The known: Several demographic, clinical, and social risk factors are associated with suicide by young people, but they have not been investigated on the national scale in Australia.
The new: Among the 3027 young people who died by suicide during 2006–2015, the lifetime burdens of mental health problems (57%), self‐harm (31%), and illicit substance use (28%) were high. Fewer than one‐third were receiving mental health care at the time of their deaths.
The implications: We need to ensure that young people are better engaged with mental health care and receive adequate support for dealing with mental health problems and psychosocial stressors, such as employment and financial difficulties.
Suicide is the leading cause of death of Australians under 25 years of age.1 The annual number of young Australians who died by suicide has nearly doubled over the past decade, from 279 in 2009 to 458 in 2018; 25% of suicide deaths in 2018 were of people under 25, while 15% were of people over 65.1
The suicide rate increases sharply during adolescence, and is as much as ten times as high for people aged 15–29 years as for children aged 5–14 years.2 Adolescence is also the peak period for the onset of mental health disorders, including depression, anxiety, and substance use disorders.3,4 Social stressors such as parental discord,5 abuse and neglect,5 exposure to suicide,6 and rapid changes in emotional and cognitive development,3 are also associated with suicidal behaviour in adolescents.
In Australia, national and state‐based suicide prevention strategies recognise young people as being at particular risk and in need of specific preventive strategies.7 But information on the demographic, social, and clinical antecedents of suicide by young Australians is limited to studies restricted by geographic location8,9 or suicide method,10,11 or studies that included both young people and adults.12 We therefore analysed national suicide mortality data to identify the demographic, social, and clinical characteristics of young Australians who died by suicide during 2006–2015.
Methods
We conducted a retrospective national study of suicide in Australia by people aged 10–24 years during 2006–2015, based upon data from the National Coronial Information System (NCIS). The year 2015 was selected as the study endpoint because more than 90% of intentional self‐harm cases to the end of 2015 had been closed by the time of our analysis.13 Cases were extracted from the NCIS database in April 2017, and we updated our search for closed cases in June 2019.
The NCIS is an online data repository for all external cause deaths in Australia. Individual deaths are recorded as cases comprising a core dataset. Additional information is available as free text documents, including police reports, coroners’ reports, autopsy reports, and post mortem toxicology reports. We included cases in our analysis if the deceased had been aged 10–24 years and died during 1 January 2006 – 31 December 2015, the cause of death was recorded as “intentional self‐harm”, and the case had been closed by the coroner (ie, investigation was complete) (further details: online Supporting Information, part 1.1).
Study variables
We extracted NCIS core data on age, Indigenous status, method of suicide, location of suicide, and remoteness and geospatial information on the location of death. Population level data from the 2011 Index of Relative Socio‐economic Disadvantage (IRSD) was obtained from the Australian Bureau of Statistics.14 The social and clinical antecedents of suicide were collected from police, coroner, autopsy, and toxicology reports. In cases of discrepancies between information in the police and coroner reports, information in the coroner report was deemed final (Supporting Information, table 1).
Statistical analysis
We calculated age‐ and sex‐specific suicide rates (number per 100 000 person‐years). Population estimates were extracted from the Australian Bureau of Statistics annual mid‐year estimated resident population of people aged 10–24 years (2006–2015), using TableBuilder.15 For the free text analysis, antecedents of suicide were coded as categorical variables in an Excel spreadsheet (Microsoft). Data were coded as the presence or absence of the relevant characteristic unless otherwise specified (Supporting Information, table 2). Results for each variable are reported as proportions, overall and by sex. All analyses were conducted in R 3.6.0 (R Foundation for Statistical Computing).
Ethics approval
Our study was approved by the Justice Human Research Ethics Committee (reference, CF/15/13188).
