The known: One priority for mental health care is to reduce the long term impact of emerging mental disorders. However, diverse trajectories of functioning restrict effective service planning.
The new: The functional levels of two in three young people who attended early intervention services remained poor or deteriorated and fluctuated across two years of care. Prior mental health care or self‐harm and suicidality, physical comorbidity, substance misuse, and social disengagement were associated with poor outcomes.
The implications: Most young people with emerging mental disorders require dynamic, multidisciplinary, measurement‐based approaches that take into account physical comorbidity, ambiguous or attenuated symptomatology, and social or occupational complexity.
One in four young people experience mental ill health by the age of 25.1 As these disorders typically emerge during adolescence and early adulthood, they often have functional outcomes that extend into later life.2 Consequently, responding early is the key to reducing their overall impact.
The value of early intervention is supported by evidence that the longer the period of untreated illness, the poorer the outcomes.3 Early intervention clinics attract young people with sub‐threshold or early stage disorders,4 many of whom are already subject to substantial functional impairment, comorbidity, and suicidality.5,6 The heterogeneity of symptoms, risk, and functioning at their first presentation means that providing timely interventions that meet all of a young person’s needs can be difficult.7 Short term reductions in psychological distress and risk are typically reported for young people who attend early intervention clinics,8 but most will later experience deterioration of symptoms or chronic functional impairment.5
Trajectory‐based modelling takes into account the heterogeneity of young people who require mental health care by identifying subpopulations of young people, with the aim of guiding service planning and strategies for improving long term functional outcomes.9,10 Our study evaluated trajectories of functioning during the first two years of early intervention care, and identified factors associated with these trajectories.
Methods
We identified our participants in a research registry of 6743 people aged 12–30 years who presented to the youth mental health clinics at the Brain and Mind Centre (University of Sydney) during 1 June 2008 – 31 July 2018. These clinics provide both primary care services (headspace) and more specialised services. The clinics are not diagnosis‐specific, do not impose symptom‐, severity‐, or risk‐based thresholds for care, and attract young people with a broad range of emerging anxiety, depressive, mania‐like, psychosis‐like, and comorbid syndromes. Case management was provided for all participants by clinicians, and clients received appropriate psychological, social, and medical interventions as standard care. Those whose needs exceeded the capacity of the primary care services were referred to more specialised mental health services or were hospitalised.
The inclusion criteria for participation were age 12‒25 years at baseline, and at least three data points between one and 24 months after baseline.
Data collection
Data were extracted from clinical files to a standardised form, as previously described.11 For each participant, their first clinical assessment at the service was defined as the baseline time point, and its date determined each follow‐up time point. All clinical notes from all time points up to and including the current time point were used for completing the standardised form. The data collected were demographic characteristics (sex, age), current engagement in part‐ or full‐time education or employment (yes, or no: “not in education, employment, or training”), and social and occupational functioning as assessed with the Social and Occupational Functioning Assessment Scale (SOFAS).12 Clinical information included in the standardised form were Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM‐5) diagnoses and at‐risk mental states (clusters of symptoms deemed to be risk factors for progression to more severe mental disorders). DSM‐5 diagnoses were labelled primary, secondary, or tertiary diagnoses, but these categories were collapsed for the purposes of this study. Other clinical information collected included history of self‐harm or of suicidal thoughts and behaviours, comorbid physical conditions (eg, diabetes), personal mental illness history, and treatment (medications, hospitalisation) for mental health problems (further details: online Supporting Information: supplementary methods).
Statistical analyses
Analyses were performed in R 3.6.2 (R Foundation for Statistical Computing). We identified trajectories of function using growth mixture modelling of SOFAS scores during two‐year follow‐up.9,10 Time was coded as the number of months since baseline. Models were run with an increasing number of classes (two to seven classes), specifying both linear and quadratic trends over time and using two different covariance structures. Initial parameter values were estimated with an optimisation algorithm, with 100 random starting values.13 The estimates with the best log‐likelihood after ten iterations were used. The posterior probabilities for each trajectory were calculated for each participant, and people were assigned to the trajectory with the greatest probability. The criteria for model selection and adequacy were the lowest Bayesian information criterion value, inclusion of at least 5% of the participants by each class, mean predictive probabilities of assignment greater than 70% for each class, and a relative entropy value exceeding 0.5.9,10 Associations of factors with class membership were examined by multinomial logistic regression, and expressed as odds ratios (ORs) with 95% confidence intervals (CIs).
Ethics approval
The study was approved by the University of Sydney Human Research Ethics Committee (2008/5453, 2012/1626). All participants provided written informed consent.
