As 60% of Indigenous people in the Northern Territory primarily speak languages other than English,1,2 greater use of interpreters in health care could improve outcomes for patients.3,4 Barriers to using Aboriginal interpreters at Royal Darwin Hospital have been described.1
We undertook a quasi‐experimental pilot study to determine the effects of a package of measures on the use of interpreters and patient outcomes at Royal Darwin Hospital. The intervention comprised employment of an Aboriginal interpreter coordinator (to advocate the use of interpreters, coordinate their efficient use, and support interpreters in the hospital), training for health care providers in working with Aboriginal interpreters, and the promotion of interpreter use. The primary outcome was the number of interpreter bookings by clinicians; secondary outcomes were the number of completed bookings — 20–30% of bookings are not completed because no interpreter with the required language is available, or the patient declines an interpreter, is discharged, or dies1 — and self‐discharge rates by Aboriginal patients. Language documentation and interpreter booking processes at the hospital are described in the online Supporting Information. The Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health Research approved the study (references, 2017‐3007, 2018‐3245).
Interpreter bookings data (provided by the Aboriginal Interpreter Service) and hospital separations data were obtained for all Aboriginal people admitted as public patients to Royal Darwin Hospital during 1 April 2016 – 31 March 2019. Torres Strait Islander patients, patients admitted for dialysis or same‐day procedures, and patients receiving care in psychiatry units (with an already high level of interpreter use) were excluded from our analysis. Outcomes were assessed by interrupted time series analysis:5 the baseline period was April 2016 – March 2018, and the intervention period was April 2018 – March 2019 (Supporting Information).
The intervention was associated with an immediate increase in Aboriginal interpreter bookings and a decline in self‐discharge numbers. During the baseline period, 10 582 of 21 163 Aboriginal inpatients (50%) required an interpreter; interpreters were booked for 1333 (12.6% of those needing an interpreter; 755 completed bookings, 57%). During the intervention, 5460 of 10 919 Aboriginal inpatients (50%) required an interpreter; interpreters were booked for 958 (17.5%; 607 completed bookings, 63%). The difference in regression slopes for bookings before (–0.35) and during (+0.16) the intervention was 0.51 (95% confidence interval [CI], 0.13–0.90) (Box). The difference in regression slopes for completed bookings was 0.21 (–0.11 v +0.10; 95% CI, 0.03–0.39). Self‐discharge rates fell from 12.0% to 10.1% (slope difference, –0.19; 95% CI, –0.34 to –0.04) (Box). The Aboriginal Interpreter Coordinator role appeared to be the most important component of the intervention, based on the timing of its introduction and its scope (data not shown).
Increased use of Aboriginal interpreters, critical for improving the quality of care and patient outcomes, can be achieved by targeted strategies. By the end of the study period, however, fewer than one in five Aboriginal patients needing interpreters had access to one. Considerable improvement is needed in the supply, demand and efficiency domains. Supply must be increased with recruitment and retention strategies, including interpreter mentoring. Drivers of demand include health care providers being equipped to deliver culturally safe care by knowing the names of Aboriginal languages, identifying which patients need interpreters, and knowing how to book and work effectively with interpreters. Efficiency requires new models for integrating interpreters in different contexts (ward rounds, outpatient care) and service coordination. These aspects are being examined in the further stages of this project.
Box – Study outcomes during the baseline and intervention phases. A. Proportion of Aboriginal patients requiring interpreters for whom interpreters were booked. B. Proportion of hospital admissions of Aboriginal people ending in self‐discharge*
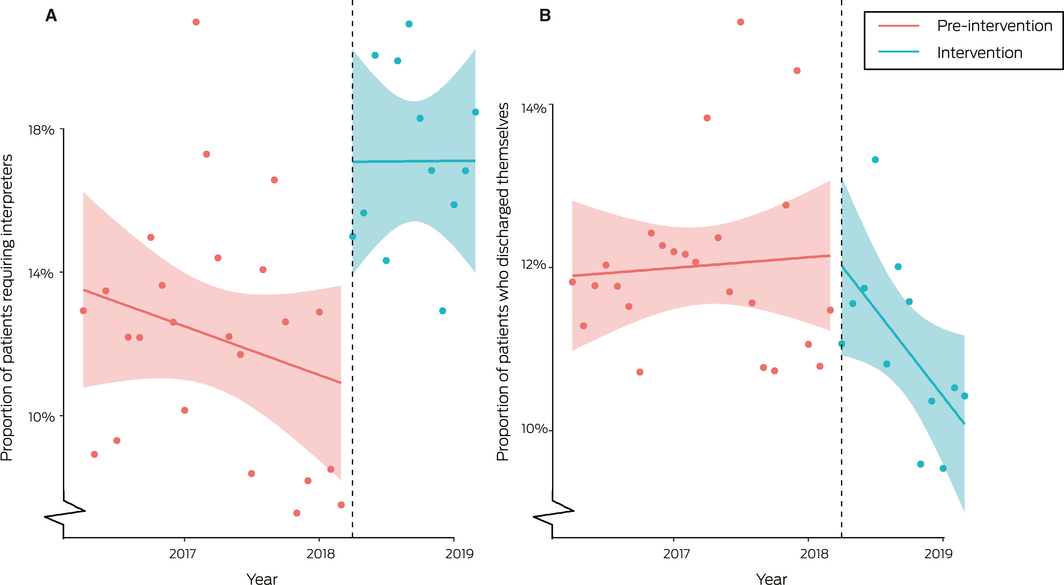
* Data points: monthly mean values; solid line: line fitted by linear regression; shaded envelope: 95% confidence interval for fitted line; dotted line: commencement date of Aboriginal Interpreter Coordinator appointment.
Received 25 March 2020, accepted 28 May 2020
- 1. Ralph AP, Lowell A, Murphy J, et al. Low uptake of Aboriginal interpreters in healthcare: exploration of current use in Australia's Northern Territory. BMC Health Serv Res 2017; 17: 733.
- 2. Australian Bureau of Statistics. 4713.7.55.001. Population characteristics, Aboriginal and Torres Strait Islander Australians, Northern Territory, 2006. May 2010. http://www.abs.gov.au/AUSSTATS/abs@.nsf/MF/4713.7.55.001 (viewed May 2020).
- 3. Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev 2005; 62: 255–299.
- 4. Karliner LS, Jacobs EA, Chen AH, at al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res 2007; 42: 727–754.
- 5. Linden A. Conducting interrupted time‐series analysis for single‐ and multiple‐group comparisons. Stata J 2015; 15: 480–500.





*The Communicate Study group:
Anna P Ralph1,2
Craig Castillon2
Vincent Mithen1
Gail Madrill2
Vicki Kerrigan1
Zhiqiang Wang1
Curtis Roman3
Bhavini Patel2
Elise O'Connor2
Martin Hansen2
Natasha Keillor2
Robyn Aitken4
Alan Cass1
1 Menzies School of Health Research, Charles Darwin University, Darwin, NT.
2 Royal Darwin Hospital, Darwin, NT.
3 Aboriginal Interpreter Service, Northern Territory Department of Local Government, Housing and Community Development, Darwin, NT.
4 Flinders University, Adelaide, SA. anna.ralph@menzies.edu.au
Our study was supported by the Menzies School of Health Research Grants Scheme, and by the National Health and Medical Research Council (Improving Health Outcomes in the Tropical North: A Multidisciplinary Collaboration [HOT NORTH], GNT1131932). Anna Ralph is supported by a National Health and Medical Research Council fellowship (1142011). We greatly thank the Aboriginal Interpreter Service and Top End Health Services for providing the data.
No relevant disclosures.