A live‐streamed teaching strategy that can be applied to all areas of medicine and many clinical scenarios
The emergence of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has resulted in unprecedented challenges to hospitals, the community and society. Although the necessary focus has been to care for patients and communities, the profound effects of coronavirus disease 2019 (COVID‐19) have disrupted medical education and required intense and prompt attention from medical educators. COVID‐19 poses unique challenges to the clinical clerkship model that is fundamental to medical students’ education and has the potential to change forever how future physicians are educated.1
For more than a decade, medical schools have been working to transform pedagogy by reducing live face‐to‐face didactic lectures; using technology and simulation; implementing team‐facilitated, active and self‐directed learning; and promoting individualised and interprofessional education.2,3 However, as described by Sir William Osler, clinical teaching of medical students at the bedside remains vitally important: “to study the phenomena of disease without books is to sail an uncharted sea, while to study without patients is not to go to sea at all”.4 Medical graduates must function in a team‐based, collaborative work environment, have sound knowledge and clinical skills, and have a capacity for lifelong learning.5
In response to COVID‐19, there has been rapid development of the “boot camp” model of accelerated learning for final year medical students to support their swift transition to assistants in medicine. However, it is unclear how medical schools will manage students from the middle years of medical school, where clinical exposure is a vital part of clinical education. Typically, during years 3 and 4 of the Doctor of Medicine degree at the University of Newcastle, students spend about 50% of their time attached to wards, clinics, operating theatres and other clinical exposure opportunities. How can this clinical education continue while medical students are omitted from the clinical environment due to the COVID‐19 pandemic? Further, given that social distancing is anticipated to last many months, clinical teaching rounds with multiple medical students are unlikely to be able to recommence soon.
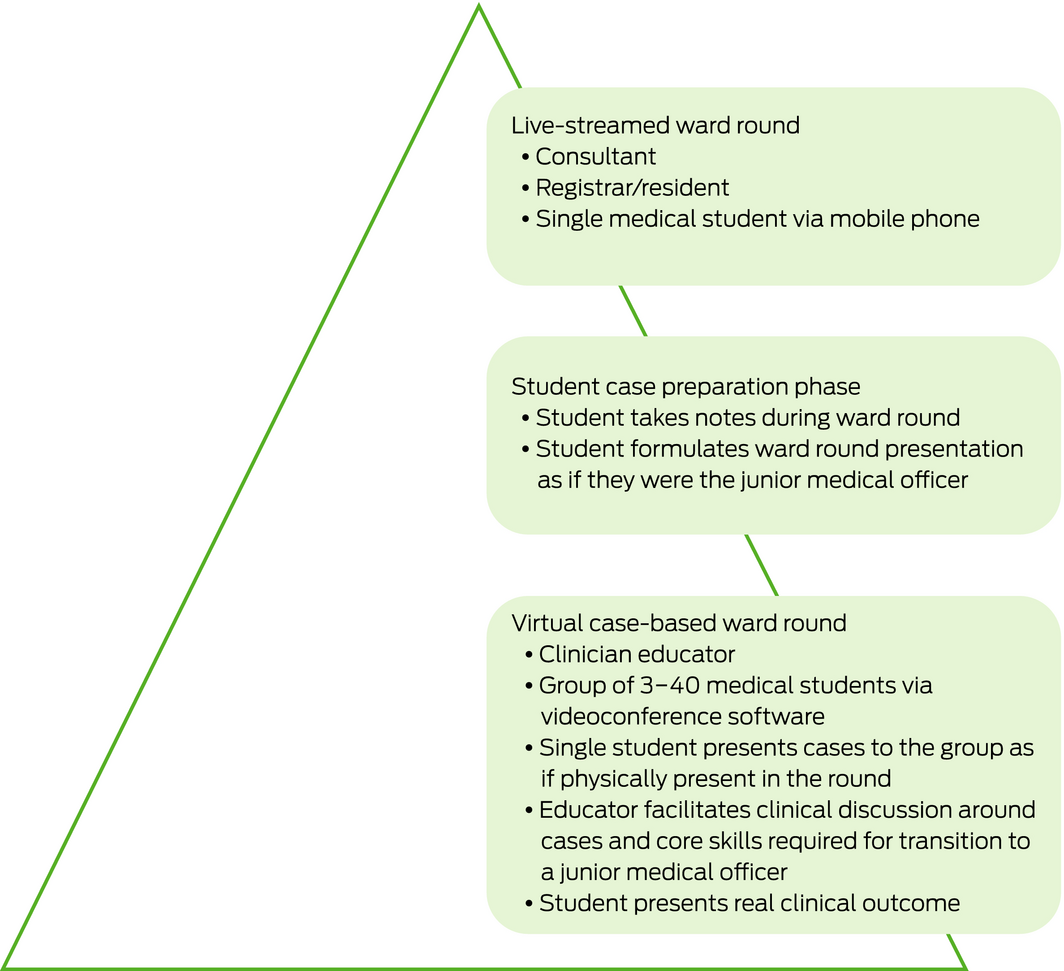
The clinical teaching team from the University of Newcastle at John Hunter Hospital have developed the concept of “live‐streamed ward rounds”. The initiative addresses the challenge of maintaining the clinical clerkship model of education while students are excluded from the hospital for several months during the vital early years of clerkship training. This model of education has three phases (Box 1), which broadly align to advanced cognitive levels of learning expected of medical students. The Hunter New England Local Health District Ethics Committee confirmed that ethics approval was not required for this project.