Results
A total of 1510 people aged 12‒25 years satisfied our criteria for inclusion in our study sample. The characteristics of the sample and the 1391 excluded candidates are summarised in the Supporting Information, table 1. The mean age of our participants was 18.1 years (standard deviation, 3.3 years); 930 were female (62%) (Box 1).
Latent class trajectories
A total of 24 models were estimated; the four‐class solution with quadratic terms was the preferred solution, with the lowest Bayesian information criterion for models that identified classes that each contained at least 5% of the population (model 12 in Supporting Information, table 2). The adequacy of the model was confirmed on all criteria: the mean predictive probabilities of assignment (0.59, 0.79, 0.72, 0.71) indicated that the likelihood of correct assignment to the latent classes was high, and the relative entropy value of 0.56 indicated that the classes were reasonably well differentiated. The numbers of follow‐up time points available for each class were similar (Supporting Information, figure 1).
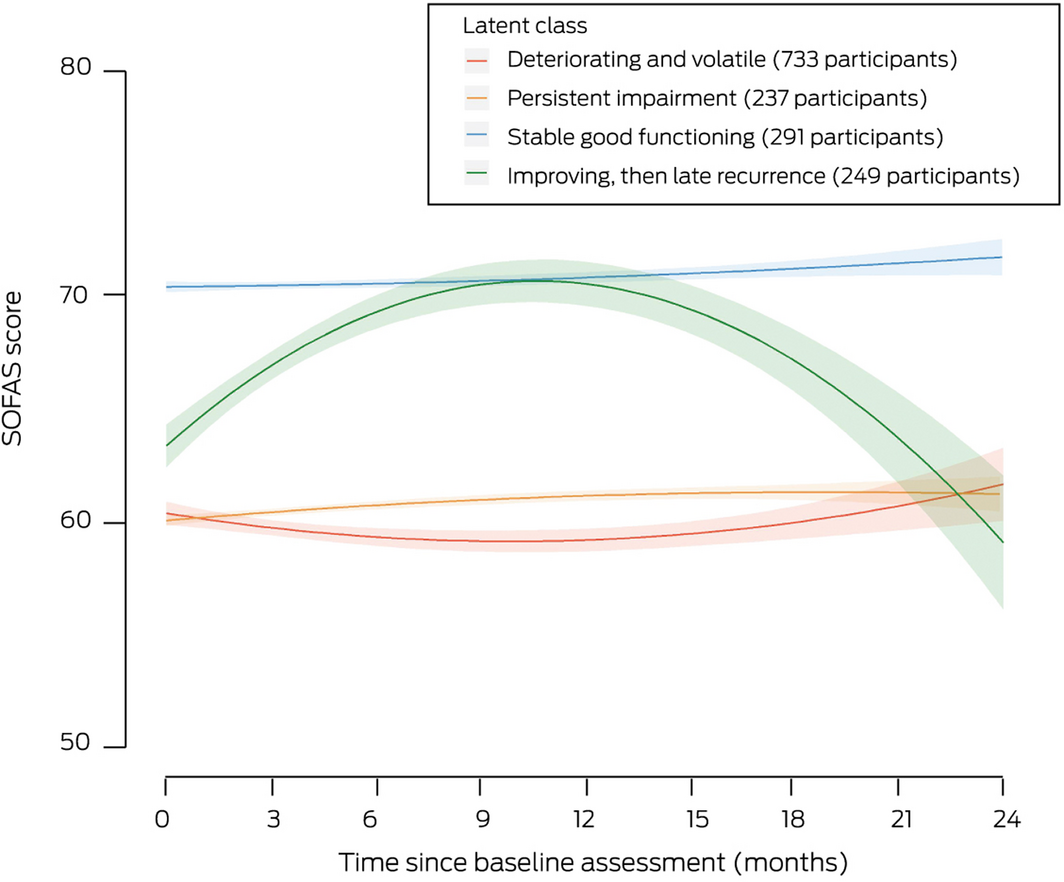
We identified four distinct trajectories of social and occupational functioning (Box 1, Box 2, Box 3):
Box 2 – Latent class trajectories of social and occupational functioning for 1510 people aged 12‒25 years who attended the Brain and Mind Centre clinics for mental health care, 2008‒2018 (with standard error, shaded)
Box 3 – Individual latent class trajectories of social and occupational functioning for 1510 people aged 12‒25 years who attended the Brain and Mind Centre clinics for mental health care, 2008‒2018 (overlayed with summary trajectories)
