Suturing, a fundamental skill for surgeons, emergency medicine specialists, and general practitioners, is taught in medical school and throughout surgical training. Opportunities to practise and perfect suturing are limited by the ethical dilemma of learning on patients, and limited access to appropriate synthetic or animal skins. These barriers were highlighted in a 2016 national survey of undergraduate suturing training in the United Kingdom: 526 of 705 students from sixteen medical schools (86%) reported inadequate training. More worryingly, 366 students (44%) reported they did not meet the General Medical Council competency standard for a simple interrupted suture, and 609 (84%) the standard for subcutaneous sutures.1 The authors reported that 20% of medical students paid for supplementary suturing training. The teaching of suturing evidently needs to be improved. We propose that this aim could be accomplished were less expensive, more accessible, and equivalent substitutes to animal and synthetic skins available.
Fruit skins (peels) have been proposed as alternatives to cadaver animal or synthetic skins for suturing practice,2,3,4,5 but few studies have compared suturing of fruit skins and synthetic and animal skins with suturing of human skin. One study compared suturing fruit peels and foam blocks.2 Moreover, studies of suturing alternatives to human skin reported changes in suturing proficiency, but not how accurately these materials simulated the experience of suturing human skin.2,6 Different suturing types (simple, vertical mattress, subcuticular) on different practice materials have not been compared in published studies.
We therefore explored how suturing orange and banana peels, synthetic skin, and pig skin compared with the experience of suturing human skin. We undertook both quantitative (suture completion) and qualitative comparisons (questionnaire).
Methods
Emergency medicine and surgical consultants, general practitioners, and accredited trainees at the Wagga Wagga regional teaching hospital were invited by email during 12 September 2020 – 15 March 2021 to participate in our interventional study. People were contacted if they had completed or were undertaking an accredited surgical, emergency, or general practice training program and had been suturing human skin at least twice a week in the operating theatre or emergency department for at least one year.
Setting and experimental protocol
Doctors who consented to participation were invited to the University of New South Wales clinical school in Wagga Wagga to suture four materials (oranges, bananas, and pig and synthetic skins) using three different suture types (simple interrupted, vertical mattress, subcuticular). Participants sutured the materials in the order: orange, banana, pig, and synthetic skins (Box 1). For each material, simple interrupted sutures were attempted first, then vertical mattress and subcuticular sutures.
Materials
Cavendish bananas (Musa acuminata cultivar) and navel oranges (Citrus × sinensis variety) were obtained from the same supermarket on the day prior to each session. Oranges were selected if their skins exhibited no discolouration or lacerations. Bananas were selected if they had no lacerations and their colour was ranked 3.0–4.0 on a visual ripeness chart;7 we had previously established that banana peels of this colour range were the least likely to resist suturing attempts.
Skin from a frozen, large white pig (Sus scrofa domesticus) was obtained from the same meat supplier one day prior to each session and defrosted overnight. The pig skin was derived from a variety of anatomic locations, including the backstrap, legs, and shoulders.
For synthetic skin we used a 17 cm × 13 cm silicone‐based suture practice pad (Dental Point: suture pad 01), comprising three layers that simulate skin, fat, and muscle.
Preparation of materials
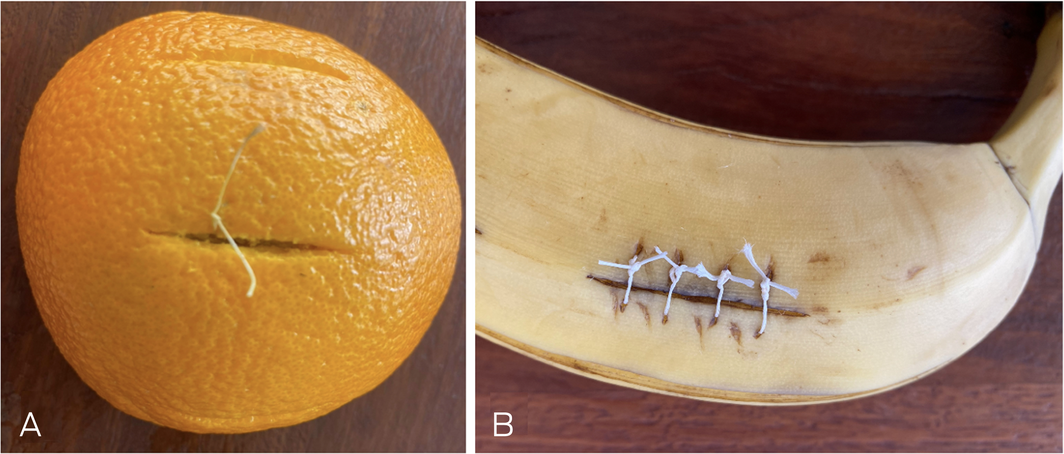
Three 30 mm longitudinal cuts were made into the banana and orange peels and pig skin; the depth of each cut was 5 mm (measured with a marking on the scalpel during cutting, and verified with a ruler). Each cut was widened to an ellipsoid, the opposing edges separated by 4 mm at the centre.