Results
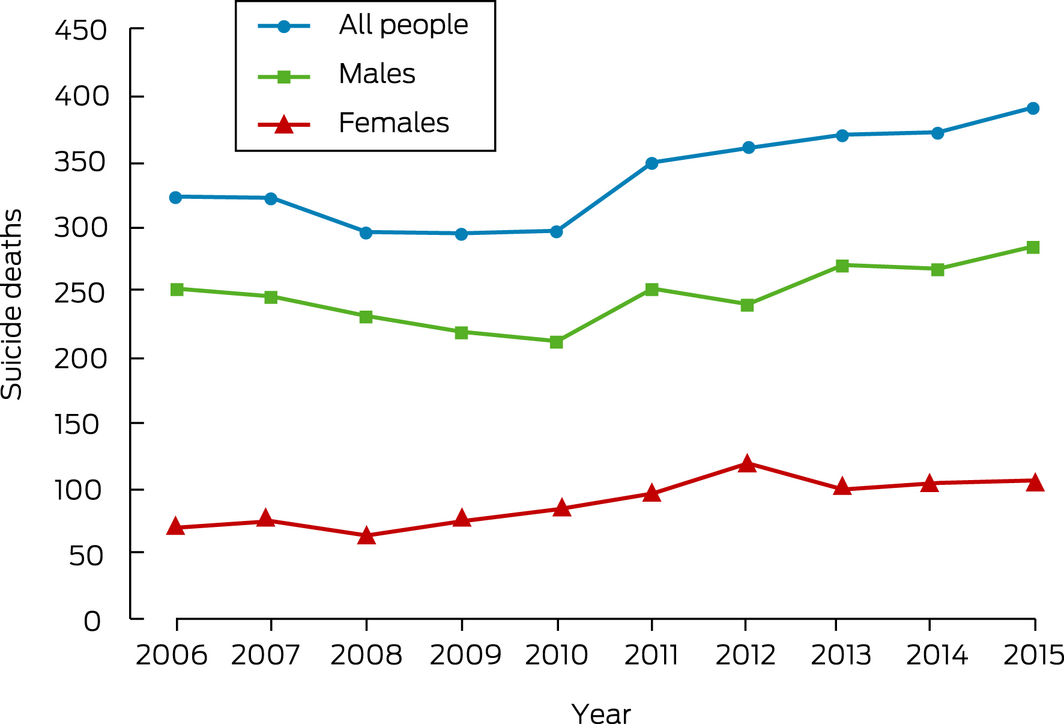
Between 1 January 2006 and 31 December 2015, 3365 people aged 10–24 years died by suicide in Australia (Box 1), a rate of 7.59 per 100 000 people in this age group (males: 10.9 per 100 000; females: 4.1 per 100 000). Annual age‐specific rates were higher for people aged 19–24 years (males, 19.1 per 100 000; females, 5.9 per 100 000) than for those aged 15–19 years (males, 11.6 per 100 000; females, 5.3 per 100 000) or 10–14 years (both sexes, 1.0 per 100 000). Suicide rates among people aged 10–24 years were highest in the Northern Territory (27.4 per 100 000) and Western Australia (10.1 per 100 000), and lowest in the Australian Capital Territory (0.7 per 100 000) (Supporting Information, figures 1–3).
Demographic characteristics and circumstances of death
Most suicides were by boys or men (2473 of 3365, 73.5%); 484 suicides (14.4%) were by Aboriginal or Torres Strait Islander Australians, 255 (7.6%) by people residing in remote or very remote locations, and 1292 (38.4%) by people residing in the most disadvantaged regions in Australia (IRSD deciles 1–3, based on 2011 Statistical Areas 2 category for place of residence).16 Hanging or strangulation (2341 deaths, 69.6%), poisoning by gaseous substances (183, 5.4%), falls from heights (179, 5.3%), and railway suicides (172, 5.1%) were the most frequent methods of suicide; most of the young people took their lives at home (2242 deaths, 66.6%) (Box 2, Supporting Information, figure 4).
Social, clinical and adverse life events characteristics (free text data)
Narrative text was unavailable from both the police and coroners’ reports for 338 of 3365 cases (10.0%), including all 240 cases in South Australia (Supporting Information, part 1.2). Consequently, free text reports for the deaths of 3027 young people (90.0%), including separate toxicology reports for 2996 people, were examined for information on the social and clinical antecedents of their deaths.
At the time of death, 879 of 3027 people (29.0%) were enrolled in education or training, 994 (32.8%) were employed, and 1172 (38.7%) were neither employed nor in education or training. A total of 142 (4.7%) had experienced deaths of parents, and 202 (6.7%) had been exposed to the suicides of relatives, friends, or acquaintances. A history of abuse and neglect was reported in 223 cases (7.4%), and 76 people (2.5%) had been exposed to domestic violence. Contact with child protection services or out‐of‐home placement (including foster care) was reported in 52 cases (1.7%), and 31 young people (1.0%) had had contact with the juvenile justice system (Box 3).
A total of 1237 young people (40.9%) had confirmed mental health disorder diagnoses, and 475 (15.7%) were reported as possibly having mental health disorders. The most commonly recorded diagnosed disorders were depression (902 of 1237 people, 72.9%), anxiety (238, 19.2%), and psychotic disorders (175, 14.1%) (Box 4; Supporting Information, table 4). A history of non‐fatal self‐harm or attempted suicide was reported in 940 cases (31.1%), including for 161 young people (5.3%) in the 12 months preceding their deaths. Suicide notes were left by 815 people (26.9%); 1123 (37.1%) had communicated suicidal thoughts to friends or family members (Box 4).