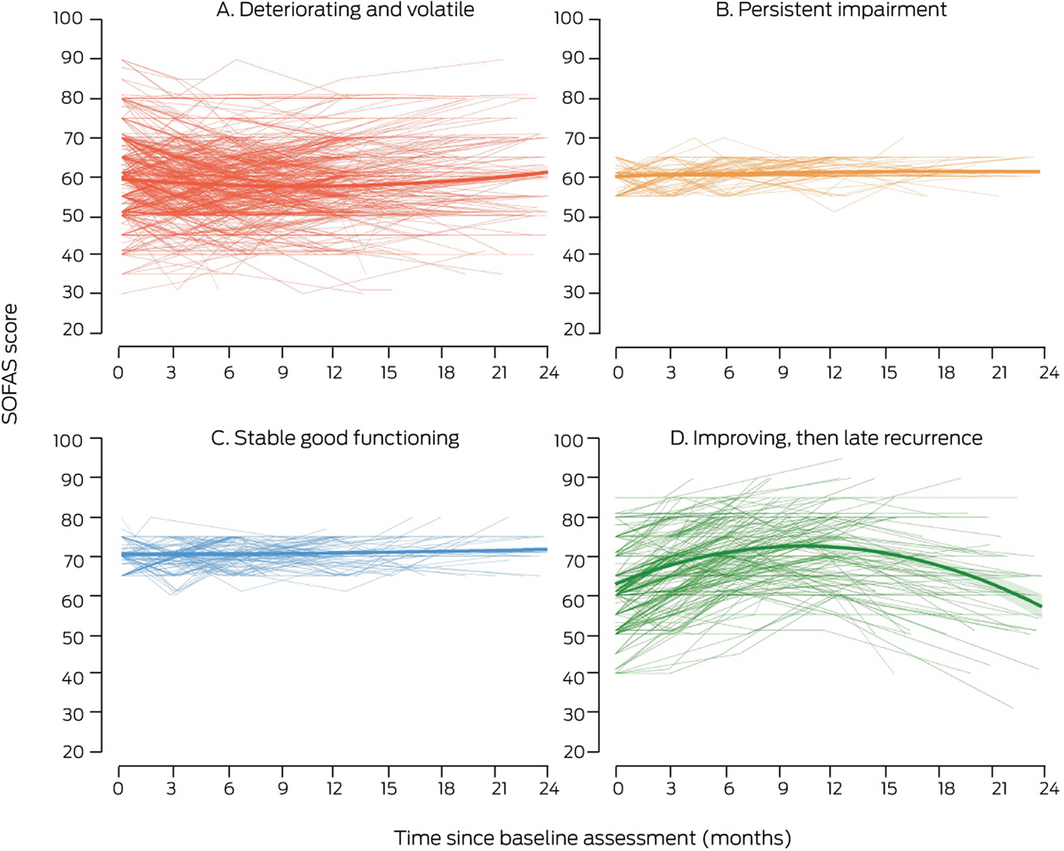
- deteriorating and volatile (733 participants, 49%);
- persistent impairment (237 participants, 16%);
- stable good functioning (291 participants, 19%);
- improving, then late recurrence (249 participants, 16%).
The odds of a “deteriorating and volatile” trajectory were about twice as high as any other trajectory for people with any major physical illness. For people not in education, employment, or training, the odds of a “deteriorating and volatile” trajectory were greater than for “stable good functioning” (OR, 6.03; 95% CI, 3.20–12.6) or “persistent impairment” (OR, 1.61; 95% CI, 1.05–2.51). For people using psychiatric medications (OR, 1.45; 95% CI, 1.04–2.04) or with histories of self‐harm (OR, 1.61; 95% CI, 1.13–2.31), the odds of a “deteriorating and volatile” trajectory were greater than for “improving, then late recurrence”. The odds were greater than for “stable good functioning” for people with substance‐related disorders (OR, 2.22; 95% CI, 1.12–4.82), and people who had been hospitalised for mental illness (OR, 2.21; 95% CI, 1.12–4.64), had a childhood onset mental disorder (OR, 1.99; 95% CI, 1.19–3.46), or had attempted suicide (OR, 1.96; 95% CI, 1.05–3.82); the odds declined with increasing age (per year: OR, 0.94; 95% CI, 0.89–0.99). For people with bipolar disorder (OR, 2.37; 95% CI, 1.08–5.40) or psychosis‐like experiences (OR, 1.86; 95% CI, 1.17–3.06), the odds of a “deteriorating and volatile” trajectory were greater than for “persistent impairment” (Box 4).