Oranges were cut in half; to optimise orange skin tension, two 30 mm cuts were made along the edges of each half, allowing increased apposition of the edges for suturing (Box 2, A). The three simulated wounds were then cut 20 mm apart, with the central cut on the apex of the half orange (Box 2, B).
For bananas, additional cuts were made to optimise skin tension. We found that a 10 mm cut adjacent to the stalk and cuts along alternative ridges resulted in higher suture completion rates (Box 2, C). The simulated wounds were then cut on the remaining ridge (Box 2, D).
Simulated wounds were cut into the pig skin at least 20 mm apart (Box 2, E). For synthetic skin, we used the 30 mm pre‐made cuts (Box 2, F).
Suturing
Participants chose 2‐0 or 3‐0 monocryl or vicryl sutures, according to personal preference. Simple interrupted, vertical mattress, and subcuticular sutures (Box 3) were performed until the participant was satisfied with wound closure.
Primary outcome
The investigators assessed visually whether a suture had adequately closed the “wound” (the primary outcome). Suture completion was determined visually by the investigators. A suture was deemed complete if it brought the edges to apposition and did not pull through to the wound or another suture hole (Box 4).
Secondary outcomes (questionnaire)
Participants completed a questionnaire that assessed (using Likert scales) how similar suturing the material was to suturing human skin (eg, with regard to bites, pulling, tying), and whether they would recommend the material for practising a particular suture technique. The questionnaire also included a free text question on whether the material resembled human skin from specific anatomic regions (eg, abdomen, hand) (online Supporting Information 1).
We undertook a pilot study to validate the questionnaire, evaluating the responses from ten participants about suturing synthetic skin. Responses regarding similarity to human skin and clinician recommendation for suturing practice were reliable (Cronbach alpha = 0.893). Principal factor analysis identified two factors with eigenvalues greater than one; each questionnaire question contributed to these factors with a commonality score of 0.7 or greater. Analysis of factor loadings indicated that questions regarding recommendation for suturing practice were associated with the first factor (r > 0.8) and those regarding the similarity of the material to human skin with the second factor (r > 0.8). We concluded that the questionnaire adequately assessed both questions.
Statistical analysis
We calculated that 21 participants were required to detect a 35% difference in suture completion rate (α = 0.05; power, 80%); recruitment ceased when this number was reached. The statistical significance of differences between completion rates were assessed in Cochran Q tests, followed by post hoc McNemar tests with Bonferroni corrections. The statistical significance of secondary outcomes were assessed in Kruskal–Wallis tests with post hoc paired comparisons. P < 0.05 was deemed statistically significant. All data analyses were performed in SPSS 26 (IBM).
Ethics approval
The Greater Western Human Research Ethics Committee approved the study (2020/ETH01606), and we adhered to all tenets of the Declaration of Helsinki. Participants provided informed written consent before participation.
Results
Of 32 invited doctors who met the inclusion criteria, 21 participated in the study (15 consultants, six trainees); twelve were men, nine were women.