Illicit substance use was indicated in toxicology, autopsy or coroner reports for 852 of 3027 people (28.1%), and evidence of alcohol consumption near the time of death was noted in 1015 cases (33.5%), including 350 (11.6%) in which the alcohol concentration exceeded 150 mg/dL (the threshold for significant cognitive impairment in adults). Excessive alcohol use or binge drinking was reported for 485 young people (16.0%) (Box 4).
Contact with mental health care services (free text data)
Overall, 496 of 3027 young people (16.4%) had reportedly been admitted to hospital or inpatient care for treatment of mental health symptoms at least once during their lives, and 228 (7.5%) had been discharged from emergency departments after treatment related to mental health symptoms (Box 5). A total of 2210 young people (73.2%) had diagnosed or possible mental health disorders or histories of attempted suicide or illicit substance misuse, or had presented to emergency departments for mental health‐related events.
Of the 1237 young people with diagnosed mental health disorders, 1002 (81.0%) were receiving treatment at the time of death: 521 (52.0%) were receiving psychopharmacological treatment, 359 (35.8%) both psychotropic medication and psychological therapy/case management, and 122 (12.2%) psychological therapy/case management alone. Young people were often prescribed more than one medication; the most commonly recorded types were antidepressants (293 of 1237, 23.7%), benzodiazepines and other anxiolytics (169 of 1237, 13.7%), and antipsychotics (120 of 1237, 10.0%).
Discussion
We examined the demographic characteristics, circumstances of death, and social and clinical antecedents of suicide by people aged 10–24 years in Australia during 2006–2015. Three‐quarters of suicides were by boys and young men. In 41% of all cases, the young people who had taken their own lives had diagnosed mental disorders, and a further 16% had histories of possible mental health disorders. In all, 57% of young people had a either a diagnosed or possible mental health disorder, suggesting that the mental health and wellbeing of Australian young people should remain a key target for youth suicide prevention.
Several measures that have shown promise in reducing suicide risk have been discussed in the literature. Evidence‐based early intervention services can reduce suicide risk during treatment,17 and some young people require only short term interventions.18 A recent modelling study found that the youth suicide rate in Australia could be reduced markedly by providing coordinated care after discharge from emergency departments following treatment for self‐harm, and by increasing the capacity of specialist mental health services.19 Moreover, our findings suggest that further investment in drug and alcohol services could be helpful, as one‐third of young people who died by suicide had used illicit substances. Interventions that improve treatment engagement and adherence could also avert as many as one in ten suicide deaths.20 For example, the results of digital delivery of brief contact interventions to people who presented to emergency departments during suicidal crises have been promising,21 and should be further investigated for assisting digitally proficient young people.7
However, despite several government inquiries,7,22,23 there have been no efforts to systematically introduce clinical interventions for this purpose in emergency departments across Australia. Nor have there been coordinated efforts to strengthen service systems (eg, referral pathways) at critical points of entry, such as primary care, and discharge, such as emergency departments.7 Closing such gaps in service provision could assist prevention of youth suicide.
More than one‐third of young people who died by suicide resided in disadvantaged regions, confirming that poverty and social disparities are significant determinants of mental health for Australian youth. Further, 39% of young people were not employed or in education or training at the time of death. A major economic contraction has accompanied the coronavirus disease 2019 (COVID‐19) pandemic, and young adults have been particularly affected by job losses and financial stressors.24 Given the association between economic recession and suicide, particularly among young men,25 investments that provide financial security for young people not in education or employment (eg, JobKeeper and JobSeeker) should remain a national priority.
We found that 36% of boys and young men and 39% of girls and young women communicated their distress to family and friends prior to their suicides, either online or directly. A recent psychological autopsy study found that next of kin have significantly greater knowledge of suicide warning signs than health care professionals,26 and could consequently be usefully consulted during clinical decision making. As hanging is the most frequent method of suicide used by young people11 and has a high fatality rate (83%),27 engaging relatives in safety planning and means restriction counselling3 may be particularly useful.
Improving the ability of community members (including other young people) to detect and respond to people at risk of self‐harm in others is critical. A United States study found that providing gatekeeper training to students at 18 schools increased their mental health literacy, their willingness to seek help, and their confidence in talking about suicide.28 An Australian study that included 20 000 construction workers found that levels of mental health and suicide prevention literacy were lower in younger than older men, but that young men were amenable to education, particularly when delivered in the workplace.29
Limitations
First, coroners’ determinations of intent may have led to our excluding some suicides as accidental deaths or as being of undetermined intent.30 Second, when data were not recorded for a particular variable, we assumed a negative value or that the variable was not relevant to the case. This may be particularly relevant for risk factors such as possible mental health disorders, sexual and gender identity, Indigenous status, and history of abuse and neglect, which may be more reliably ascertainable from self‐reports. Third, our reliance on post mortem toxicology reports for information about psychopharmacological treatment meant that we did not have consistent data on dose, duration of treatment, or safety considerations, all important for the pharmaceutical management of young people at risk of suicide. Finally, we did not include a control group in our study, and the causal inferences that can be drawn from our cross‐sectional study are consequently limited.
