Practitioners who prescribe opioid medications for people with chronic non‐cancer pain must navigate increasingly stringent policy requirements,1 research findings questioning the benefit of opioids for such patients,2 and patients who fear uncontrolled pain if opioids are withdrawn.3
In Australia and New Zealand, people with chronic non‐cancer pain may be referred to specialist pain management services, most of which participate in the electronic Persistent Pain Outcomes Collaboration (ePPOC; https://www.uow.edu.au/ahsri/eppoc), an initiative for collecting standardised information about their patients, the services they provide, and the outcomes of treatment. This information is used at point of care, and for reporting, benchmarking, and research.
To explore the impact of changes in opioid use on outcomes for patients, we analysed ePPOC data collected at 67 pain services (online Supporting Information) during January 2015 – June 2020. We extracted data for all patients with completed episodes of care and who had answered questions about opioid use at referral and episode end. We summarised their characteristics and outcomes as means with standard deviations (SDs). All analyses were conducted in SAS 9.4. Our study was approved by the University of Wollongong and Illawarra and Shoalhaven Local Health District health and medical human research ethics committee; reference, 2019/ETH03804).
The mean age of the 10 302 patients who provided information at both referral and at the end of their treatment episodes was 49.5 years (SD, 14.4 years); 5807 were women (56.4%), and 3490 had experienced their pain for more than five years (33.9%). The most frequent site of their main pain was the back (3936 patients; 38.2%).
A total of 6340 patients (61.5%) were using opioid medications at referral (Box 1); their mean oral morphine equivalent daily dose4 was 56.3 mg (SD, 75.3 mg), the median daily dose was 31.0 mg (interquartile range [IQR], 15–75 mg). They reported higher mean pain scores than patients not using opioids at referral (6.2 [SD, 1.6] v 5.8 [SD, 1.7]) and greater interference in daily activities (7.2 [SD, 1.8] v 6.5 [SD, 2.0]; each measured with the Brief Pain Inventory5). Mean values for depression, anxiety, stress, pain catastrophising, and pain self‐efficacy were also worse for people using opioid medications (data not shown).
The most frequent service events were individual appointments with medical and allied health staff (35 678 of 55 012 events, 65%) and group pain programs (18 841 events, 34%); there were 493 procedural interventions (1%). The median episode length was 175 days (IQR, 99–322 days).
Opioid prescribing varies between pain services, including direct prescribing by the pain specialist and recommendations to patients’ general practitioners. However, a major focus of multidisciplinary care is supporting patients to reduce their opioid use, which typically involves collaboration between the patient, their GP, and the pain service.
By the end of their treatment episodes, 1724 patients who reported using opioids at referral (27.2%) had stopped doing so, 1234 patients (19.5%) had reduced their dose by at least 50% and 3382 patients (53.3%) had either not changed, increased, or reduced opioid use by less than 50%. For each group, scores had improved in each clinical domain, and the changes were greatest for patients who had ceased opioid use, as were the proportions experiencing clinically significant improvement. Scores for measures specifically related to pain experience (pain severity, interference, catastrophising and self‐efficacy) at the end of treatment were similar to or better than those of patients who had not been using opioids at referral, despite greater initial pain severity. Conversely, the smallest mean improvements were for the patients who had not reduced opioid use by at least 50% (Box 2).
Although our study was limited by its retrospective nature, the lack of follow‐up of patients who did not complete treatment, and its restriction to specialist pain practices, our findings are encouraging. We found that significant clinical improvements are possible for people with chronic non‐cancer pain attending multidisciplinary pain management services in Australia and New Zealand, even as they discontinue opioid medications. The challenge is to extend these services and supported self‐management skills to primary and community care.