Primary outcome: suture completion
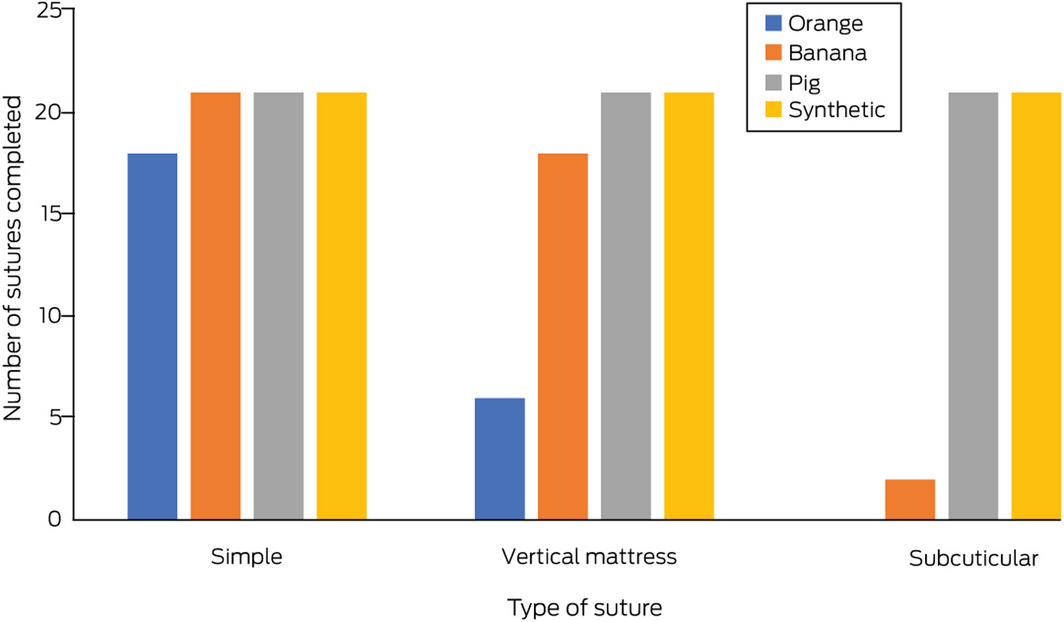
All 21 participants completed simple interrupted sutures in bananas and pig and synthetic skins; 15 completed simple interrupted sutures in oranges (Q test: P = 0.002). All 21 participants completed vertical mattress sutures in pig and synthetic skins, 18 in bananas, and six in oranges (P < 0.001). The numbers of subcuticular suture completions were lower for fruit peels (orange, zero; banana, two) than for pig and synthetic skins (each, 21; P < 0.001) (Box 5; online Supporting Information 2 [video]).
Similarity to human skin and recommendation for suturing practice
For simple interrupted sutures, participants reported that suturing any of the four simulation materials was somewhat similar to suturing human skin. Differences in the material recommended for practising these sutures were not statistically significant.
For vertical mattress sutures, orange skin was generally rated as dissimilar to human skin, while the other three materials were rated as somewhat similar (P = 0.003). Participants would generally not recommend orange skin for practising vertical mattress sutures, would recommend synthetic skin, and were unsure about bananas and pig skin (P = 0.004).
For subcuticular sutures, participants generally rated pig and synthetic skins as somewhat like human skin, but were unsure about recommending them for practice; suturing oranges and bananas was rated as dissimilar or very dissimilar, and were not recommended for practising (Box 6).
Qualitative data
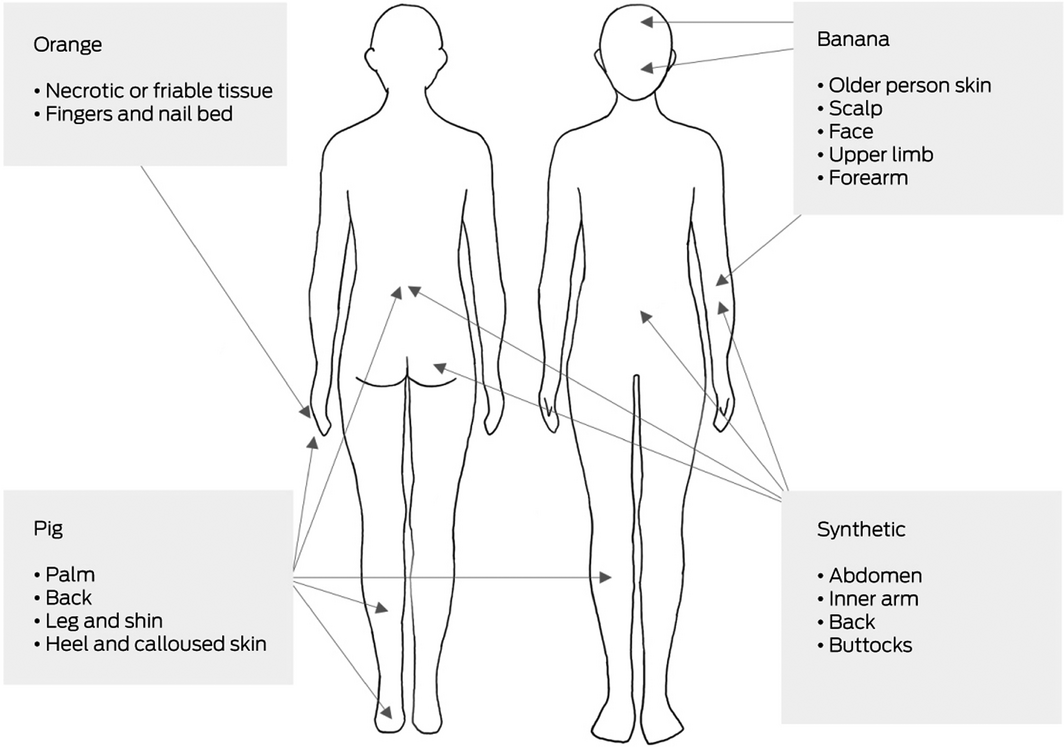
We noted several consistent responses to the question “Is there a specific area of [human] skin that suturing this material simulates?” Orange skin was reported to resemble necrotic friable tissue and very soft tissues, such as nailbed. Banana peel was thought to resemble the skin of older people and soft tissues, such as forearm and facial skin. Pig skin was considered similar to areas of thick skin, such as the palm, soles of the feet, and back. Synthetic skin resembled skin of the torso, including the buttocks, abdomen, and back (Box 7).