Phase 1: student remote observation (assess and analyse)
Clinicians undertake routine ward rounds with medical students in attendance as part of routine inpatient care. During live‐streamed ward rounds, a medical student is engaged securely (password‐protected) via mobile phone to participate in the ward round, including discussion before and after a patient visit. In addition to participating in discussions, similar to face‐to‐face teaching, the student can be shown clinical records (eg, pathology results, observation charts, medical imaging, intraoperative photographs) on video via platform‐agnostic streaming software (eg, Skype for Business, Pexip, Zoom) to broaden engagement with the clinical interaction. When the patient is visited, the patient provides verbal consent for student involvement in the live‐streamed round before the consultation. This is documented in the clinical record of each patient. After obtaining verbal consent, student introduction occurs by turning the phone around so the patient can see the student and vice versa.
After the introduction, the phone is turned back to the clinician so the student can see the clinician holding the phone to observe non‐verbal cues. No streaming of the clinical examination occurs during the patient encounter. When the consultation is complete, the phone is turned briefly to the patient to facilitate eye contact when the student thanks them for permission to participate in the encounter. This process is repeated with each patient on the ward round, after which the student is involved in the post‐round clinical discussion that occurs routinely as part of multidisciplinary patient care. The phone is muted or disconnected during the patient encounter if the patient declines student involvement.
Phase 2: student preparation (evaluate and synthesise)
During the live‐streamed ward round, the student is directed to take detailed notes so they can formulate a series of case presentations for the subsequent student case‐based ward round. The medical student obtains any missing medical information from the junior medical officer at the completion of Phase 1. Clinical records are not available electronically for the students. The aim is to prepare the student for the role of a junior medical officer in the ward environment.
Phase 3: student remote case‐based ward round presentation (construct and justify)
This element of the learning cycle is typically held later in the week of the live‐streamed clinical round at a time when three to 40 students can be engaged simultaneously for 60–90 minutes through videoconferencing software. The student who attended the live‐streamed clinical round presents each patient to the group as if they were a junior medical officer performing clinical handover. A clinician educator is present to facilitate case‐based discussion. After each patient is discussed, the student presents what actually occurred on the clinical round and presents the plan for ongoing care with justification. This element of the interaction is designed to emphasise patient‐centred care.
We have conducted live‐streamed rounds at John Hunter Hospital in obstetrics, gynaecology and birth suite handover rounds. Approval was provided by the hospital executive after review by the local health district privacy team — student involvement by phone using a secure application (Skype for Business) was thought to be similar to student involvement with telehealth consultations in outpatient clinics. The benefits and challenges experienced with live‐streamed ward rounds are summarised in Box 2. After completion of 50 live‐streamed rounds, an informal evaluation was conducted via an anonymous voluntary Qualtrics online survey. Most of the 25 student respondents and clinicians provided positive feedback. Key findings from this survey are presented in the Supporting information.
Clinical teaching is a fundamental component of medical education, particularly for developing tangible and intangible skills of medical students.6 Bedside teaching is a key opportunity for medical students, with the presence of the medical teacher, to develop medical knowledge, history taking and physical examination skills, clinical data gathering and clinical decision making.7 While students cannot participate in the clinical examination component of the patient interaction during live‐streamed ward rounds, they can hear the relevant history taking. Evidence indicates that physicians can collect 60–80% of the information relevant for a diagnosis just by taking a medical history, leading to a final diagnosis in more than 70% of cases.8
Previous studies investigating factors that are most important in creating an effective learning environment for medical students found that the level of participation students are afforded in the workplace is vital in clinical practice learning.9 Greater participation in the workplace facilitates greater confidence and competency, especially in clinical practice.9,10 A recent Australian study11 of final year medical students found the top six responses as to why students found clinical venues the most educationally useful include:
- the amount of patient contact;
- various patient presentations;
- being part of the clinical team;
- the opportunity to ask questions and receive useful information;
- the high level of supervision in training; and
- the amount of formal bedside teaching.
Tutorials in a clinical setting also allow for professional development to be taught, such as communication, teamwork and ethics.12 Students require teaching in real clinical settings to develop skills for success in the real clinical environment.