Box 1 – Opioid use by patients at referral and at the end of treatment in specialist pain clinics
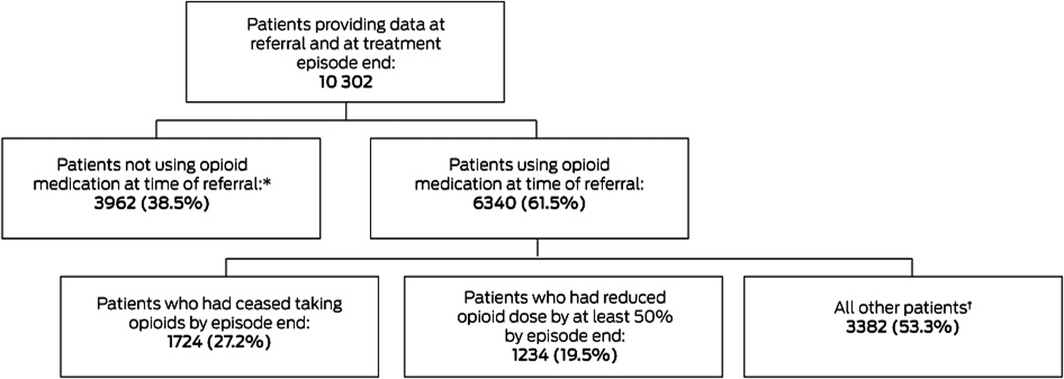
* Opioid therapy was initiated for 536 of patients who had not being using opioid medications at referral (13.5%). † Opioid use had been reduced by less than 50% for 1025 patients (30.3%), not changed for 878 patients (26.0%), and increased for 1479 patients (43.7%).
Box 2 – Mean pain and psychometric scores, and changes in scores between referral and end of treatment (with standard deviations), by opioid use at the two time points
|
Clinical domain |
Patients not using opioids at referral |
Patients who were using opioids at referral |
|||||||||||||
|
Ceased taking opioids |
Reduced opioid use by at least 50% |
Other* |
|||||||||||||
|
|
|||||||||||||||
|
Total number of patients |
3962 |
1724 |
1234 |
3382 |
|||||||||||
|
Pain severity (BPI5) |
3787 |
1646 |
1174 |
3215 |
|||||||||||
|
Referral |
5.8 (1.7) |
6.1 (1.7) |
6.3 (1.6) |
6.3 (1.6) |
|||||||||||
|
Episode end |
4.9 (2.0) |
4.9 (2.0) |
5.5 (1.8) |
5.8 (1.7) |
|||||||||||
|
Change in score |
–0.9 (1.7) |
–1.2 (1.8) |
–0.8 (1.6) |
–0.5 (1.5) |
|||||||||||
|
Clinically significant improvement† |
817/2997 (27%) |
459/1410 (33%) |
231/1035 (22%) |
436/2827 (15%) |
|||||||||||
|
Pain interference (BPI5) |
3905 |
1702 |
1219 |
3316 |
|||||||||||
|
Referral |
6.5 (2.0) |
7.1 (1.8) |
7.3 (1.7) |
7.2 (1.9) |
|||||||||||
|
Episode end |
4.9 (2.4) |
5.0 (2.4) |
5.7 (2.3) |
6.2 (2.2) |
|||||||||||
|
Change in score |
–1.6 (2.2) |
–2.1 (2.3) |
–1.6 (2.1) |
–1.0 (2.0) |
|||||||||||
|
Clinically significant improvement† |
2050/3279 (63%) |
1062/1546 (69%) |
679/1133 (60%) |
1481/3003 (49%) |
|||||||||||
|
Depression (DASS‐216) |
3827 |
1673 |
1201 |
3240 |
|||||||||||
|
Referral |
17.8 (12.1) |
20.2 (12.4) |
20.9 (12.6) |
20.7 (12.4) |
|||||||||||
|
Episode end |
12.8 (11.1) |
13.8 (11.6) |
15.6 (12.0) |
16.6 (11.9) |
|||||||||||
|
Change in score |
–5.0 (10.1) |
–6.4 (11.0) |
–5.3 (10.7) |
–4.0 (10.2) |
|||||||||||
|
Clinically significant improvement† |
1308/2231 (59%) |
662/1100 (60%) |
434/810 (54%) |
1042/2190 (48%) |
|||||||||||
|
Anxiety (DASS‐216) |
3821 |
1676 |
1191 |
3233 |
|||||||||||
|
Referral |
12.1 (10.2) |
13.3 (10.4) |
14.1 (10.4) |
13.7 (10.3) |
|||||||||||
|
Episode end |
10.1 (9.5) |
10.9 (9.7) |
11.9 (9.7) |
12.5 (10.1) |
|||||||||||
|
Change in score |
–2.0 (8.2) |
–2.4 (8.7) |
–2.2 (8.4) |
–1.2 (8.0) |
|||||||||||
|
Clinically significant improvement† |