Conclusion
In our national study, three‐quarters of the young people who died by suicide were boys or young men, and more than half had diagnosed or possible mental health disorders. More than two‐thirds of young people who died by suicide were not receiving therapy for mental health problems, suggesting that an opportunity for intervention is being missed. The availability and quality of specialist youth mental health services is currently being assessed as part of the Australian Productivity Commission assessment of mental health care services22 and in Victoria by a Royal Commission.23 We hope that these investigations, together with our findings, help improve access to and the quality of care for young people in Australia experiencing suicidal crises.
Box 2 – Demographic characteristics and circumstances of death for people aged 10–24 years who died by suicide, Australia, 2006–2015 (core NCIS variables data)
|
Characteristic |
Total |
Females |
Males |
||||||||||||
|
|
|||||||||||||||
|
Number of people |
3365 |
892 |
2473 |
||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
10–14 |
127 (3.8%) |
59 (6.6%) |
68 (2.7%) |
||||||||||||
|
15–19 |
1235 (36.7%) |
374 (41.9%) |
861 (34.8%) |
||||||||||||
|
20–24 |
2003 (59.5%) |
459 (51.5%) |
1544 (62.4%) |
||||||||||||
|
Mean (standard deviation) |
20.1 (2.9) |
19.2 (3.2) |
20.2 (2.8) |
||||||||||||
|
Aboriginal and Torres Strait Islander Australians |
484 (14.4%) |
153 (17.2%) |
331 (13.4%) |
||||||||||||
|
Socio‐economic status (IRSD)* |
|
|
|
||||||||||||
|
Most disadvantaged (deciles 1–3) |
1292 (38.4%) |
326 (36.5%) |
966 (39.1%) |
||||||||||||
|
Moderately disadvantaged (deciles 4–7) |
1295 (38.5%) |
349 (39.1%) |
946 (38.3%) |
||||||||||||
|
Least disadvantaged (deciles 8–10) |
778 (23.1%) |
217 (24.3%) |
561 (22.6%) |
||||||||||||
|
Remoteness* |
|
|
|
||||||||||||
|
Major cities/inner or outer regional |
3110 (92.4%) |
827 (92.7%) |
2283 (92.3%) |
||||||||||||
|
Remote/very remote |
255 (7.6%) |
65 (7.3%) |
190 (7.7%) |
||||||||||||
|
Method of suicide |
|
|
|
||||||||||||
|
Hanging or strangulation |
2341 (69.6%) |
638 (71.5%) |
1703 (68.9%) |
||||||||||||
|
Poisoning by gaseous substances |
183 (5.4%) |
31 (3.5%) |
152 (6.1%) |
||||||||||||
|
Fall from a height |
179 (5.3%) |
47 (5.3%) |
132 (5.3%) |
||||||||||||
|
Railway |
172 (5.1%) |
47 (5.3%) |
125 (5.1%) |
||||||||||||
|
Poisoning |
154 (4.6%) |
80 (9.0%) |
74 (3.0%) |
||||||||||||
|
Firearms |
130 (3.9%) |
6 (0.7%) |
124 (5.0%) |
||||||||||||
|
Crashed vehicle |
49 (1.5%) |
10 (0.8%) |
39 (1.6%) |
||||||||||||
|
Sharp object |
35 (1.0%) |
6 (0.7%) |
29 (1.2%) |
||||||||||||
|
Jumped in front of vehicle |
32 (1.0%) |
7 (0.8%) |
25 (1.0%) |
||||||||||||
|
Drowning |
15 (0.4%) |
0 |
15 (0.6%) |
||||||||||||
|
Immolation or thermal injury |
11 (0.3%) |
0 |
11 (0.4%) |
||||||||||||
|
Location of suicide |
|
|
|
||||||||||||
|
Home |
2242 (66.6%) |
655 (73.4%) |
1587 (64.2%) |
||||||||||||
|
Public recreation setting |
433 (12.9%) |
87 (9.8%) |
346 (14.0%) |
||||||||||||
|
Transport setting |
410 (12.5%) |
93 (10.4%) |
317 (12.8%) |
||||||||||||
|
School or education setting |
50 (1.5%) |
10 (1.1%) |
40 (1.6%) |
||||||||||||
|
Medical service area or correctional setting |
62 (1.8%) |
18 (2.0%) |
44 (1.8%) |
||||||||||||
|
Industrial or commercial setting |
87 (2.6%) |
17 (1.9%) |
70 (2.8%) |
||||||||||||
|
Other |
81 (2.4%) |
12 (1.4%) |
69 (2.8%) |
||||||||||||
|
|
|||||||||||||||
|
IRSD = Index Relative Socio-economic Disadvantage;14 NCIS = National Coronial Information System. * Based on 2011 Statistical Areas 2 for area of residence.16 |