Discussion
This is the first study to compare the suitability of non‐traditional materials for practising simple interrupted, vertical mattress, and subcuticular suturing techniques. Surgeons and surgical trainees were asked to compare the similarity of suturing bananas and oranges with suturing human skin, and their suitability for training, with those of traditionally used synthetic and pig skins. All four materials were suitable for practising simple interrupted sutures, but reliability of wound closure was lower with oranges. Attempting vertical mattress sutures on oranges was largely unsuccessful, and subcutaneous suturing was completely unsuccessful. Banana peel was compared with forearm or fragile skin, while orange skin was regarded as similar only to friable or necrotic tissue and finger and nailbed skin.
This was the first study of suturing practice on alternative materials that included only participants who regularly suture in clinical practice. Their collective experience made it possible to confidently establish whether three different suturing techniques were feasible on each material, and whether they accurately simulated human skin. It was also the first study to compare fruit skins with synthetic and pig skins, traditionally used for suturing practice. Our findings indicate that practice materials must be chosen according to suture type: bananas for simple and vertical mattress, oranges for simple interrupted sutures. Reliable practising of subcutaneous suturing was possible only with pig or synthetic skin, but two participants completed subcutaneous sutures on bananas and four vertical mattress sutures on oranges. These lows success rates may be useful as providing a technical challenge for trainees.
Four other published studies have assessed non‐traditional materials for suturing practice. In the most ambitious, a randomised crossover controlled trial, twenty medical students sutured bananas and homemade foam boards. The authors found that banana peel was superior to the foam boards, but the participants had no suturing experience apart from watching a video on suturing technique.2 The similarity of suturing fruit, pig, or synthetic skins to suturing human skin has not been examined in a published study, nor the anatomic areas that these materials most resemble. Our findings are consequently novel, and their credibility bolstered by including participants with surgical experience using three different suturing techniques. We also detail which sections of the body the fruit, pig, and synthetic skins best simulate.
Consistent with the finding of a 2008 study, “Teach yourself to suture for under a tenner”,4 we concluded that bananas provide an economical, accessible, and tasteful material for practising suturing techniques and is acceptable for simulating human skin. However, our major conclusion is that any clinician wanting to improve their suturing techniques should practise on a variety of materials. For example, banana was not as good for practising subcutaneous suturing as synthetic or pig skins. Other materials that emulate human skin for subcutaneous suturing should be explored.
Limitations
Several sets of pig skin and fruit peels were needed, and material quality may have varied between sessions. We attempted to mitigate this problem by sourcing skins from the same location, one day prior to suturing, and by selecting similar mature fruit. Findings using other fruit cultivars or pig species may yield different results. We could not blind participants to the material that they sutured, nor could we control for previous experience with suturing a particular material; several participants reminisced about suturing chicken skin or mangoes. We minimised this effect by enrolling surgeons from various specialties and stages of training. Finally, we did not compare the biomechanical characteristics of the materials and human skin, nor did we measure forces used for suture insertion or tying knots.
