To the Editor: The coronavirus disease 2019 (COVID‐19) pandemic has required rapid adjustments in health service delivery.1 The Victorian COVID‐19 Cancer Network (VCCN) is a joint initiative of the Victorian Comprehensive Cancer Centre and Monash Partners Comprehensive Cancer Consortium. Through expert groups, the VCCN aims to provide support and advice to clinicians and health care services treating cancer patients during the pandemic.
The VCCN Telehealth Expert Working Group conducted a survey to understand the barriers and enablers to the rapid adoption of telehealth in health services during the first week of April 2020. Seventeen cancer services from across metropolitan and regional Victoria and Tasmania responded. Notably, all respondent cancer services had implemented some form of telehealth since the pandemic. Healthdirect, the Victorian Department of Health and Human Services’ supported telehealth platform, was used in 40% of services, with 25% using phone only and others using platforms such as Skype, FaceTime and doxy.me.
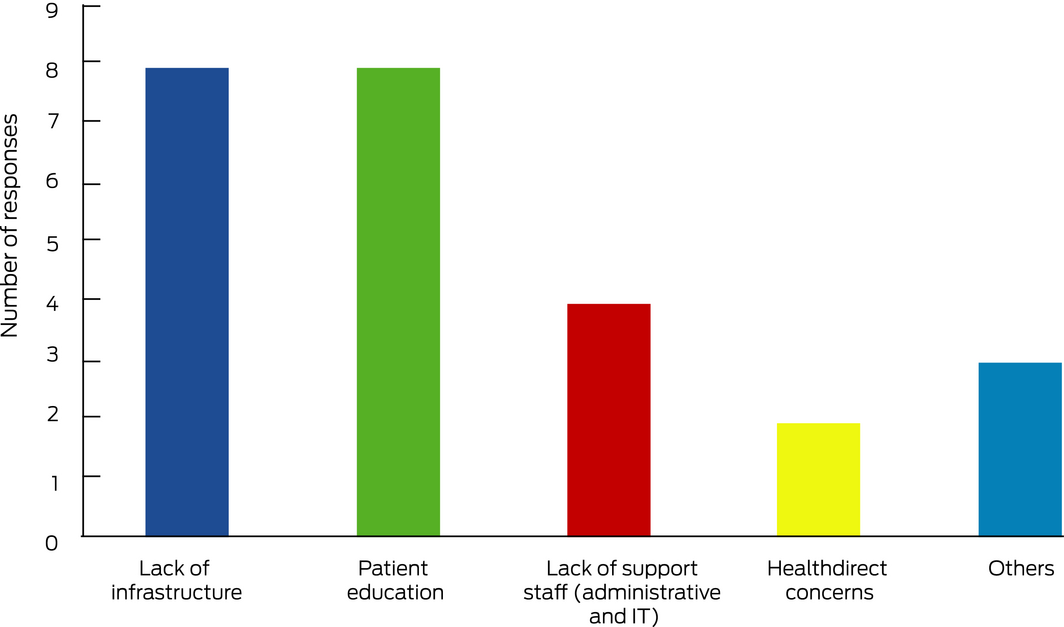
With the unprecedented increase in the uptake of telehealth,2 there is a tremendous opportunity to integrate telehealth into routine practice, potentially improving inequities and inefficiencies in the delivery of cancer care for suitably selected patients. Our survey results suggest several areas for attention to support telehealth, including the need for further investment in information technology infrastructure across health services and administrative support to facilitate changes in practice and workflow (Box).
The survey results also highlight the educational and training needs of consumers and health professionals during telehealth implementation. Aboriginal and Torres Strait Islanders, people from culturally and linguistically diverse backgrounds and of lower socio‐economic status, and older patients may have greater needs and will require additional support from both government and relevant organisations to ensure equity of access to cancer care via telehealth.
We strongly advocate the need to establish evidence‐based, patient‐centred and sustainable telehealth in cancer management. Research into the experience of patients and clinicians should be prioritised to ensure the consistent quality of telehealth consultation with face‐to‐face consultation in appropriate clinical circumstances.
- 1. Australian Government Department of Health. Impact of COVID‐19 in Australia – ensuring the health system can respond. https://www.health.gov.au/resources/publications/impact-of-covid-19-in-australia-ensuring-the-health-system-can-respond (viewed June 2020).
- 2. Boyages S. COVID‐19 consequence: telehealth will go mainstream. InSight+ 2020; 20 Apr. https://insightplus.mja.com.au/2020/15/covid-19-consequence-telehealth-will-go-mainstream/ (viewed June 2020).





We thank the VCCN Telehealth Expert Working Group and Clinical Directors Group, and the Victorian Department of Health and Human Services.
Both authors are members of the VCCN Telehealth Expert Working Group.