For people with histories of self‐harm, the odds of “persistent impairment” were greater than for “improving, then late recurrence” (OR, 1.60; 95% CI, 1.04–2.49). For people who were older (per year: OR, 0.93; 95% CI, 0.88–0.99) or had bipolar disorder (OR, 0.33; 95% CI, 0.11–0.92), the odds of “persistent impairment” were lower than for “stable good functioning”; they were greater for people who were not in education, employment, or training (OR, 5.13; 95% CI, 2.39–11.9), had childhood onset mental disorders (OR, 2.48; 95% CI, 1.34–4.69), or had attempted suicide (OR, 2.64; 95% CI, 1.29–5.57) (Box 4).
The odds of an “improving, then late recurrence” trajectory were greater than of “stable good function” for people who were not in education, employment, or training (OR, 3.65; 95% CI, 1.72–8.37), who had been hospitalised (OR, 2.92; 95% CI, 1.32–6.80), or who had attempted suicide (OR, 2.22; 95% CI, 1.07–4.73); they were lower for people with a history of self‐harm (OR, 0.63; 95% CI, 0.41–0.96) (Box 4).
Discussion
The functional trajectories of young people visiting early intervention services were quite heterogeneous, but only 35% had good functional outcomes over two years; that is, only one in three people maintained an initially good level of function or substantially improved from a lower level of function. In contrast, functional impairment persisted in nearly two‐thirds of participants, or their level of function deteriorated and was volatile. Our findings suggest that the current primary care‐based model meets the needs of only a minority of young people seeking care, and that most require more comprehensive and multidisciplinary approaches because of substantial comorbidity, ambiguous or attenuated symptomatology, and social or occupational complexity.
Early intervention services for young people with non‐specific anxiety and mood syndromes typically employ basic stepped care approaches with an emphasis on brief psychological therapies, in the expectation that more specialised care will be needed only by those with major mood or psychotic disorders. This approach has significant clinical benefits for people with mild impairment, as brief psychological interventions are effective for reducing psychological distress, and can marginally improve functioning.14 However, differentiating young people with reasonable or good baseline functioning from those with impaired or poor functioning is a key factor that should be considered (alongside other clinical variables) to determine whether personalised care is needed, as well as the appropriate type, intensity, sequence, and duration of multidisciplinary services. This approach, aligned with optimal models of mental health care, should be an explicit component of youth mental health service provision.15
The group of young people with relatively good baseline levels of function that were maintained during early intervention care had lower rates of comorbidity, childhood onset mental illness, and social disengagement (that is, they were usually employed or in education) than the other groups. The rates of bipolar disorder and of self‐harm or suicidality in this group were higher than for people with persistent impairment or with an improving but late recurrence trajectory, suggesting that it includes young people with mild illness who benefit from brief primary care‐based interventions, but also people who have experienced serious mental problems in the past that had been well managed. Similarly, participants in the improving but late recurrence trajectory group had lower rates of comorbidity and of self‐harm and suicidality than people with persistent impairment or on a deteriorating and volatile trajectory.
Young people with persistent impairment or on deteriorating and volatile trajectories have substantial needs that extend beyond the syndromes with which they present, encompassing broader impacts on their physical health, social and occupational disengagement, self‐harm and suicidality, and substance abuse.16 For example, having a major physical illness was associated with a deteriorating and volatile trajectory, confirming that physical comorbidity complicates treatment and is associated with poorer overall outcomes.17 Early intervention services often neglect the physical health needs of young people, but early recognition and treatment of such ailments should be a priority to improve mental health outcomes.18 Similarly, not being in education, employment or training distinguished these young people from those with stable good functioning, indicating the need for additional support, even for those without serious or full threshold disorders.19 They may require more complex, personalised multidisciplinary interventions not typically offered by early intervention services, such as vocational rehabilitation and individual placement and support.20
More young people in the two less favourable trajectory groups had histories of mental illness than in the other two groups, as indicated by recorded hospitalisation, psychiatric medication use, or childhood onset of mental illness. When planning the intensity of treatment, understanding a young person’s history of illness is important, regardless of their functioning at baseline, because it may indicate a more severe and recurring condition.21 One feature that distinguished participants on an improving but late recurrence trajectory from those with stable good functioning was that they more likely to have been hospitalised for mental illness and to have a history of attempted suicide. Such a history may indicate a risk of recurrence and need for more frequent monitoring, whether function improves in the short term or not. Taken together, our findings indicate that comorbidity and complexity influence long term functioning, supporting our greater emphasis on multidimensional assessment and outcome tools, rather than diagnosis‐oriented systems (eg, early psychosis), as the basis for service provision.