858/1972 (44%) |
438/962 (46%) |
288/716 (40%) |
662/1904 (35%) |
|||||||||||
|
Stress (DASS‐216) |
3818 |
1660 |
1191 |
3226 |
|||||||||||
|
Referral |
19.8 (11.0) |
21.1 (10.8) |
21.9 (10.9) |
21.2 (11.1) |
|||||||||||
|
Episode end |
15.6 (10.6) |
16.6 (10.7) |
17.9 (10.5) |
18.6 (10.8) |
|||||||||||
|
Change in score |
–4.1 (9.6) |
–4.5 (10.2) |
–4.0 (9.3) |
–2.6 (9.2) |
|||||||||||
|
Clinically significant improvement† |
1154/1936 (60%) |
553/905 (61%) |
387/710 (55%) |
898/1828 (49%) |
|||||||||||
|
Pain catastrophising (PCS7) |
3796 |
1649 |
1174 |
3204 |
|||||||||||
|
Referral |
26.3 (13.3) |
28.1 (13.4) |
28.5 (13.4) |
28.3 (13.3) |
|||||||||||
|
Episode end |
18.3 (13.3) |
17.9 (13.5) |
20.9 (13.6) |
22.1 (13.6) |
|||||||||||
|
Change in score |
–8.0 (11.6) |
–10.2 (12.2) |
–7.6 (11.1) |
–6.2 (11.2) |
|||||||||||
|
Clinically significant improvement† |
1425/2513 (57%) |
714/1164 (61%) |
435/841 (52%) |
1056/2308 (46%) |
|||||||||||
|
Pain self‐efficacy (PSEQ8) |
3860 |
1685 |
1210 |
3262 |
|||||||||||
|
Referral |
24.0 (12.6) |
20.6 (12.0) |
18.6 (11.0) |
18.9 (11.9) |
|||||||||||
|
Episode end |
32.1 (14.4) |
32.0 (14.4) |
26.9 (13.1) |
24.0 (13.1) |
|||||||||||
|
Change in score |
+8.1 (12.7) |
+11.5 (14.0) |
+8.3 (12.7) |
+5.1 (12.1) |
|||||||||||
|
Clinically significant improvement† |
1433/2796 (51%) |
827/1382 (60%) |
504/1058 (48%) |
1015/2773 (37%) |
|||||||||||
|
|
|||||||||||||||
|
BPI = Brief Pain Inventory (range, 0–10); DASS‐21 = Depression Anxiety and Stress Scale (range, 0–42); PCS = Pain Catastrophising Scale (range, 0–52); PSEQ = Pain Self‐Efficacy Questionnaire (range, 0–60; higher scores indicate greater self‐efficacy). * Opioid use by patients had been reduced by less than 50%, not changed, or increased. † For patients who reported at least moderate symptom severity at referral (see Supporting Information for definitions of clinically significant improvement). |
|||||||||||||||
Received 14 September 2020, accepted 5 February 2021





We thank the staff at the participating pain management services for collecting and collating the data we analysed.
The electronic Persistent Pain Outcomes Collaboration (ePPOC) is funded by the participating services, NSW Health, the Victorian Department of Health and Human Services, the Victorian Transport Accident Commission, Worksafe Victoria, the Australian Department of Veterans’ Affairs, and the Accident Compensation Corporation (New Zealand). Hilarie Tardif and Samuel Allingham are employed by ePPOC.