The known: The renewed National Cervical Screening Program includes a new clinician‐supported self‐collection pathway, but its acceptability among practitioners and participants is unknown.
The new: Self‐collection was highly acceptable to most screening participants and practitioners. However, key implementation barriers, including difficulty in identifying eligible screening participants and interpreting guidelines, reduced the capacity of primary care providers to offer self‐collection.
The implications: In order to realise the full potential of the self‐collection pathway to reduce the burden of cervical cancer, systems and resources are needed that help practitioners and their practices identify underscreened women and provide adequate support for completing the pathway.
In December 2017, the renewed National Cervical Screening Program (rNCSP) commenced operation in Australia, moving from two‐yearly Papanicolaou smear tests (Pap tests) to five‐yearly human papillomavirus (HPV) testing.1 The rNCSP also introduced the option of an alternative screening pathway that allows self‐collected vaginal samples to be used for HPV testing of women and other people with cervixes (“screening participants”) aged 30 years or more, who had not been screened for at least four years since their last Pap test, or had never been screened and had declined clinician‐collected cervical screening tests (Supporting Information, 1).2 Primary care plays a critical role, as testing of a self‐collected sample in Australia must be facilitated by a primary care practitioner3 rather than using mail‐to‐all or door‐to‐door strategies described overseas.4,5
Australia is on track to meeting the World Health Organization target for eliminating cervical cancer as a public health problem.6,7 However, there are inequities in the current program related to socio‐economic status, remoteness of residence, and Indigenous status.8 Cervical cancer is more common in people who are not regularly screened,9 including those for whom the rNCSP is not culturally safe or is unacceptable for other reasons, including previous trauma.10,11,12 The availability of self‐collection offers a possibility to reduce these inequities by mitigating reported barriers to screening.10,11,12 Further, evidence that self‐collection is as sensitive as clinician collection for detecting CIN2 and CIN3 lesions4 may help overcome practitioners’ reservations about the accuracy of testing self‐collected samples. Ultimately, the capacity of self‐collection to improve equity depends on the extent to which self‐collection is implemented in primary care and is acceptable to women. In studies in Australia and overseas, self‐collection has improved the uptake of cervical screening13,14 and was acceptable to screening participants12,15,16,17 and primary care practitioners.17,18
Most studies have either described results from outside Australia or have assessed self‐collection with mail‐out kits. A pilot study, conducted before commencement of the rNCSP, found that a clinician‐supported model of self‐collection increased screening participation and was acceptable to primary care and screening participants.12,14 However, as pilot practices were supported in implementing the pathway, their findings may not be generalisable to routine practice. We therefore examined the acceptability and experience of the self‐collection pathway, as implemented in the rNCSP, for screening participants and for practitioners.
Methods
We undertook a qualitative approach to exploring the acceptability and implementation experience of the self‐collection pathway2 from the perspectives of screening participants and practitioners who had used the pathway within the rNCSP.
Sampling strategy
Data on the users of the self‐collection pathway who used the pathway during 1 December 2017 – 30 April 2019, provided by VCS Pathology (the sole laboratory in Victoria accredited to test self‐collected samples during this period), were used to develop a robust sampling frame that allowed recruitment from subgroups of pathway users (Supporting Information, 2).
Recruitment
Screening participants were recruited in a two‐stage process: VCS Pathology forwarded a letter to the screening participant’s primary care practitioner, who could opt out on behalf of their patient; if they did not, an invitation letter was forwarded to the screening participant. Practitioners were recruited by letters sent by VCS Pathology. At each stage, participants had 14 days to opt out of further contact. If no reply was received during the opt‐out periods, the participant’s contact details were provided to the investigators, who then contacted participants by phone to assess interest in participating in an interview. Participants were recruited during July – November 2019, and the interviews were held during July – December 2019.
Data collection
Trained qualitative researchers individually interviewed screening participants and practitioners in semi‐structured interviews. Informed consent was obtained from each interviewee to record the interview, with the exception of one participant for whom comprehensive written notes were taken with their consent. For screening participants who had negative HPV test results from self‐collected tests, the interview centred on their experience of the self‐collection pathway and the circumstances that led them to the pathway. For the few screening participants with positive test results, we also explored their experience with the follow‐up pathway, including the need for a clinician‐collected cervical screening test for those positive for HPV types not 16/18. Interviews with practitioners focused on their experiences of implementing the self‐collection pathway (using the model of care implemented in their practice), including processes for identifying eligible participants and their perceptions of self‐collection.