Despite the diversity of individual functional trajectories (Box 3), we identified three groups of participants with relatively stable courses. The largest group, however, was that of young people with deteriorating and volatile trajectories. Any individual’s trajectory can oscillate between health and disorder as a function of vulnerability and protective and treatment factors.17 However, most treatment plans are driven by broad guidelines based on population effects or clinical experience, which can be inaccurate and inconsistent.22 They often do not recognise the dynamic nature of the disorders and needs of the individual, and service provision is accordingly characterised by low rates of change in the type or intensity of the interventions employed, suggesting inadequate outcome monitoring.23 Our findings highlight the importance of measurement‐based care, whereby outcomes are monitored to inform more personalised and responsive treatment,24 a core component of the chronic care model that supports more informed clinical decisions.25 Despite evidence for its effectiveness and its feasibility in medical disease management,25 measurement‐based care is largely unused in youth mental health care.
Limitations
As our study included young people receiving a variety of primary and secondary health care services, conclusions about the effects of specific treatments cannot be drawn. However, the outcome trajectories were determined under real world conditions, in which the delivery of treatment is less controlled and more variable than in controlled trials. Our study was therefore suited to investigating questions about outcomes for young people in whom trans‐diagnostic disorders, complexity, and comorbidity were common. Further, our sample was restricted to young people who remained in contact with the service for at least two years. We could not assess the longer term functional outcomes for those who did not remain in contact, perhaps biasing our sample towards people who required ongoing care and were accordingly more likely to have poorer outcomes.
The SOFAS is a somewhat crude measure of functioning, but is commonly used in clinical practice and research because it is simple and practical. It was appropriate for broadly and reliably tracking overall individual functional progress during early intervention care. Other measures of social and occupational functioning could be considered for obtaining information about changes in specific social or occupational domains, useful for decisions about appropriate interventions.
Our choice of model was based on standard metrics of model fit and adequacy, but the choice will have influenced the allocation of individuals to trajectory types, given the large within‐group variation for some classes. We limited the set of predictors used, excluding a range of important factors of predictive utility, such as neurocognition and imagining.26 While the variables we included were indicators typically recorded at initial presentation by young people with mental health problems (increasing the generalisability of our findings), including other predictors, such as social determinants of health, could lead to further valuable insights.
Conclusion
We identified several distinct trajectories of functional outcomes during two years of early intervention care for a heterogeneous group of young people with a variety of mental problems. As two‐thirds of these people had generally poor functional outcome patterns, our findings offer important insights into the limitations of current primary care‐based, low intensity, and psychologically focused stepped care provided by early intervention services. The effects in such services of more sophisticated, multidimensional assessment, measurement‐based care tools, and more dynamic, personalised and intensive multidisciplinary care packages, should be evaluated.
Box 1 – Baseline characteristics of the study participants, by latent trajectory
|
Characteristic |
All participants |
Persistent impairment |
Deteriorating and volatile |
Improving, then late recurrence |
Stable good functioning |
||||||||||
|
|
|||||||||||||||
|
Number of participants |
1510 |
237 |
733 |
249 |
291 |
||||||||||
|
Demographic characteristics |
|
|
|
|
|
||||||||||
|
Age (years), mean (SD) |
18.1 (3.3) |
17.9 (3.2) |
18.0 (3.3) |
18.2 (3.3) |
18.2 (3.3) |
||||||||||
|
Sex (female) |
930 (61.6%) |
142 (59.9%) |
436 (59.5%) |
153 (61.4%) |
199 (68.4%) |
||||||||||
|
Not in education, employment or training |
238 (15.8%) |
33 (13.9%) |
157 (21.4%) |
38 (15.3%) |
10 (3.4%) |
||||||||||
|
Clinical presentation |
|
|
|
|
|
||||||||||
|
Depression |
1039 (68.8%) |
165 (69.6%) |
