This investigation was supported by a research grant from the Western Australia Department of Health Telethon–Perth Children’s Hospital Research Fund and by the Wesfarmers Centre for Vaccines and Infectious Diseases at the Telethon Kids Institute. Chris Brennan‐Jones was supported by a National Health and Medical Research Council Fellowship (GNT 1142897) and a Western Australian Department of Health Emerging Leader Fellowship. We acknowledge that this research was undertaken on Noongar Whadjuk Boodja, and acknowledge their Elders past, present and emerging. We acknowledge all members of the Djaalinj Waakinj team and the Aboriginal Community Advisory Group (listed in reference 5).
No relevant disclosures.