|||||||||||||||
Box 3 – Demographic and social characteristics, and adverse life events among people aged 10–24 years who died by suicide, Australia, 2006–2015 (free text data)
|
Characteristic |
Total |
Females |
Males |
||||||||||||
|
|
|||||||||||||||
|
Number of people |
3027 |
813 |
2214 |
||||||||||||
|
Demographic characteristics |
|
|
|
||||||||||||
|
Aged 18 years or less |
915 (30.2%) |
321 (39.5%) |
594 (26.8%) |
||||||||||||
|
Aboriginal or Torres Strait Islander |
458 (15.1%) |
148 (18.2%) |
310 (14.0%) |
||||||||||||
|
LGBTI identification |
67 (2.2%) |
26 (3.2%) |
41 (1.9%) |
||||||||||||
|
Employment/education at time of death |
|
|
|
||||||||||||
|
Employed |
994 (32.8%) |
172 (21.2%) |
822 (37.1%) |
||||||||||||
|
Enrolled in education/training |
879 (29.0%) |
334 (41.1%) |
545 (24.6%) |
||||||||||||
|
Neither employed nor in education/training |
1154 (38.1%) |
307 (37.8%) |
847 (38.3%) |
||||||||||||
|
Social characteristics |
|
|
|
||||||||||||
|
Living alone |
266 (8.8%) |
73 (9.0%) |
193 (8.7%) |
||||||||||||
|
Parents separated or divorced |
800 (26.4%) |
241 (29.6%) |
559 (25.3%) |
||||||||||||
|
Social isolation (past month) |
136 (4.5%) |
38 (4.7%) |
98 (4.4%) |
||||||||||||
|
Difficulty finding employment (past year) |
66 (2.2%) |
4 (0.5%) |
62 (2.8%) |
||||||||||||
|
Financial problems at the time of death |
174 (5.8%) |
28 (3.4%) |
146 (6.6%) |
||||||||||||
|
Job loss past month |
58 (1.9%) |
4 (0.5%) |
54 (2.4%) |
||||||||||||
|
Family problems or conflict (lifetime) |
524 (17.3%) |
178 (21.9%) |
346 (15.6%) |
||||||||||||
|
Family problems or conflict (past year) |
486 (16.1%) |
160 (19.7%) |
326 (14.7%) |
||||||||||||
|
Peer problems or conflict (past year) |
150 (5.0%) |
65 (8.0%) |
85 (3.8%) |
||||||||||||
|
Difficulty making friends (lifetime) |
76 (2.5%) |
17 (2.1%) |
59 (2.7%) |
||||||||||||
|
History of bullying (lifetime) |
76 (2.5%) |
40 (4.9%) |
36 (1.6%) |
||||||||||||
|
Relationship breakdown (past year) |
634 (20.9%) |
144 (17.7%) |
490 (22.1%) |
||||||||||||
|
Relationship breakdown (past month) |
517 (17.1%) |
115 (14.1%) |
402 (18.2%) |
||||||||||||
|
Relationship breakdown (past week) |
261 (8.6%) |
70 (8.6%) |
191 (8.6%) |
||||||||||||
|
Adverse life events |
|
|
|
||||||||||||
|
Death of parent (lifetime) |
142 (4.7%) |
36 (4.4%) |
106 (4.8%) |
||||||||||||
|
Exposure to suicide (lifetime) |
202 (6.7%) |
59 (7.3%) |
143 (6.5%) |
||||||||||||
|
Exposure to suicide (past year) |
109 (3.6%) |
42 (5.2%) |
67 (3.0%) |
||||||||||||
|
History of abuse or neglect (lifetime) |
223 (7.4%) |
120 (14.8%) |
103 (4.7%) |
||||||||||||
|
Exposure to domestic violence (lifetime) |
76 (2.5%) |
47 (5.8%) |
29 (1.3%) |
||||||||||||
|
Contact with child protection services (lifetime) |
52 (1.7%) |
27 (3.3%) |
25 (1.1%) |
||||||||||||
|
Contact with juvenile justice system (lifetime) |
31 (1.0%) |
2 (0.2%) |
29 (1.3%) |
||||||||||||
|
|
|||||||||||||||
|
LGBTI = lesbian, gay, bisexual, transgender, intersex. |
|||||||||||||||
Box 4 – Mental health history and history of self‐harm or suicidal ideation among people aged 10–24 years who died by suicide, Australia, 2006–2015
|
Characteristic |
Total |
Females |
Males |
||||||||||||
|
|
|||||||||||||||
|
Number of people |
3027 |
813 |
2214 |
||||||||||||
|
Mental health history |
|
|
|
||||||||||||
|
Diagnosed mental health disorder |
1237 (40.9%) |
407 (50.1%) |
830 (37.5%) |
||||||||||||
|
Possible mental health disorder |
475 (15.7%) |
120 (14.8%) |
355 (16.0%) |
||||||||||||
|