484 (66.0%) |
173 (69.5%) |
218 (74.9%) |
||||||||||
|
Anxiety |
1067 (70.7%) |
173 (73.0%) |
491 (67.0%) |
176 (70.7%) |
226 (77.7%) |
||||||||||
|
Bipolar disorder |
143 (9.5%) |
14 (5.9%) |
83 (11%) |
19 (7.6%) |
27 (9.3%) |
||||||||||
|
Psychosis |
79 (5.2%) |
12 (5.1%) |
46 (6.3%) |
15 (6.0%) |
6 (2%) |
||||||||||
|
Mania‐like experiences |
215 (14.2%) |
32 (14%) |
121 (16.5%) |
29 (12%) |
33 (11%) |
||||||||||
|
Psychosis‐like experiences |
280 (18.5%) |
34 (14%) |
169 (23%) |
44 (18%) |
33 (11%) |
||||||||||
|
Circadian disturbance |
223 (14.8%) |
28 (12%) |
123 (16.8%) |
29 (12%) |
42 (14%) |
||||||||||
|
Substance‐related disorder |
119 (7.9%) |
23 (9.7%) |
69 (9.4%) |
17 (6.8%) |
10 (3.4%) |
||||||||||
|
Personal history of mental illness |
|
|
|
|
|
||||||||||
|
Any childhood disorder |
219 (14.5%) |
39 (16%) |
128 (17.5%) |
33 (13%) |
20 (6.9%) |
||||||||||
|
Any family history |
733 (48.5%) |
110 (46.4%) |
367 (50.1%) |
118 (47.4%) |
138 (47.4%) |
||||||||||
|
Physical comorbid conditions |
|
|
|
|
|
||||||||||
|
Any major physical illness |
279 (18.5%) |
29 (12%) |
174 (23.7%) |
38 (15%) |
38 (13%) |
||||||||||
|
Treatment for mental illness |
|
|
|
|
|
||||||||||
|
Any hospitalisation |
200 (13.2%) |
27 (11%) |
119 (16.2%) |
40 (16%) |
12 (4.1%) |
||||||||||
|
Any psychiatric medication |
719 (47.6%) |
111 (46.8%) |
394 (53.8%) |
107 (43.0%) |
106 (36.4%) |
||||||||||
|
Self‐harm and suicidal thoughts and behaviours |
|
|
|
|
|
||||||||||
|
Self‐harm |
669 (44.3%) |
109 (46.0%) |
342 (46.7%) |
92 (37%) |
125 (43.0%) |
||||||||||
|
Suicide ideation |
755 (50.0%) |
124 (52.3%) |
385 (52.5%) |
124 (49.8%) |
121 (41.6%) |
||||||||||
|
Suicide attempt |
227 (15.0%) |
38 (16%) |
136 (18.6%) |
38 (15%) |
15 (5.2%) |
||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. |
|||||||||||||||
Box 4 – Factors that influence latent class membership: multinomial logistic regressions (odds ratios with 95% confidence intervals)
|
|
Deteriorating and volatile |
Persistent impairment |
Improving, then late recurrence |
||||||||||||
|
|
v persistent impairment |
v improving, then late recurrence |
v stable good functioning |
v improving, then late recurrence |
v stable good functioning |
v stable good functioning |
|||||||||
|
|
|||||||||||||||
|
Demographic characteristics |
|
|
|
|
|
|
|||||||||
|
Age (per year) |
1.00 |
0.97 |
0.94 |
0.96 |
0.93 |
0.99 |
|||||||||
|
Sex (male) |
1.01 |
1.15 |
1.22 |
1.17 |
1.31 |
1.12 |
|||||||||
|
Not in education, employment, or training |
1.61 |
1.38 |
6.03 |
1.00 |
5.13 |
3.65 |
|||||||||
|
Clinical presentation |
|
|
|
|
|
|
|||||||||
|
Depression |
1.02 |
0.89 |
0.70 |
0.89 |
0.78 |
0.72 |
|||||||||
|
Anxiety |
0.79 |
0.93 |
0.72 |
1.11 |
0.89 |
0.75 |
|||||||||
|
Bipolar disorder |
2.37 |
1.16 |
0.56 |
0.47 |
0.33 |
0.37 |
|||||||||
|
Psychosis |
0.70 |
0.79 |
1.18 |
1.32 |
2.38 |
1.18 |
|||||||||
|
Mania‐like experiences |
0.68 |
1.13 |
1.32 |
1.91 |
2.11 |
1.15 |
|||||||||
|
Psychosis‐like experiences |
1.86 |
1.28 |
1.45 |
0.73 |
0.94 |
1.23 |
|||||||||
|
Circadian disturbance |
1.33 |
1.32 |
0.98 |
1.09 |
0.63 |
0.68 |
|||||||||
|
Substance‐related disorder |
0.80 |
1.33 |
2.22 |
1.42 |
2.25 |
1.22 |
|||||||||
|
Personal history of mental illness |
|
|
|
|
|
|
|||||||||
|
Any childhood disorder |
1.03 |
1.16 |
1.99 |
1.14 |
2.48 |
1.66 |
|||||||||
|
Any family history |
1.14 |
0.99 |
1.04 |
0.93 |
1.02 |
1.03 |
|||||||||
|
Physical health conditions |
|
|
|
|
|
|
|||||||||
|
Any major physical illness |
2.18 |
1.74 |
1.98 |
0.80 |
0.96 |
1.31 |
|||||||||
|
Treatment use |
|
|
|
|
|
|
|||||||||
|
Any hospitalisation |
1.29 |
0.63 |
2.21 |
0.53 |
1.79 |
2.92 |
|||||||||
|
Any psychiatric medication |
1.02 |
1.45 |
1.39 |
1.36 |
1.31 |
1.00 |
|||||||||
|
Self‐harm and suicidal thoughts and behaviours |
|
|
|
|
|
|
|||||||||
|
Self‐harm |
1.01 |
1.61 |
0.85 |
1.60 |
0.98 |
0.63 |
|||||||||
|
Suicide ideation |
0.96 |
0.96 |
1.40 |
0.99 |
1.47 |
1.42 |
|||||||||
|
Suicide attempts |
0.90 |
0.99 |
1.96 |
1.01 |
2.64 |
2.22 |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 27 September 2020, accepted 13 July 2021
- Frank Iorfino1
- Joanne S Carpenter1
- Shane PM Cross1
- Jacob Crouse1
- Tracey A Davenport1
- Daniel F Hermens2
- Hannah Yee1
- Alissa Nichles1
- Natalia Zmicerevska1
- Adam Guastella1
- Elizabeth M Scott1
- Ian B Hickie1
- 1 Brain and Mind Centre, the University of Sydney, Sydney, NSW
- 2 Thompson Institute, University of the Sunshine Coast, Birtinya, QLD
We thank all the young people who participated in this study, and all the staff in the Youth Mental Health Team at the University of Sydney Brain and Mind Centre, past and present, who contributed to this work.