Analysis
To ensure data integrity and validity, all audio transcripts were crossed‐checked before analysis. Interviews were analysed by template analysis in NVivo 12 (QSR International). In this form of thematic analysis, a coding framework is developed on the basis of a set of a priori themes informed by the literature, such as barriers to and facilitators of cervical screening and the acceptability of the pathway, prior to coding.19 Throughout analysis, the coding framework underwent several revisions as themes were identified on the basis of the responses (Supporting Information, 3). Screening participant (author NC) and practitioner transcripts (author CZ) were each analysed individually. Throughout revisions, author MK crossed‐checked the coding framework to ensure consistency within and between samples.
Ethics approval
The University of Melbourne Medicine and Dentistry Human Ethics committee approved the study (19540446.2).
Results
Forty‐five of 193 invited screening participants (23%) and 18 of 50 invited medical practitioners (36%) were recruited (Box 1, Box 2). Our analysis focused on the acceptability and uptake of the self‐collection pathway, the different models of care employed, and barriers to implementing the pathway efficiently.
Acceptability of the self‐collection pathway
The self‐collection pathway was highly acceptable as an alternative cervical screening pathway for screening participants and practitioners (Box 3). Most screening participants (39, 87%) described the experience of self‐collection as “pleasant” and “positive”, and reported that self‐collection provided greater control over one’s health:
I guess it was that sense of having control over my own health and it being a choice I can make, it being something I can do myself, rather than it being done to me. Screening participant (31 years), never screened, HPV‐negative
If a self‐collected swab is positive for HPV types not 16/18, clinical practice guidelines recommend that the participant returns for a clinician‐collected cervical screening test.2 Four of the ten participants who had such results reported negative experiences of self‐collection, a larger proportion than other screening participants. The practitioner’s approach to the clinician‐collected cervical screening test was the strongest predictor of the acceptability of the test and self‐collection; if the participant perceived the practitioner as understanding their personal circumstances, a positive experience with the follow‐up clinician‐collected cervical screening test was more likely.
Practitioners regarded self‐collection as a “progressive” change to the rNCSP. They reported that self‐collection was an effective pathway for re‐engaging screening participants who would decline a clinician‐collection cervical screening test:
I definitely think self‐testing has helped me convince some women to participate, that would otherwise not participate in the standard Pap smear. General practitioner, metropolitan private general practice
Awareness and use of the self‐collection pathway
Use of the self‐collection pathway by screening participants was driven more by practitioners offering it, in most cases opportunistically, than by the participants themselves. Many screening participants noted that its availability was the primary reason for undertaking cervical screening at the time of their self‐collection test:
For me, [self‐collection] made the difference between having one and not having [a cervical screening test]. As much as I can flippantly say, well, you have to die of something, I’m not having that invasive procedure [the clinician‐collected cervical screening test] ever again. Screening participant (57 years), underscreened, HPV‐negative
Awareness among screening participants of the self‐collection pathway prior to their first contact with it was low, and some participants reported they would have attended primary care for screening had they known about the pathway:
Given what I’ve told you where I’ve put [cervical screening] off, had I known that [self‐collection] was an option, I would’ve done it when it came out, basically. Screening participant (48 years), underscreened, HPV‐negative
Practitioners had mixed experiences with becoming aware of the self‐collection pathway; some discovered that it was available under the rNCSP only 12 months after its introduction. A practitioner who happened to be interviewed as a screening participant noted that:
I don’t think [self‐collection is] as well known as it should be… I had a conversation with another colleague where I said, I just had to do a self‐collection. She was like, “You do that?” I had to say yes. Then I had to tell her what the [eligibility] criteria is”. Screening participant (36 years), underscreened, HPV‐negative
Different models of care
Practitioners took a patient‐centred approach that considered the participants’ circumstances when integrating the self‐collection pathway into their practice. It was evident, however, that there was confusion about the extent to which the pathway must be facilitated and requested by practitioners. In some practices, screening participants could take the self‐collection test kit home (in accordance with clinical practice guidelines), which was useful for participants who were distressed after a difficult conversation or an unsuccessful cervical screening sample collection attempt:
I definitely don’t feel like I could have done it behind the screen myself because the self‐collection kit was given to me directly after having this kind of difficult conversation with my GP. Screening participant (35 years), underscreened, HPV-positive
Other practitioners interpreted the clinical practice guidelines as indicating that sample collection needed to be directly supervised:
The nurse has to be present in the room while they do the sample. They’re not allowed to take it to the toilet. They’re not allowed to take it at home. Nurse practitioner, rural community health
Uncertainty caused by the limited practical direction in the clinical practice guidelines about the extent to which self‐collection must be facilitated by a practitioner reduced practitioners’ confidence in implementing the pathway.