Mental health treatment at time of death (diagnosed mental health disorder) |
1100 (36.3%) |
388 (47.7%) |
712 (32.2%) |
||||||||||||
|
Diagnosed mental health disorders |
1237 |
407 |
830 |
||||||||||||
|
Depression |
902 [72.9%] |
314 [77.1%] |
588 [70.8%] |
||||||||||||
|
Anxiety |
238 [19.2%] |
91 [22.4%] |
830 [17.7%] |
||||||||||||
|
Psychotic disorders |
175 [14.1%] |
37 [9.1%] |
138 [16.6%] |
||||||||||||
|
Substance misuse or dependence |
164 [13.3%] |
48 [11.8%] |
116 [14.0%] |
||||||||||||
|
Personality disorder |
94 [7.6%] |
62 [15.2%] |
32 [3.9%] |
||||||||||||
|
Bipolar disorder |
74 [6.0%] |
30 [7.4%] |
44 [5.3%] |
||||||||||||
|
Attention deficit/hyperactivity disorder |
73 [5.9%] |
10 [2.5%] |
63 [7.6%] |
||||||||||||
|
Post‐traumatic stress disorder |
39 [3.2%] |
22 [5.4%] |
17 [2.0%] |
||||||||||||
|
Eating disorder |
39 [3.2%] |
33 [16.2%] |
6 [0.3%] |
||||||||||||
|
Autism spectrum disorder |
41 [3.3%] |
3 [0.4%] |
38 [4.6%] |
||||||||||||
|
Disruptive behaviour disorders |
17 [1.4%] |
3 [0.4%] |
14 [1.7%] |
||||||||||||
|
Not indicated |
54 [4.4%] |
26 [6.4%] |
56 [6.7%] |
||||||||||||
|
History of self‐harm or suicidal ideation |
|
|
|
||||||||||||
|
Suicide attempt or self‐harm (lifetime) |
940 (31.1%) |
381 (46.9%) |
559 (25.3%) |
||||||||||||
|
Suicide attempt or self‐harm (past year) |
161 (5.3%) |
78 (9.6%) |
83 (3.7%) |
||||||||||||
|
Suicide attempt or self‐harm (past month) |
88 (2.9%) |
38 (4.7%) |
50 (2.3%) |
||||||||||||
|
Suicide attempt or self‐harm (past week) |
39 (1.3%) |
18 (2.2%) |
21 (0.9%) |
||||||||||||
|
Behaviour before suicide |
|
|
|
||||||||||||
|
Suicide note written |
815 (26.9%) |
242 (27.1%) |
573 (23.2%) |
||||||||||||
|
Communicated about suicidal ideation |
1123 (37.1%) |
319 (39.2%) |
804 (36.3%) |
||||||||||||
|
Communicated about suicidal ideation more than once |
1017 (33.6%) |
161 (19.8%) |
401 (18.1%) |
||||||||||||
|
Internet search for suicide methods |
90 (3.0%) |
33 (4.1%) |
57 (2.6%) |
||||||||||||
|
Communicated about suicide on social media |
94 (3.1%) |
32 (3.9%) |
62 (2.8%) |
||||||||||||
|
Substance misuse |
|
|
|
||||||||||||
|
Illicit substances detected at time of death |
852 (28.1%) |
183 (22.5%) |
669 (30.2%) |
||||||||||||
|
Cannabis |
672 (22.2%) |
147 (18.1%) |
525 (23.7%) |
||||||||||||
|
Methamphetamine |
222 (7.3%) |
45 (5.5%) |
177 (8.0%) |
||||||||||||
|
Other illicit substances |
101 (3.3%) |
25 (3.1%) |
76 (3.4%) |
||||||||||||
|
Alcohol detected at time of death |
1015 (33.5%) |
202 (24.9%) |
813 (36.7%) |
||||||||||||
|
Alcohol concentration > 150 mg/dL at time of death |
350 (11.6%) |
70 (8.6%) |
280 (12.6%) |
||||||||||||
|
Binge drinking or excessive alcohol consumption (past month) |
485 (16.0%) |
100 (15.2%) |
385 (13.8%) |
||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 5 – Contact with mental health services by people aged 10–24 years who died by suicide, Australia, 2006–2015
|
Contact with mental health services |
Total |
Females |
Males |
||||||||||||
|
|
|||||||||||||||
|
Number of people |
3027 |
813 |
2214 |
||||||||||||
|
Emergency department |
|
|
|
||||||||||||
|
Lifetime |
228 (7.5%) |
83 (10.2%) |
145 (6.6%) |
||||||||||||
|
More than one episode (lifetime) |
54 (1.8%) |
31 (3.8%) |
23 (1.0%) |
||||||||||||
|
Past year |
211 (7.0%) |
78 (9.6%) |
133 (6.0%) |
||||||||||||
|
Past month |
106 (3.5%) |
42 (5.2%) |
64 (2.9%) |
||||||||||||
|
Past week |
71 (2.3%) |
26 (3.2%) |
45 (2.0%) |
||||||||||||
|
Hospital admission |
|
|
|
||||||||||||
|
Lifetime |
496 (16.4%) |
190 (23.4%) |
306 (13.8%) |
||||||||||||
|
More than one episode (lifetime) |