Elizabeth Scott is the medical director of the Young Adult Mental Health Unit at St Vincent’s Hospital in Darlinghurst, the Adult Mental Health discipline leader in the University of Notre Dame School of Medicine, a research affiliate at the University of Sydney, and a consultant psychiatrist. She has received honoraria for educational seminars related to the clinical management of depressive disorders supported by Servier and Eli‐Lilly, participated in a national advisory board for the antidepressant compound Pristiq (Pfizer), and was the national coordinator of an antidepressant trial sponsored by Servier. Ian Hickie was inaugural commissioner of the National Mental Health Commission (2012‒18). He is co‐director (health and policy) of the Brain and Mind Centre (BMC), University of Sydney. The BMC operates early intervention youth services under contract to headspace. Ian Hickie has previously led community‐based and pharmaceutical industry‐supported (Wyeth, Eli Lilly, Servier, Pfizer, AstraZeneca) projects on the identification and better management of anxiety and depression. He was a member of the medical advisory panel for Medibank Private until October 2017, a board member of the Psychosis Australia Trust, and a member of the Veterans’ Mental Health Clinical Reference Group. He is the Chief Scientific Advisor to, and a 5% equity shareholder in, InnoWell Pty Ltd. InnoWell was formed by the University of Sydney (45% equity) and PwC Australia (45% equity) to deliver the $30 million Australian government‐funded Project Synergy (2017‒20), a three‐year program for the transformation of mental health services, and to lead transformation of mental health services internationally through the use of innovative technologies.
- 1. Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet 2011; 377: 2093–2102.
- 2. Copeland WE, Wolke D, Shanahan L, Costello EJ. Adult functional outcomes of common childhood psychiatric problems: a prospective, longitudinal study. JAMA Psychiatry 2015; 72: 892–899.
- 3. Ghio L, Gotelli S, Marcenaro M, et al. Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta‐analysis. J Affect Disord 2014; 152: 45–51.
- 4. Hickie I, Scott EM, Hermens DF, et al. Applying clinical staging to young people who present for mental health care. Early Interv Psychiatry 2013; 7: 31–43.
- 5. Iorfino F, Hermens D, Cross SPM, et al. Delineating the trajectories of social and occupational functioning of young people attending early intervention mental health services in Australia: a longitudinal study. BMJ Open 2018; 8: e020678.
- 6. Iorfino F, Hermens DF, Cross SPM, et al. Prior suicide attempts predict worse clinical and functional outcomes in young people attending a mental health service. J Affect Disord 2018; 238: 563–569.
- 7. Voineskos AN. Predicting functional outcomes in early‐stage mental illness: prognostic precision medicine realized? JAMA Psychiatry 2018; 75: 1105–1106.
- 8. Rickwood DJ, Mazzer KR, Telford NR, et al. Changes in psychological distress and psychosocial functioning in young people visiting headspace centres for mental health problems. Med J Aust 2015; 202: 537–142. https://www.mja.com.au/journal/2015/202/10/changes‐psychological‐distress‐and‐psychosocial‐functioning‐young‐people
- 9. Lennon H, Kelly S, Sperrin M, et al. Framework to construct and interpret latent class trajectory modelling. BMJ Open 2018; 8: e020683.
- 10. Van De Schoot R, Sijbrandij M, Winter SD, et al. The GRoLTS‐checklist: guidelines for reporting on latent trajectory studies. Structural Equation Modeling 2017; 24: 451–467.
