In Australia, highly effective direct‐acting antiviral (DAA) therapy has been available for people with chronic hepatitis C through the Pharmaceutical Benefits Scheme (PBS) since March 2016. All clinicians, including general practitioners, have prescribing authority.1 In many countries, DAA prescribing is restricted to specific medical specialties,2 creating barriers to treatment by disrupting the cascade of care and limiting access for those unable or unwilling to attend specialist services.3 In this study, we characterised DAA prescribing by GPs in the Australian model of DAA access.
We analysed PBS data for DAA dispensed to people with chronic hepatitis C during March 2016 – March 2020, applying methodology we have previously described.4 Prescribers were categorised into three broad groups: GPs, main specialist groups, and other prescribers. Main specialist groups included mainstream specialists who provide clinical care to people with or at risk of hepatitis C (gastroenterologists, infectious disease physicians, sexual health specialists, addiction specialists and psychiatrists, internal medicine specialists). We assessed the numbers of people with hepatitis C commencing DAA treatment (aggregated as quarterly numbers and proportions) and DAA prescribers, by prescriber specialty. We also assessed the number of people with hepatitis C prescribed DAA treatment by each prescriber. The UNSW Human Research Ethics Advisory Panel Ethics approved the study (HC200728).
During March 2016 – March 2020, 82 694 people with hepatitis C received DAA treatment, prescribed by GPs in 36 098 cases (44%), by specialists in 42 585 cases (51%), and by other prescribers in 4011 cases (5%) (Box 1). The median age of patients treated by specialists (51 years; interquartile range [IQR], 41–58 years) was slightly higher than for those treated by GPs (46 years; IQR, 37–55 years). Long duration treatment (16–24 weeks), prescribed for patients with more complex disease (eg, cirrhosis, previous failed hepatitis C treatment), was prescribed less frequently by GPs (2188 patients; 6%) than by specialists (5822 patients; 14%; Supporting Information, table).
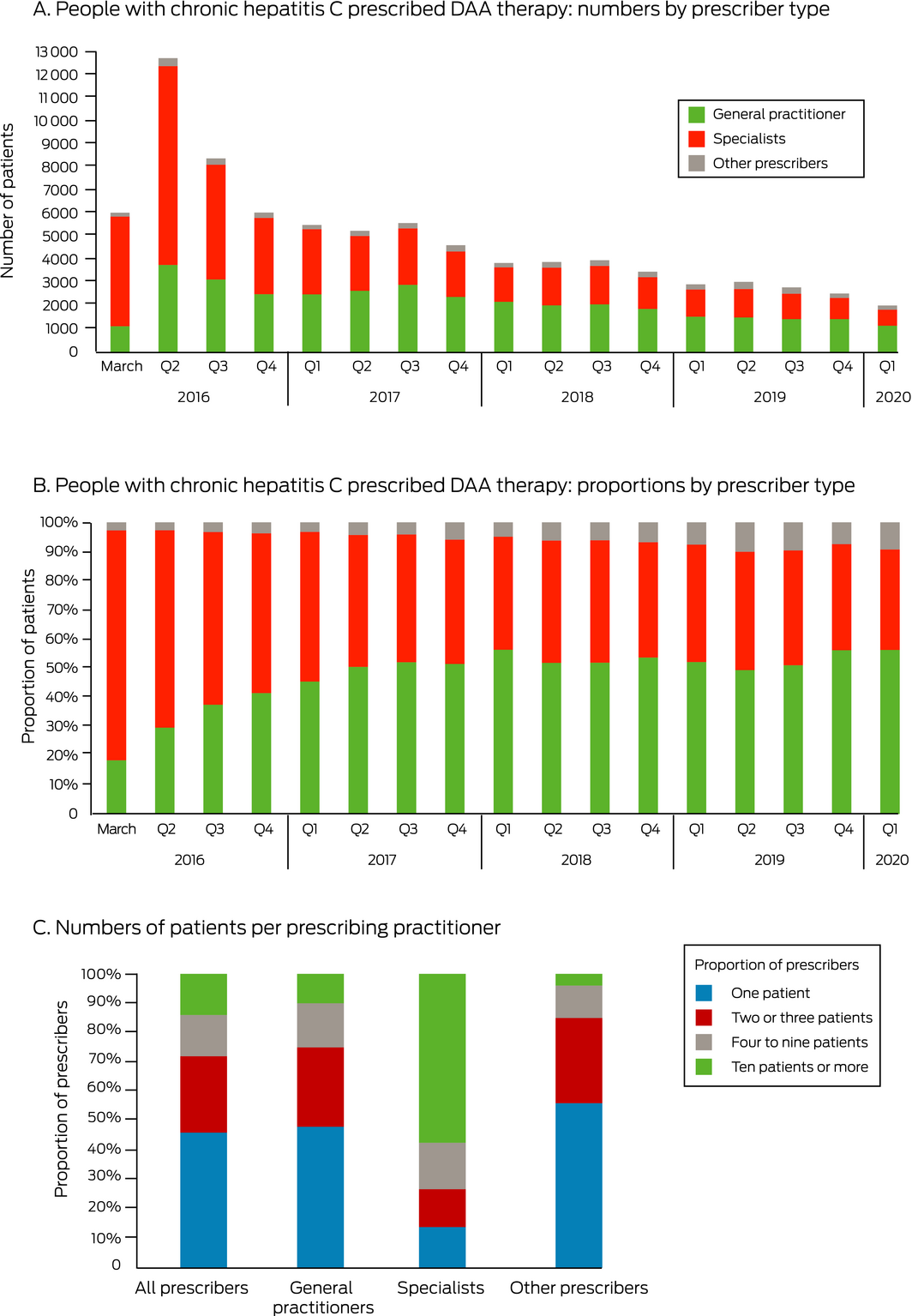
The number of people receiving DAA therapy declined from 33 203 during March–December 2016 to 20 971 in 2017, 15 209 in 2018, and 11 295 in 2019 (Box 2, A). The number of people for whom GPs prescribed DAA treatment declined from 10 531 during March–December 2016 to 5872 in 2019 (44% decrease); the number for whom specialists prescribed treatment declined from 21 662 to 4436 (80% decrease). The proportion of people receiving DAA therapy for whom GPs prescribed treatment increased from 18% (1113 of 6035) in March 2016 to 56% (2172 of 3855) in January–March 2018, and has since remained at about 50% (Box 2, B).