169 (5.6%) |
86 (10.6%) |
83 (3.7%) |
||||||||||||
|
Past year |
366 (12.1%) |
148 (18.2%) |
218 (9.8%) |
||||||||||||
|
Past month |
168 (5.6%) |
72 (8.9%) |
96 (4.3%) |
||||||||||||
|
Past week |
89 (2.9%) |
39 (4.8%) |
50 (2.3%) |
||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 3 June 2020, accepted 7 October 2020
- Nicole TM Hill1,2
- Katrina Witt2
- Gowri Rajaram2
- Patrick D McGorry2
- Jo Robinson2
- 1 Telethon Kids Institute, Perth, WA
- 2 Orygen Centre for Youth Mental Health, University of Melbourne, Melbourne, VIC
We thank Sarah Hetrick for her help with grouping the mental health symptoms included in our study. Our study was funded by the William Buckland Foundation and the Future Generations Global Foundation. Jo Robinson and Katrina Witt are supported by National Health and Medical Research Council Career Development Fellowships (1142348, 1177787). Patrick McGorry is supported by a National Health and Medical Research Council Senior Principal Research Fellowship (1155508).
No relevant disclosures.
- 1. Australian Bureau of Statistics. 3303.0 Causes of death, Australia, 2018. Sept 2019. https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/2018 (viewed Mar 2020).
- 2. Cha CB, Franz PJ, E MG, et al. Annual research review. Suicide among youth: epidemiology, etiology, and treatment. J Child Psychol Psychiatry 2017; 59: 460–482.
- 3. Hawton K, Saunders KE, O’Connor RC. Self‐harm and suicide in adolescents. Lancet 2012; 379: 2373–2382.
- 4. Gili M, Castellvi P, Vives M, et al. Mental disorders as risk factors for suicidal behavior in young people: a meta-analysis and systematic review of longitudinal studies. J Affect Disord 2019; 245: 152–162.
- 5. Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry 2006; 47: 372–394.
- 6. Hill NTM, Robinson J, Pirkis J, et al. Association of suicidal behavior with exposure to suicide and suicide attempt: a systematic review and multilevel meta-analysis. PLoS Med 2020; 17: e1003074.
- 7. Robinson J, Bailey E, Browne V, et al. Raising the bar for youth suicide prevention. Melbourne: Orygen, the National Centre of Excellence in Youth Mental Health, 2016. https://www.orygen.org.au/Policy/Policy-Reports/Raising-the-bar-for-youth-suicide-prevention/orygen-Suicide-Prevention-Policy-Report?ext= (viewed Mar 2020).
- 8. McNamara PM. Adolescent suicide in Australia: rates, risk and resilience. Clin Child Psychol Psychiatry 2013; 18: 351–369.
- 9. Kõlves K, McDonough M, Crompton D, et al. Choice of a suicide method: trends and characteristics. Psychiatry Res 2018; 260: 67–74.
- 10. Austin AE, van den Heuvel C, Byard RW. Cluster hanging suicides in the young in South Australia. J Forensic Sci 2011; 56: 1528–1530.
- 11. Kõlves K, de Leo D. Suicide methods in children and adolescents. Eur Child Adolesc Psychiatry 2017; 26: 155–164.
- 12. Page A, Morrell S, Hobbs C, et al. Suicide in young adults: psychiatric and socio‐economic factors from a case–control study. BMC Psychiatry 2014; 14: 68–77.
- 13. National Coroners Information System. Operational statistics: case closure. https://www.ncis.org.au/about-the-data/operational-statistics/ (viewed Oct 2019).
- 14. Australian Bureau of Statistics. 2033.0.55.001. Census of population and housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2011. IRSD. Mar 2013. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/2033.0.55.001main+features100052011 (viewed Nov 2019).
- 15. Australian Bureau of Statistics. TableBuilder. https://www.abs.gov.au/websitedbs/censushome.nsf/home/tablebuilder?opendocument&navpos=240 (viewed Nov 2019).