- 11. Carpenter JS, Iorfino F, Cross S, et al. Cohort profile: the Brain and Mind Centre Optymise cohort: tracking multidimensional outcomes in young people presenting for mental healthcare. BMJ Open 2020; 10: e030985.
- 12. Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM‐IV: a review of measures of social functioning. Am J Psychiatry 1992; 149: 1148–1156.
- 13. Biernacki C, Celeux G, Govaert G. Choosing starting values for the EM algorithm for getting the highest likelihood in multivariate Gaussian mixture models. Computational Studies and Data Analysis 2003; 41: 561–575.
- 14. Cross SP, Hermens DF, Hickie IB. Treatment patterns and short‐term outcomes in an early intervention youth mental health service. Early Interv Psychiatry 2016; 10: 88–97.
- 15. Hickie IB, Scott EM, Cross SP, et al. Right care, first time: a highly personalised and measurement‐based care model to manage youth mental health. Med J Aust 2019; 211 (9 Suppl): S3–S46. https://www.mja.com.au/journal/2019/211/9/right‐care‐first‐time‐highly‐personalised‐and‐measurement‐based‐care‐model
- 16. Iorfino F, Carpenter JS, Cross SP, et al. Multidimensional outcomes in youth mental health care: what matters and why? Med J Aust 2019; 211 (9 Suppl): S4–S11. https://www.mja.com.au/journal/2019/211/9/right‐care‐first‐time‐highly‐personalised‐and‐measurement‐based‐care‐model
- 17. Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007; 370: 851–858.
- 18. Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry 2019; 6: 675–712.
- 19. Brinchmann B, Widding‐Havneraas T, Modini M, et al. A meta‐regression of the impact of policy on the efficacy of individual placement and support. Acta Psychiatr Scand 2020; 141: 206–220.
- 20. Killackey E, Allott K, Jackson HJ, et al. Individual placement and support for vocational recovery in first‐episode psychosis: randomised controlled trial. Br J Psychiatry 2019; 214: 76–82.
- 21. Ormel J, Oerlemans AM, Raven D, et al. Functional outcomes of child and adolescent mental disorders. Current disorder most important but psychiatric history matters as well. Psychol Med 2017; 47: 1271–1282.
- 22. Ægisdóttir S, White MJ, Spengler PM, et al. The meta‐analysis of clinical judgment project: fifty‐six years of accumulated research on clinical versus statistical prediction. Counseling Psychologist 2006; 34: 341–382.
- 23. Richards DA, Bower P, Pagel C, et al. Delivering stepped care: an analysis of implementation in routine practice. Implement Sci 2012; 7: 3.
- 24. Hickie IB. The role of new technologies in monitoring the evolution of psychopathology and providing measurement‐based care in young people. World Psychiatry 2020; 19: 38–39.
- 25. Tam H, Ronan K. The application of a feedback‐informed approach in psychological service with youth: systematic review and meta‐analysis. Clin Psychol Rev 2017; 55: 41–55.
- 26. Lee RSC, Hermens DF, Naismith SL, et al. Neuropsychological and functional outcomes in recent‐onset major depression, bipolar disorder and schizophrenia‐spectrum disorders: a longitudinal cohort study. Transl Psychiatry 2015; 5: e555.





Abstract
Objective: To identify trajectories of social and occupational functioning in young people during the two years after presenting for early intervention mental health care; to identify demographic and clinical factors that influence these trajectories.
Design: Longitudinal, observational study of young people presenting for mental health care.
Setting: Two primary care‐based early intervention mental health services at the Brain and Mind Centre (University of Sydney), 1 June 2008 – 31 July 2018.
Participants: 1510 people aged 12‒25 years who had presented with anxiety, mood, or psychotic disorders, for whom two years’ follow‐up data were available for analysis.
Main outcome measures: Latent class trajectories of social and occupational functioning based on growth mixture modelling of Social and Occupational Assessment Scale (SOFAS) scores.
Results: We identified four trajectories of functioning during the first two years of care: deteriorating and volatile (733 participants, 49%); persistent impairment (237, 16%); stable good functioning (291, 19%); and improving, but late recurrence (249, 16%). The less favourable trajectories (deteriorating and volatile; persistent impairment) were associated with physical comorbidity, not being in education, employment, or training, having substance‐related disorders, having been hospitalised, and having a childhood onset mental disorder, psychosis‐like experiences, or a history of self‐harm or suicidality.
Conclusions: Two in three young people with emerging mental disorders did not experience meaningful improvement in social and occupational functioning during two years of early intervention care. Most functional trajectories were also quite volatile, indicating the need for dynamic service models that emphasise multidisciplinary interventions and measurement‐based care.