In 2014, we reported in the MJA our findings, based on linked data for cervical screening and human papillomavirus (HPV) vaccination of women in Victoria, that participation of young women in cervical screening during 2010 and 2011 was significantly lower among HPV‐vaccinated than among unvaccinated women.1
In 2018, we had the opportunity to repeat the study at the national level as part of a broader data linkage study of cancer outcomes and screening behaviour across the three national cancer screening programs in Australia.2
In the original study (2014), the Australian Institute of Health and Welfare (AIHW) data linkage unit applied probabilistic name‐based linkage to HPV vaccination and cervical screening data. We acknowledged it was likely that some screened women who were vaccinated would be incorrectly identified as unvaccinated because many young women would have changed their names and addresses between vaccination and cervical screening.
In the more recent study (2018), the AIHW again used probabilistic name‐based linkage, but first updated HPV vaccination and cervical screening data by obtaining histories of name and address changes from the Medicare Enrolment File. Medicare registrants’ details are updated when new data are provided to Medicare, the national health care scheme, and are recorded in new records with dates of change. The Australian Department of Human Services agreed to provide these data to the AIHW for data linkage purposes for our 2018 study. Our investigation was approved by the AIHW Ethics Committee (reference, EO 2014‐4‐130) and by state and territory human research ethics committees.
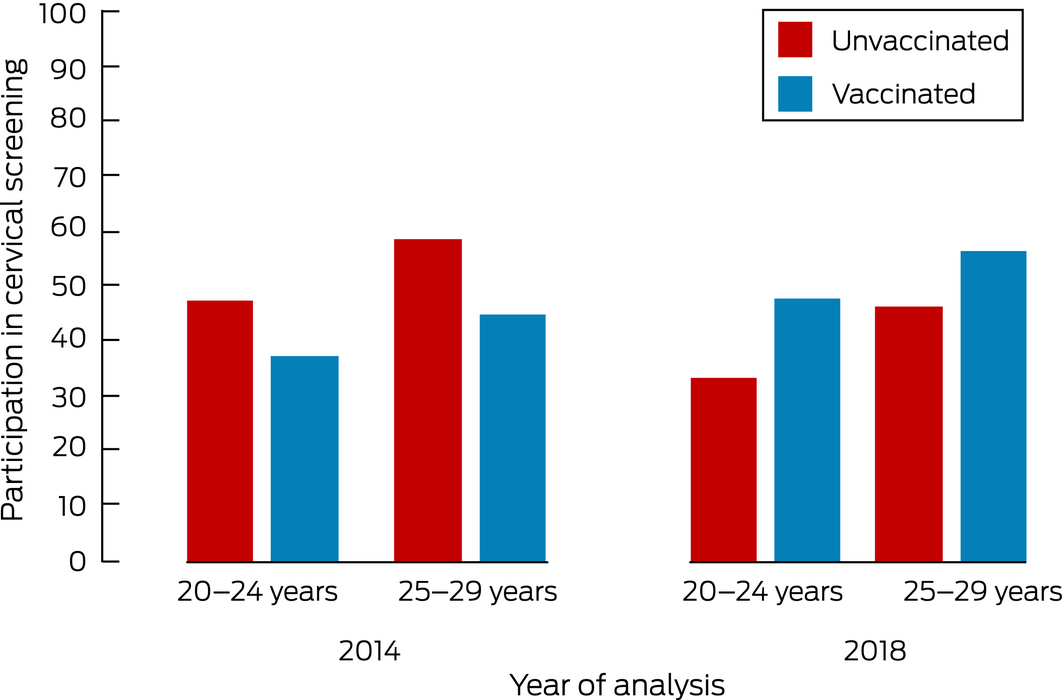
After incorporating Medicare data, annual cervical screening rates for Victorian women aged 20–24 years or 25–29 years were higher during 2010 and 2011 for vaccinated than unvaccinated women,2 contrary to our 2014 findings.1 For 20–24‐year‐old Victorian women, the difference in rate changed from 10.1% lower to 14.7% higher for vaccinated women, and for 25–29‐year‐old women from 13.5% lower to 10.0% higher (Box).
Our updated findings are consistent with findings from other countries of higher cervical screening participation among women who have been vaccinated against HPV.3,4,5
Incorporating the Medicare Enrolment File into the 2018 linkage was a test of proof of concept. Its successful use in this and similar studies has led to the AIHW data linkage unit granting ethics approval and relevant authorisations for employing the Medicare Enrolment File as a tool for improving the quality of other data linkage studies.
The key message of our original study, however, remains unchanged. All women, whether vaccinated against HPV or not, should be encouraged to participate in cervical screening: the HPV vaccine does not protect against all HPV types, and many women in Australia were sexually active before they were vaccinated. While it is as yet unclear whether the association between vaccination and screening will persist for women who were routinely vaccinated at school, it is crucial that we focus on strategies that effectively engage women who do not currently participate in screening.
Received 30 September 2019, accepted 8 November 2019
- 1. Budd AC, Brotherton JML, Gertig DM, et al. Cervical screening rates for women vaccinated against human papillomavirus. Med J Aust 2014; 201: 279–282. https://www.mja.com.au/journal/2014/201/5/cervical-screening-rates-women-vaccinated-against-human-papillomavirus.
- 2. Australian Institute of Health and Welfare. Analysis of cancer outcomes and screening behaviour for national cancer screening programs in Australia (Cat. no. CAN 115; Cancer series no. 111). Canberra: AIHW, 2018.
- 3. Boone SD, Pinkston CM, Baumgartner KB, et al. Associations between prior HPV4 vaccine doses and cervical cancer screening participation. Cancer Epidemiol 2016; 42: 108–114.
- 4. Kreusch T, Wang J, Sparén P, et al. Opportunistic HPV vaccination at age 16–23 and cervical screening attendance in Sweden: a national register‐based cohort study. BMJ Open 2018; 8: e024477.
- 5. Palmer TJ, McFadden M, Pollock KG, et al. HPV immunisation and increased uptake of cervical screening in Scottish women; observational study of routinely collected national data. Br J Cancer 2016; 114: 576–581.





Julia Brotherton was an investigator on investigator‐initiated research grants that provided funding for laboratory testing for a study of cervical cancers (Seqirus) and recurrent respiratory papillomatosis (Merck) more than three years ago, but did not receive personal financial benefits.