- 16. Australian Bureau of Statistics. 1270.0.55.001. Australian Statistical Geography Standard (ASGS): volume 1. Main structure and Greater Capital City Statistical Areas. July 2016. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/1270.0.55.001July%202016?OpenDocument (viewed July 2019).
- 17. Hawton K, Witt KG, Taylor Salisbury TL, et al. Interventions for self‐harm in children and adolescents. Cochrane Database Syst Rev 2015; CD012013.
- 18. Harris MG, Burgess PM, Chant DC, et al. Impact of a specialized early psychosis treatment programme on suicide. Retrospective cohort study. Early Interv Psychiatry 2008; 2: 11–21.
- 19. Cosgrave EM, Robinson J, Godfrey KA, et al. Outcome of suicidal ideation and behavior in a young, help-seeking population over a 2-year period. Crisis 2007; 28: 4–10.
- 20. Page A, Atkinson JA, Heffernan M, et al. A decision-support tool to inform Australian strategies for preventing suicide and suicidal behaviour. Public Health Res Prac 2017; 27: e2721717.
- 21. Larsen M, Shand F, Morley K, et al. A text message intervention to reduce repeat suicidal episodes: design and development of Reconnecting After a suicide attempt (RAFT). JMIR Mental Health 2017; 4: e56.
- 22. Australian Productivity Commission. Mental health: draft report. Oct 2019. https://www.pc.gov.au/inquiries/completed/mental-health/draft (viewed Feb 2020).
- 23. Royal Commission into Victoria’s Mental Health System. Interim report summary (Parliamentary paper no. 101, 2018–19). Nov 2019. https://rcvmhs.vic.gov.au/download_file/view_inline/2179 (viewed Feb 2020).
- 24. Montenovo L, Xuan J, Rojas F, et al. Determinants of disparities in COVID-19 job losses. National Bureau of Economic Research [online], May 2020. https://www.nber.org/papers/w27132 (viewed May 2020).
- 25. Barr B, Taylor-Robinson D, Scott-Samuel A, et al. Suicides associated with the 2008–10 economic recession in England: time trend analysis. BMJ 2012; 345: e5142.
- 26. Draper B, Krysinska K, Snowdon J, et al. Awareness of suicide risk and communication between health care professionals and next-of-kin of suicides in the month before suicide. Suicide Life Threat Behav 2018; 48: 449–458.
- 27. Elnour AA, Harrison J. Lethality of suicide methods. Inj Prev 2008; 14: 39–45.
- 28. Wyman PA, Brown CH, LoMurray M, et al. An outcome evaluation of the Sources of Strength suicide prevention program delivered by adolescent peer leaders in high schools. Am J Public Health 2010; 100: 1653–1661.
- 29. King TL, Batterham PJ, Lingard H, et al. Are young men getting the message? Age differences in suicide prevention literacy among male construction workers. Int J Environ Res Public Health 2019; 16: 475–487.
- 30. De Leo D, Dudley MJ, Aebersold CJ, et al. Achieving standardised reporting of suicide in Australia: rationale and program for change. Med J Aust 2010; 192: 452–456. https://www.mja.com.au/journal/2010/192/8/achieving-standardised-reporting-suicide-australia-rationale-and-program-change





Abstract
Objective: To assess the demographic, social, and clinical characteristics of young Australians who die by suicide.
Design: Retrospective analysis of National Coronial Information System (NCIS) data.
Setting, participants: People aged 10–24 years who died by suicide in Australia during 2006–2015.
Main outcome measures: Demographic, social, and clinical characteristics of young people who died by suicide; circumstances of death recorded in the NCIS.
Results: 3365 young people died of suicide during 2006–2015 (including 2473 boys and men, 73.5%); 1292 people (38.4%) lived in areas of greater socio‐economic disadvantage. Free text reports were included in the NCIS for 3027 people (90%), of whom 1237 (40.9%) had diagnosed mental health disorders and 475 (15.7%) had possible mental health disorders. Alcohol consumption near the time of death was detected in 1015 of 3027 cases (33.5%); histories of self‐harm were recorded in 940 cases (31.1%) and of illicit substance misuse in 852 (28.1%). Adverse life events included history of abuse or neglect (223, 7.4%), suicide of relatives, friends, or acquaintances (202, 6.7%), and financial difficulties (174, 5.8%).
Conclusions: Three‐quarters of the young people who died by suicide were boys or young men, and 57% had diagnosed or possible mental health disorders, suggesting that the mental health and wellbeing of young Australians should be a key target for youth suicide prevention. To reduce the number of youth suicides, it is imperative that prevention strategies target the mental health and psychosocial stressors that lead to suicidal crises in young people.