To the Editor: As the coronavirus disease 2019 (COVID‐19) pandemic spread across Europe, we worked in the intensive care unit (ICU) of a Swedish university hospital. We share our experiences and offer some thoughts regarding Sweden’s pandemic response.
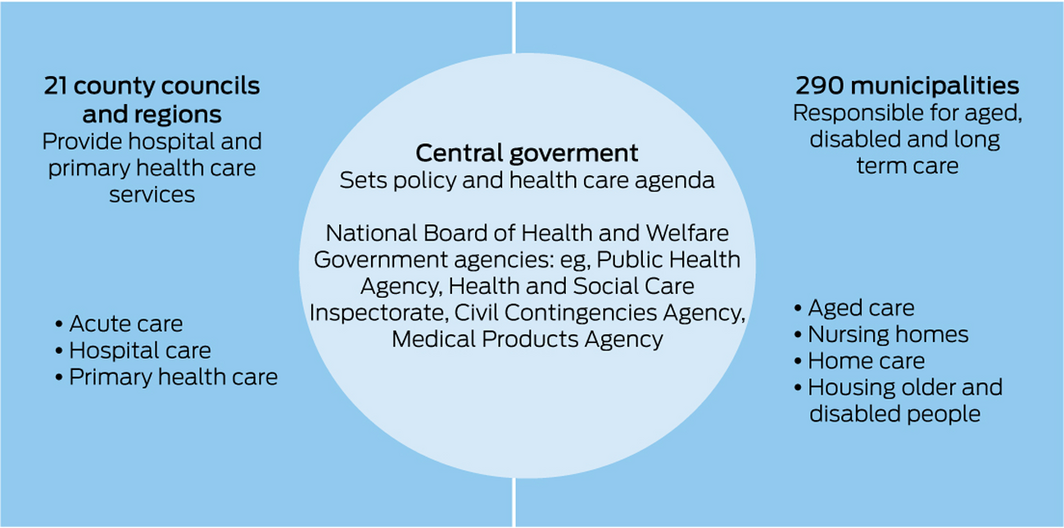
The decentralised Swedish health system works on three levels (Box). These traditional divisions may partially account for the lack of coordination between care services in the initial phases of the pandemic, where large numbers of deaths occurred in care homes. As the pandemic intensified, safety checks were implemented to protect residents of aged care facilities. This resulted in a quick containment of infections, although tragically too late for many.
Our health care region received the fourth highest number of hospitalisations in Sweden.1 We were privileged to work in a system that was well organised, without political conflict and with pre‐existing disaster plans that were quickly converted to pandemic plans. A pandemic‐specific leadership established a centralised inventory and oversaw the acquisition and distribution of beds, staffing, medical equipment, essential drugs, personal protective equipment and disinfection agents. An eight‐step plan ensured a rapid escalation of regional ICU capacity. Intermediate care units were opened, reducing demand for ICU beds. Projected numbers of patients were calculated daily, based on models provided from the Public Health Agency of Sweden and local data.
Anaesthesia and intensive care are a combined speciality in Sweden. This enabled the rapid deployment of a large workforce of anaesthetists and nurse anaesthetists to ICUs. Despite these resources, our tripled ICU capacity meant significant staffing challenges, with additional difficulties because of staff illnesses and quarantines.
Our impression is that the Swedish response has been controlled and planned for the long term. Daily public announcements from the Public Health Agency became a regular part of our lives and Swedes were generally compliant with recommendations regarding physical distancing and hygiene routines. We are perplexed by reports in the media that life went on as usual in Sweden. In fact, life was very different. Most people worked from home, large numbers were furloughed, many institutions were closed and public events were cancelled. Travel was discouraged and fell dramatically.2 What sets the Swedish approach apart from others is that these measures were largely voluntary, with generally good public support.
We avoided an overwhelming wave of patients with an undercapacity of ICU beds, as seen in many other countries. We maintained normal criteria for ICU admissions. This is notable given that Sweden has the second lowest number of ICU beds per capita in Europe.3,4 Results from intensive care are encouraging, with mortality rates generally lower than previously reported.5
Challenges included staff burnout, a shortage of usual sedatives and lack of clinical experience with this new disease, resulting in the use of futile and potentially harmful treatments. However, guidance from a national group of senior clinicians provided regular recommendations6 and there was excellent compliance with advice from regulatory authorities.
Up to 70% of elective surgeries were cancelled during the first half of 2020. Cancer‐related surgeries continued to be prioritised during the pandemic, but the longer term effects of cancelled surgeries, outpatient clinics and altered illness behaviour are not known. We are heartbroken at our inability to provide enough comfort to relatives of our patients who succumbed to COVID‐19 when hospital visits were prohibited.
As two Australian emigrants working in a Swedish ICU, we are humbled by our ability to contribute to the care of patients during the pandemic. Our Australian medical training instilled in us a sense of duty, tempering any feelings of helplessness. We applaud the tenacity of our Swedish colleagues. We wish our Australian colleagues well and hope that Australia will be protected from the horrors of COVID‐19.
- 1. Socialstyrelsen. Statistik om slutenvård av patienter med covid‐19. https://www.Socialstyrelsen.se/statistik-och-data/statistik/statistik-om-covid-19/statistik-om-slutenvard-av-patienter-med-covid-19/ (viewed Oct 2020).
- 2. Telia COVID‐19 mobilitetsanalys: svenskarnas resande: vecka 4. https://www.telia.se/privat/aktuellt/hemma-i-folknatet/covid-19-mobilitetsanalys (viewed Oct 2020).
- 3. Rhodes A, Ferdinande P, Flaatten H, et al. The variability of critical care bed numbers in Europe. Intens Care Med 2012; 38: 1647–1653.
- 4. Swedish Intensive Care Registry. Guideline for Swedish intensive care. https://portal.icuregswe.org/seiva/en/Rapport (viewed Oct 2020).
- 5. Chew MS, Blixt P, Åhman R, et al. National outcomes and characteristics of patients admitted to Swedish intensive care units for COVID‐19: a registry‐based cohort study. Eur J Anaesth 2021; https://doi.org/10.1097/EJA.0000000000001459 [online ahead of print].
- 6. Swedish Society for Anaesthesiology and Intensive Care. COVID‐19/SARS‐CoV2 guidelines. https://sfai.se/riktlinje/medicinska-rad-och-riktlinjer/intensivvard/covid-19-sars-cov-2019/ (viewed Feb 2021).





Michelle Chew has received grants from Linköping University and the Region Östergötland County Council for COVID‐19 research. The funding agency had no role in the planning, writing or publication of this article. We gratefully acknowledge the efforts of our colleagues at the Department of Anaesthesia and Intensive Care, Linköping University, Vrinnevi and Motala Hospitals, for their work during the COVID‐19 pandemic.
No relevant disclosures.