The structured live‐streamed ward round stimulates student participation and effectively develops clinical knowledge, enhances depth and permanency of learning, and enriches the stability and dependability of the knowledge attained. Being able to follow up patients to discharge is the ideal ending to these scenarios, where the student can see how effective the management plan was, as well as its implementation and results.11
We identified quality supervision as a key factor for maximising the educational value of clinical learning in live‐streamed ward rounds. Supervisors who are experienced and engaging make students more motivated to critically analyse patients’ clinical conditions, encourage their learning about these presentations, and formulate management plans.13,14
Live‐streamed clinical encounters should inspire us to revisit and prioritise the development of virtual clinical encounters, involving detailed scenarios that can be delivered flexibly, are always accessible and adaptive, and prioritise individualised learning. There are many advantages to live‐streamed clinical encounters, including their cost‐effectiveness in both set‐up and maintenance, the possibility of increasing access and usability of streaming technology, and allowing for the nuance of expertise and immediate feedback. As demonstrated by the COVID‐19 pandemic, they can be rapidly implemented and use principles of adult learning.
The live‐streamed teaching strategy can be applied to all areas of medicine and many clinical scenarios, including ward rounds and clinical handover rounds. Recommendations on how to introduce this innovative teaching method are summarised in Box 3. This strategy is one of the many that the University of Newcastle plans to use to provide ongoing clinical teaching during the COVID‐19 pandemic. Being adaptable and flexible, cognisant of costs and driven by evidence are critical features of delivering medical education and contemporary medical practice.15
Box 2 – Benefits and challenges of live‐streamed ward rounds
|
|
|||||||||||||||
|
Benefits |
|
||||||||||||||
|
Challenges |
|
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Recommendations for introducing live‐streamed ward rounds into teaching
|
|
|||||||||||||||
|
Step 1 |
Design a live‐streamed round and a follow‐up reflective simulation round. This should include addressing the process for privacy, consent and technology (ie, preferred mobile videoconference platform) |
||||||||||||||
|
Step 2 |
Include discipline and departmental consultants running the live‐streamed round and follow‐up round in reviewing the design |
||||||||||||||
|
Step 3 |
Include technology support officers in reviewing the design |
||||||||||||||
|
Step 4 |
Seek written approval from relevant senior local health district and hospital staff (eg, medical and clinical directors) |
||||||||||||||
|
Step 5 |
Pilot, refine, implement |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- 1. Rose S. Medical student education in the time of COVID‐19. JAMA 2020;. https://doi.org/10.1001/jama.2020.5227. [Epub ahead of print].
- 2. Emanuel EJ. The inevitable reimagining of medical education. JAMA 2020;. https://doi.org/10.1001/jama.2020.1227. [Epub ahead of print].
- 3. Skochelak SE, Stack SJ. Creating the medical schools of the future. Acad Med 2017; 92: 16–19.
- 4. Osler W. On the need of a radical reform in our teaching methods: senior students. Med News 1903; 82: 49–53.
- 5. Haeri A, Hemmati P, Yaman H. What kind of curriculum can better address community needs? Problems arisen by hypothetical‐deductive reasoning. J Med Syst 2007; 31: 173–177.
- 6. Bahmanbijari B, Beigzadeh A. Medical professionalism: teaching and assessment tools. Rep Health Care 2015; 1: 69–72.
- 7. Beigzadeh A, Bahaadinbeigy K, Adibi P, et al. Identifying the challenges to good clinical rounds: a focus‐group study of medical teachers. J Adv Med Educ Prof 2019; 7: 62–73.
- 8. Faustinella F, Jacobs RJ. The decline of clinical skills: a challenge for medical schools. Int J Med Educ 2018; 9: 195–197.
- 9. Billett S. Learning in the workplace: strategies for effective practice. Sydney: Allen and Unwin, 2001.
- 10. Sheehan D, Wilkinson T, Paltridge D. A tool to evaluate effective learning environments within clinical attachments for interns. Focus Health Prof Educ 2008; 10: 1–10.
- 11. Kandiah DA. Perception of educational value in clinical rotations by medical students. Adv Med Educ Pract 2017; 8: 149–162.
- 12. Sheehan D, Bagg W, de Beer W, et al. The good apprentice in medical education. N Z Med J 2010; 123: 89–96.
- 13. Sheehan D, Wilkinson TJ. Maximising the clinical learning of junior doctors: applying educational theory to practice. Med Teach 2007; 29: 827–829.
- 14. Al Kadri HM, Al‐Moamary MS, Elzubair M, et al. Exploring factors affecting undergraduate medical students’ study strategies in the clinical years: a qualitative study. Adv Health Sci Educ Theory Pract 2011; 16: 553–567.
- 15. Wittert GA, Nelson AJ. Medical education: revolution, devolution and evolution in curriculum philosophy and design. Med J Aust 2009; 191: 35–37. https://www.mja.com.au/journal/2009/191/1/medical-education-revolution-devolution-and-evolution-curriculum-philosophy-and.





We acknowledge the support of Brian Kelly and Michael Hensley in this teaching initiative and of William Lai for the informal evaluation of this initiative. We thank our patients and teaching fellows for their participation during the development of this model of teaching.
No relevant disclosures.