Eligibility criteria for self‐collection
The eligibility criteria and the requirement to confirm eligibility were key barriers for practitioners implementing the pathway. Practitioners regarded the age range and screening status eligibility criteria as “inflexible” and “narrow”:
The frustration is the time that it takes to ensure that it’s at least four years [since the last cervical screening test] … But then I do a self‐collection and boom, get the call, “No, I can’t do it.” Because it’s three years and 360 days. General practitioner, metropolitan community health
Practitioners identified eligible participants in a variety of ways. Some practices adopted a systematic approach and identified them using practice management software; in others, the individual practitioner requested patient screening histories from the registry. Regardless of the approach, the responsibility fell to primary care, limiting the reach of the self‐collection pathway, and, when a participant’s eligibility for self‐collection was unknown, practitioners opted not to discuss self‐collection as an option for cervical screening.
Discussion
We found that the self‐collection pathway was highly acceptable to screening participants and primary care practitioners. We found that acceptability was lower among participants who were positive for HPV types not 16/18 and therefore required an additional clinician‐collected cervical screening test. Considering the range of barriers to a speculum examination for under‐ or never screened participants, such as pain10 and a history of sexual violence,11 it is unsurprising that acceptability among these participants was variable. As the pathway becomes more available, supporting people with significant barriers to speculum examination through the follow‐up pathway will be crucial, including further education and resources for practitioners, to assist these screening participants during cervical screening test sample collection.
Our finding that the availability of self‐collection in primary care could improve screening participation is consistent with the conclusion drawn from the pilot study.12,14 It is important, however, that primary care practitioners are made aware of new evidence for the sensitivity and specificity of self‐collection sample testing,4 and for the low risk of repeat self‐collection of samples being necessary. At VCS Pathology, the proportion of unsatisfactory self‐collected samples is about 2%; this is similar to the rate for Pap smears (2–5%) but larger than for clinician‐collected samples (0.2%) (David Hawkes [Victorian Cytology Service], personal communication; March 2021). The rNCSP self‐collection pathway has been available to under‐ or never screened participants since 1 December 2017,1,2 but uptake in Victoria has been low. Only 1067 self‐collection tests were performed by 30 April 2019 (the date of our data extraction), whereas 290 000 clinician‐collected cervical screening tests were reported by VCS Pathology, which undertakes half of the cervical screening tests in Victoria, during the same period (unpublished data). As only 57.7% of eligible Victorians participated in screening within the recommended interval during January 2016 – June 2017,8 it is anticipated that the number of participants eligible for self‐collection substantially exceeds the number of self‐collected sample tests performed. This low uptake indicates that the potential of self‐collection to increase screening participation among underscreened women is not being realised.
The limited awareness of self‐collection among screening participants and practitioners has probably contributed to its low uptake in Victoria; most of our participants were unaware of its availability and many practitioners noted lag times between its introduction and their becoming aware of it. Awareness among practitioners is particularly important, as they are currently the drivers of the uptake of self‐collection. Initiatives to promote the pathway and drive demand are critical for ensuring that the potential of self‐collection is realised. Further, difficulties in identifying eligible participants and interpreting guidelines hinder primary care practitioners offering the pathway. Better access in primary care to accurate and timely cervical screening histories could also extend the reach of the pathway. The National Cancer Screening Register and the integration of the Healthcare Provider Portal into practice management software will undoubtedly play critical roles. Finally, clearer clinical practice guidelines that support innovation and flexibility, while maintaining practitioner confidence, will further facilitate uptake of the self‐collection pathway.
Limitations
It was beyond the scope of this study to investigate the experiences and perceptions of self‐collection among women who have not engaged with the pathway. Further, our sample was drawn from Victoria only, rather than nationally. Further, our findings are based on the perceptions and experiences of the small number of screening participants and medical practitioners we interviewed, and they may not have been representative of all screening participants and practitioners. However, our findings provide general insights into the implementation of self‐collection that may be applicable elsewhere.