Conclusion
Medical students and surgical trainees should have bananas between theatre cases not only for nutritional reasons, but also to practise and improve their simple and vertical mattress sutures. However, less portable and nourishing materials are required to practise subcuticular suturing, such as pig and synthetic skin. An apple a day may keep doctors away, but we contend that suturing a banana a day can keep wound dehiscence away.
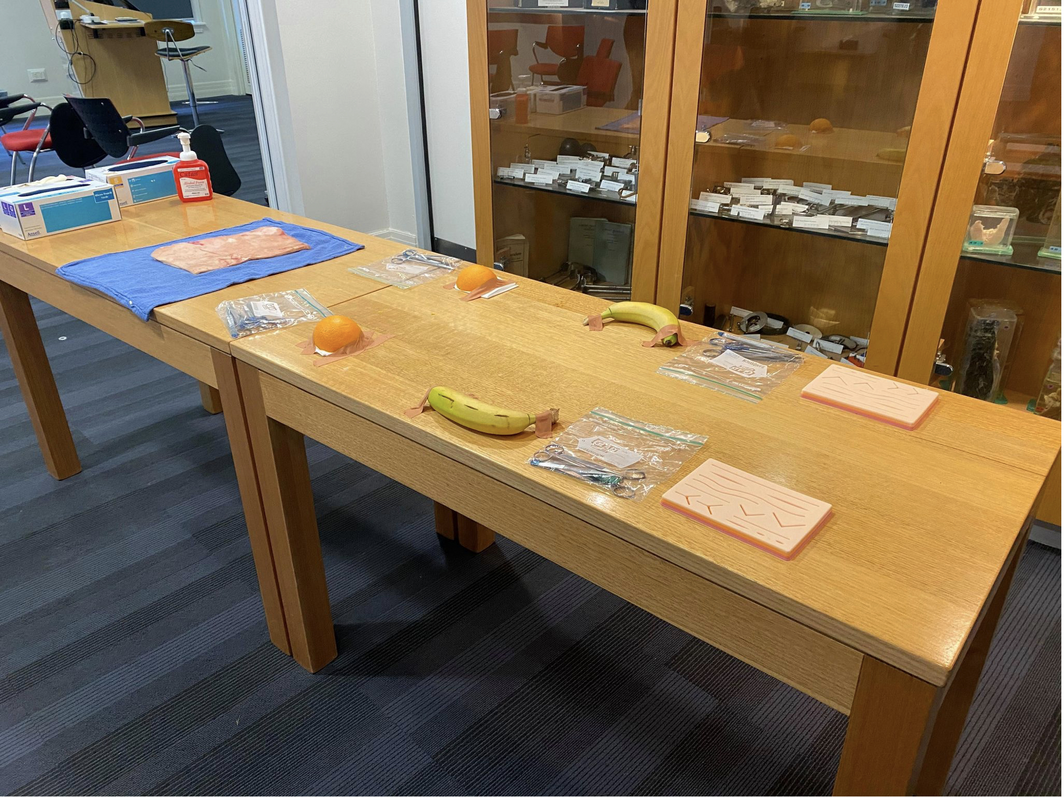
Box 1 – Experimental set‐up. From left to right: pig, orange, banana, and synthetic skins for suturing
Box 2 – Preparation of orange (A, B) and banana (C, D) peels, and pig (E) and synthetic skins (F) for suturing practice

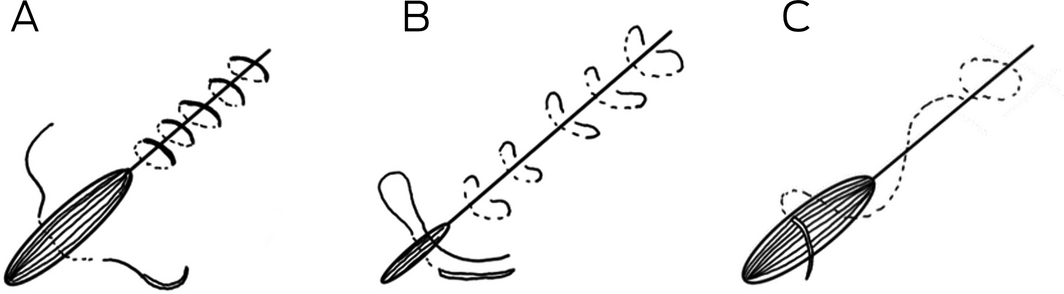
Box 3 – Suture techniques: simple interrupted (A), vertical mattress (B), and subcuticular sutures (C)
Box 6 – Material assessment by participants: similarity to human skin and recommendations for practice
|
Type of suture/assessment: median (IQR)* |
Orange |
Banana |
Pig |
Synthetic |
P |
||||||||||
|
|
|||||||||||||||
|
Simple |
|
|
|
|
|
||||||||||
|
Similarity |
2 (1–2) |
2 (2–3) |
2 (1–3) |
3 (2–3) |
0.05 |
||||||||||
|
Recommend for practice |
3 (1–3) |
3 (3‒3) |
3 (1–3) |
3 (3‒3) |
0.40 |
||||||||||
|
Vertical mattress |
|
|
|
|
|
||||||||||
|
Similarity |
1 (0–2) |
2 (1–3) |
2 (1–3) |
2 (2–3) |
0.003 |
||||||||||
|
Recommend for practice |
1 (0–2) |
3 (1–3) |
3 (1–3) |
3 (3‒3) |
0.004 |
||||||||||
|
Subcuticular |
|
|
|
|
|
||||||||||
|
Similarity |
0 (0‒0) |
0 (0‒1) |
2 (1–3) |
2 (1–3) |
< 0.001 |
||||||||||
|
Recommend for practice |
0 (0‒0) |
0 (0‒1) |
3 (1–3) |
3 (2–3) |
< 0.001 |
||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range. * Five‐point Likert scale (0‒4). |
|||||||||||||||
- Geoffrey Murphy1
- Muhammad A Khan1
- Adil Lathif1
- John Preddy2,3
- 1 University of New South Wales, Sydney, NSW
- 2 Rural Clinical School, University of New South Wales, Wagga Wagga, NSW
- 3 Wagga Wagga Base Hospital, Wagga Wagga, NSW
No relevant disclosures.
Received 14 June 2021, accepted 29 September 2021
- 1. Rufai SR, Holland LC, Dimovska EO, et al. A national survey of undergraduate suture and local anesthetic training in the United Kingdom. J Surg Educ 2016; 73: 181–184.
- 2. Wong K, Bhama PK, d’Amour Mazimpaka J, et al. Banana fruit: an “appealing” alternative for practicing suture techniques in resource‐limited settings. Am J Otolaryngol 2018; 39: 582–584.