A total of 6187 GPs prescribed DAA treatment for at least one patient (18% of 33 556 registered GPs in 20195). The number of GPs who prescribed DAA as new prescribers was 1863 in 2017 (83% of new prescribers), 1282 in 2018 (78%), and 943 in 2019 (71%) (Supporting Information, figure). Almost half the prescribing GPs (48%, 2986 of 6187) and 14% of prescribing specialists (112 of 811) had prescribed DAA therapy for one patient only; 10% of GP prescribers (630 of 6187) and 58% of specialist prescribers (469 of 811) had treated ten or more patients (Box 2, C). The proportion of GPs treating ten or more patients was slightly higher in urban (12%, 420 of 3573 prescribers) than in regional areas (8%, 207 of 2584).
We found that the broad DAA prescribing authority in Australia has enabled a large number of GPs to contribute to DAA prescribing, important for health policies in settings with restricted access to therapy. The continuing increase in the number of GPs prescribing DAA and the number treating single patients suggest that GPs are gaining confidence in prescribing DAA therapy. This is an important foundation for further enhancing access to treatment.
Box 1 – People with chronic hepatitis C who commenced direct‐acting antiviral (DAA) therapy, and unique prescribers who prescribed DAA therapy, March 2016 – March 2020, by prescriber specialty
|
Prescriber specialty |
Patients commencing DAA therapy |
Prescribers prescribing DAA therapy |
|||||||||||||
|
|
|||||||||||||||
|
All prescribers |
82 694 |
8208 |
|||||||||||||
|
General practitioners |
36 098 (44%) |
6187 (75%) |
|||||||||||||
|
Specialists |
42 585 (51%) |
811 (10%) |
|||||||||||||
|
Gastroenterologists |
30 132 (36%) |
480 (6%) |
|||||||||||||
|
Infectious disease physicians |
5131 (6%) |
118 (1%) |
|||||||||||||
|
Sexual health specialists |
888 (1%) |
32 (< 1%) |
|||||||||||||
|
Addiction specialists and psychiatrists |
836 (1%) |
68 (< 1%) |
|||||||||||||
|
Internal medicine specialists |
5598 (7%) |
113 (1%) |
|||||||||||||
|
Other prescribers |
4011 (5%) |
1210 (15%) |
|||||||||||||
|
Other medical specialists/trainees |
2989 (4%) |
966* (12%) |
|||||||||||||
|
Nurse practitioners |
443 (< 1%) |
28 (< 1%) |
|||||||||||||
|
Unknown |
579 (< 1%) |
216 (3%) |
|||||||||||||
|
|
|||||||||||||||
|
* Other specialists, 94; medical trainees (registrars), 872. |
|||||||||||||||
Received 22 June 2020, accepted 13 November 2020
- 1. Hajarizadeh B, Grebely J, Matthews GV, et al. Uptake of direct‐acting antiviral treatment for chronic hepatitis C in Australia. J Viral Hepat 2018; 25: 640–648.
- 2. Marshall AD, Cunningham EB, Nielsen S, et al; International Network on Hepatitis in Substance Users (INHSU). Restrictions for reimbursement of interferon‐free direct‐acting antiviral drugs for HCV infection in Europe. Lancet Gastroenterol Hepatol 2018; 3: 125–133.
- 3. Radley A, Robinson E, Aspinall EJ, et al. A systematic review and meta‐analysis of community and primary‐care‐based hepatitis C testing and treatment services that employ direct acting antiviral drug treatments. BMC Health Serv Res 2019; 19: 765.
- 4. Iranpour N, Dore GJ, Martinello M, et al. Estimated uptake of hepatitis C direct‐acting antiviral treatment among individuals with HIV co‐infection in Australia: a retrospective cohort study. Sex Health 2020; 17: 223–230.
- 5. Australian Department of Health. General practice workforce providing primary care services in Australia. Updated 17 June 2020. https://hwd.health.gov.au/resources/data/gp‐primarycare.html (viewed June 2021).





The Kirby Institute is funded by the Australian Department of Health and Ageing. Gregory Dore, Gail Matthews and Marianne Martinello were supported by National Health and Medical Research Council (NHMRC) fellowships. Jason Grebely was supported by an NHMRC Investigator grant.
Gregory Dore is a consultant/advisor and has received research grants from Gilead, AbbVie, Merck, Bristol‐Myers Squibb, and Cepheid. Jason Grebely is a consultant/advisor and has received research grants from Gilead, AbbVie, Hologic, Indivior, Merck, and Cepheid. Gail Matthews has received research funding, advisory board payments, and speaker payments from Gilead, and research funding and speaker payments from Janssen.