Conclusion
Our findings provide increased confidence that self‐collection is an acceptable cervical screening pathway that could increase screening participation. Self‐collection, as a feasible and acceptable model of care, will play an important role in further reducing the burden of cervical cancer in Australia. To ensure that the self‐collection pathway can effectively reduce inequities in current programs, major barriers limiting the reach of the pathway that must be overcome include difficulties related to assessing eligibility, low awareness of the pathway among eligible screening participants, and uncertainty about self‐collection among many practitioners.
Box 1 – Demographic characteristics of the 45 interviewed screening participants
|
Category |
Interviewed participants |
All screening participants*† |
|||||||||||||
|
|
|||||||||||||||
|
Age (years) |
|
|
|||||||||||||
|
Under 40 |
12 (27%) |
25% |
|||||||||||||
|
41 or more |
33 (73%) |
75% |
|||||||||||||
|
Location |
|
|
|||||||||||||
|
Metropolitan |
33 (73%) |
71% |
|||||||||||||
|
Rural |
12 (27%) |
29% |
|||||||||||||
|
Ethnic background |
|
|
|||||||||||||
|
European |
39 (87%) |
NA |
|||||||||||||
|
Other |
6 (13%) |
NA |
|||||||||||||
|
Screening history |
|
|
|||||||||||||
|
Overdue |
39 (87%) |
67% |
|||||||||||||
|
Never screened |
6 (13%) |
33% |
|||||||||||||
|
HPV result (self‐collection)† |
|
|
|||||||||||||
|
Negative for HPV |
29 (65%) |
88% |
|||||||||||||
|
Positive for HPV (16/18) |
5 (11%) |
4% |
|||||||||||||
|
Positive for HPV (not 16/18) |
10 (22%) |
7% |
|||||||||||||
|
|
|||||||||||||||
|
HPV = human papillomavirus; NA = not available. * 1067 screening participants who had used the self‐collection cervical screening pathway since the commencement of the renewed National Cervical Screening Program (1 December 2017) in Victoria and 30 April 2019. † Includes only conclusive self‐collection test results; the number of participants who reported receiving inconclusive results was too small to include as separate group. |
|||||||||||||||
Box 2 – Demographic characteristics of the 18 interviewed medical practitioners
|
Category |
Interviewed practitioners |
||||||||||||||
|
|
|||||||||||||||
|
Practitioner type |
|
||||||||||||||
|
General practitioner |
10 (56%) |
||||||||||||||
|
Nurse practitioner or midwife |
8 (44%) |
||||||||||||||
|
Location |
|
||||||||||||||
|
Metropolitan |
10 (56%) |
||||||||||||||
|
Rural |
8 (44%) |
||||||||||||||
|
Primary care setting |
|
||||||||||||||
|
Community health |
5 (28%) |
||||||||||||||
|
Private practice |
5 (28%) |
||||||||||||||
|
General practice |
3 (17%) |
||||||||||||||
|
Aboriginal Controlled Community Health Organisation |
3 (17%) |
||||||||||||||
|
Gender‐diverse |
2 (11%) |
||||||||||||||
|
Self‐collection pathology requests* |
|
||||||||||||||
|
0–6 |
11 (61%) |
||||||||||||||
|
7–12 |
6 (33%) |
||||||||||||||
|
13 or more |
1 (6%) |
||||||||||||||
|
|
|||||||||||||||
|
* During 1 January 2017 – 30 April 2019. |
|||||||||||||||
Box 3 – Reported acceptability of the self‐collection cervical screening pathway from the perspective of screening participants, by HPV test results
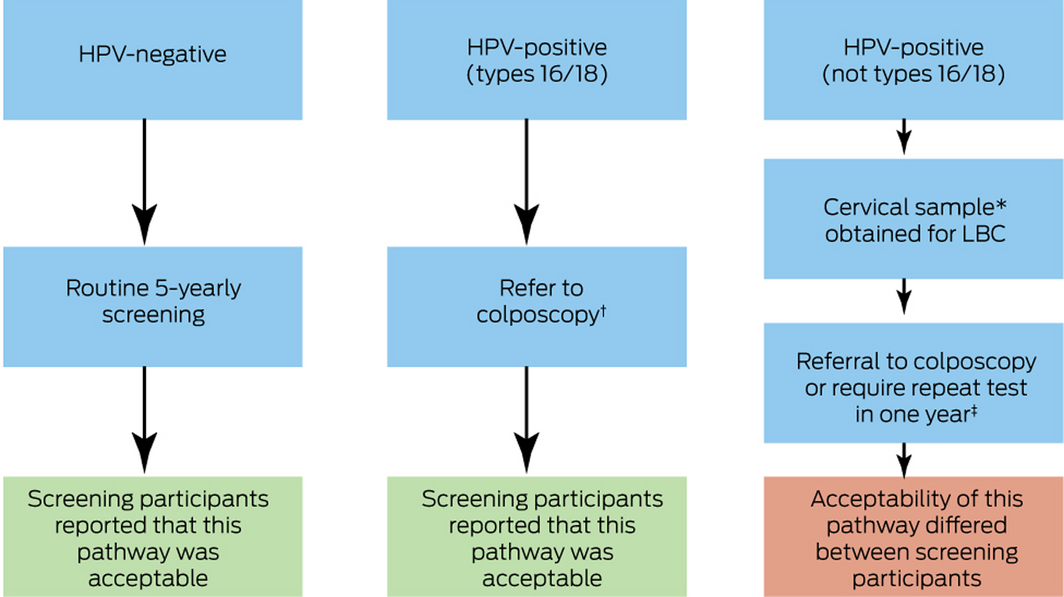
HPV = human papillomavirus; LBC = liquid‐based cytology.