- 3. Ohn MH, Ohn KM, Souza UD, et al. Banana peel: is it useful for surgical suturing training? J Phys Conf Ser 2019; 1358: 012018.
- 4. Varley I, Duncan T. Teach yourself to suture for under a tenner. BMJ 2006; 332: 060254.
- 5. Kumaresan R, Karthikeyan P. An inexpensive suturing training model. J Maxillofac Oral Surg 2014; 13: 609–611.
- 6. Gallagher PO, Bishop N, Dubrowski A. Investigating the perceived efficacy of a silicone suturing task trainer using input from novice medical trainees. Cureus 2020; 12: e6612.
- 7. Ji W, Koutsidis G, Luo R, et al. A digital imaging method for measuring banana ripeness. Color Res Appl 2013; 38: 364–374.





Abstract
Objectives: To investigate how suturing orange and banana peels, pig skin, and synthetic skin compares with the experience of suturing human skin.
Design: Interventional study of simple interrupted, vertical mattress, and subcuticular suturing on the four test materials.
Participants, setting: Fifteen consultants and six trainees in surgical and emergency medicine specialties at a New South Wales regional teaching hospital.
Main outcome measures: The primary outcome was completion of simple interrupted, vertical mattress, and subcutaneous sutures. Secondary outcomes (assessed in a questionnaire) were similarity of suturing each material to suturing human skin, suitability of each material for practising each suture type, and similarity of each material to human anatomic skin types.
Results: All 21 participants completed simple interrupted sutures in bananas and pig and synthetic skins, and 15 in orange skin (P = 0.002). All 21 participants completed vertical mattress sutures in pig and synthetic skins, 18 in bananas, and six in oranges (P < 0.001). The numbers of completed subcuticular sutures were lower for the two fruits (orange, zero; banana, two) than for pig and synthetic skins (each, 21; P < 0.001). Banana peel was rated as somewhat similar to human skin and recommended for practising simple interrupted and vertical mattress suturing.
Conclusions: Bananas are not only useful as healthy snacks between theatre cases, but also for practising and improving simple and vertical mattress suturing skills. However, less portable and nourishing materials are required for subcuticular suturing practice, such as pig skin or synthetic skin.