* Clinician‐collected cervical screening test sample that requires an additional health care professional consultation.
† Cervical sample for LBC (clinician‐collected cervical screening test sample) obtained at that visit.
‡ Depending on the LBC result (clinician‐collected cervical screening test sample), screening participants may require a colposcopy or a repeat sample in 12 months.2
This figure is based upon the follow‐up pathway in the clinical practice guidelines.2 The self‐collection pathway clinical practice guidelines can be found in Supporting Information, 4.
Received 25 October 2020, accepted 15 April 2021
- Nicola S Creagh1
- Claire Zammit1,2
- Julia ML Brotherton1,2
- Marion Saville2,3
- Tracey McDermott2
- Claire Nightingale1,4
- Margaret Kelaher1
- 1 Centre for Health Policy, School of Population and Global Health, the University of Melbourne, Melbourne, VIC
- 2 VCS Foundation, Melbourne, VIC
- 3 The University of Melbourne, Melbourne, VIC
- 4 Monash University, Bendigo, VIC
We acknowledge the support of the Victorian Department of Health and Human Services, which funded this study as part of a wider evaluation of the introduction of the self‐collection cervical screening pathway in Victoria. In addition to financial support, the Victorian Department of Health and Human Services provided input regarding methodology, as well as advice and support throughout the project.
We dedicate this article to Professor Margaret Kelaher, who leaves behind an astounding legacy in health equity research and implementation science. She will forever be carried within our hearts and minds, and her memory will guide the future research that we embark upon. Equity in Everything. Vale, Professor Margaret Kelaher.
The VCS Foundation (employer of Julia Brotherton, Marion Saville, Tracey McDermott, Claire Zammit) has received test kits for earlier research without charge from Abbott, BD, Roche, Seegene, and Cepheid. The VCS Foundation has received equipment and a funding contribution for the Compass trial from Roche Molecular Systems and Ventana USA.
- 1. Medical Services Advisory Committee. Application 1276. Final decision: analytic protocol to guide the assessment of the National Cervical Screening Program Renewal. Sept 2012. http://www.msac.gov.au/internet/msac/publishing.nsf/Content/D924E2F768B13C4BCA25801000123B9E/$File/1276-NCSP-FinalDAP.pdf (viewed Mar 2021).
- 2. Canfell K, Saville M, Smith M, et al; Cancer Council Australia Cervical Cancer Screening Guidelines Working Party. Self‐collected vaginal samples (National Cervical Screening Program: guidelines for the management of screen detected abnormalities, screening in specific populations and investigation of abnormal vaginal bleeding). Updated Feb 2021. https://wiki.cancer.org.au/australia/Clinical_question:Self-collected_vaginal_samples (viewed Mar 2021).
- 3. Australian Department of Health. National Cervical Screening Program: self‐collection policy. Apr 2018. https://www.health.gov.au/resources/publications/national-cervical-screening-program-self-collection-policy (viewed Mar 2021).
- 4. Arbyn M, Smith SB, Temin S, et al; Collaboration on Self‐Sampling and HPV Testing. Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: updated meta-analyses. BMJ 2018; 363: k4823.
- 5. Yeh PT, Kennedy CE, de Vuyst H, Narasimhan M. Self‐sampling for human papillomavirus (HPV) testing: a systematic review and meta-analysis. BMJ Glob Health 2019; 4: e001351.
- 6. World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. Nov 2020. https://www.who.int/publications/i/item/9789240014107 (viewed Mar 2021).
- 7. Hall M, Simms K, Smith M, et al. The projected timeframe until cervical cancer elimination in Australia: a modelling study. Lancet Public Health 2019; 4: e19–e27.
- 8. Australian Institute of Health and Welfare. Cervical screening in Australia 2019 (Cat. no. CAN 123; Cancer Series no. 124). Canberra: Australian Institute of Health and Welfare, 2019. https://www.aihw.gov.au/reports/cancer-screening/cervical-screening-in-australia-2019/contents/table-of-contents (viewed Mar 2021).
- 9. Australian Institute of Health and Welfare. Analysis of cervical cancer and abnormality outcomes in an era of cervical screening and HPV vaccination in Australia (Cat. no. CAN 129; Cancer Series no. 126). Canberra: Australian Institute of Health and Welfare, 2019. https://www.aihw.gov.au/getmedia/479cc5bb-d698-4ff7-92fa-4be451b1897b/aihw-can-129.pdf.aspx?inline=true (viewed Mar 2021).
- 10. Sultana F, Mullins R, English DR, et al. Women’s experience with home-based self‐sampling for human papillomavirus testing. BMC Cancer 2015; 15: 849.
- 11. Cadman L, Waller J, Ashdown-Barr L, Szarewski A. Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J Fam Plann Reprod Health Care 2012; 38: 214–220.
- 12. McLachlan E, Anderson S, Hawkes D, et al. Completing the cervical screening pathway: factors that facilitate the increase of self‐collection uptake among under‐screened and never-screened women, an Australian pilot study. Curr Oncol 2018; 25: e17–e26.
- 13. Szarewski A, Cadman L, Mesher D, et al. HPV self‐sampling as an alternative strategy in non-attenders for cervical screening: a randomised controlled trial. Br J Cancer 2011; 104: 915–920.
- 14. Saville M, Hawkes D, Mclachlan E, et al. Self‐collection for under‐screened women in a National Cervical Screening Program: pilot study. Curr Oncol 2018; 25: e27–e32.
- 15. Virtanen A, Nieminen P, Niironen M, et al. Self‐sampling experiences among non-attendees to cervical screening. Gynecol Oncol 2014; 135: 487–494.
- 16. Adcock A, Cram F, Lawton B, et al. Acceptability of self‐taken vaginal HPV sample for cervical screening among an under‐screened Indigenous population. Aust N Z J Obstet and Gynaecol 2019; 59: 301–307.
- 17. Mao C, Kulasingam SL, Whitham HK, et al. Clinician and patient acceptability of self‐collected human papillomavirus testing for cervical cancer screening. J Womens Health (Larchmt) 2017; 26: 609–615.
- 18. Katz ML, Zimmermann BJ, Moore D, et al. Perspectives from health-care providers and women about completing human papillomavirus (HPV) self‐testing at home. Women Health 2017; 57: 1161–1177.
- 19. Brooks J, McCluskey S, Turley E, King N. The utility of template analysis in qualitative psychology research. qualitative research in psychology. Qual Res Psychol 2015; 12: 202–222.





Abstract
Objectives: To evaluate the implementation and acceptability of the self‐collection cervical screening pathway since commencement of the renewed National Cervical Screening Program (rNCSP), from the perspectives of screening participants and primary care practitioners.
Design, setting, participants: Qualitative study; individual semi‐structured interviews with 45 screening participants and 18 primary care practitioners in Victoria who had engaged with the self‐collection pathway during the first 17 months of the rNCSP (1 December 2017 ‒ 30 April 2019).
Results: The self‐collection pathway was highly acceptable as an alternative cervical screening pathway for most participating screening participants and practitioners. Some screening participants indicated that they would not have been screened had the pathway not been available. Acceptability was lower among those who had tested positive for HPV types not 16/18, a result that requires additional testing of a clinician‐collected cervical sample. Use of the self‐collection pathway is driven more by practitioners than their patients. Interpretations of the self‐collection guidelines varied between practices. Barriers to expanding promotion of the pathway by practitioners included difficulties with identifying eligible participants.
Conclusions: Increasing the accessibility of the self‐collection pathway to under‐ and never screened women could reduce inequities in cervical cancer outcomes for those not participating in the main screening pathway. Practitioners should be provided resources to integrate self‐collection into routine practice and to efficiently implement the entire self‐collection pathway, in order to maximise its use and to optimise the experience for screening participants.