Widespread adoption of digital health tools requires comprehensive evidence of their effectiveness and value
Medication‐related problems are a significant and often undetected health care issue outside of formal medication review services. These problems can delay or prevent clinical improvements and may result in preventable harm. Electronic medication management systems within hospitals are largely assumed to reduce such harm; however, as described by Westbrook and Baysari elsewhere in this Supplement,1 the evidence for this is limited. Digital technologies for consumers extend the scope of care beyond health organisations and may offer an additional avenue for reducing medication‐related problems. While there are several non‐digital strategies that help people take their medicines correctly (eg, dose administration aids, home medicines reviews and pharmacy services), digital technologies such as medication management apps and wearable sensor devices can potentially also support medication management by consumers. However, despite this potential, and the launch of smartphones more than a decade ago, consumer‐directed digital health tools are seldom used in clinical practice.
Medication management: there are (too many) apps for that
One of the barriers to adoption of digital technologies for medication management is navigating the overcrowded market. A review conducted in 2017 identified more than 800 medication management apps designed to support medication adherence, available from the Windows, iTunes, Google Play and Blackberry app stores.2
Current medication management apps utilise different strategies to improve medication use, and can be roughly segregated into three categories: education techniques, reminder and management techniques, and behavioural techniques.3 Education techniques include interactive content, such as structured texts and videos. Reminder and management techniques include options such as alarms, push notifications and short message service (SMS) alerts. Behavioural techniques include personal tracking, where users monitor their own use; external tracking, where data are shared with a health professional, family member or friend to create social accountability and promote the desired behaviour; and gamification, where rewards such as badges or points, are provided for high level adherence.
A review of 420 free medication adherence apps conducted in 2018 found the majority (59.5%) employed one mechanism to promote medication adherence, 35.5% used two mechanisms, while only 5.2% used all three mechanisms.3 Use of reminders was the most popular feature, with 92.1% of all medication adherence apps having some kind of reminder functionality.3 With regard to behavioural techniques, the authors found that personal tracking was the technique most commonly included, with external tracking and gamification relatively uncommon (5.2% and 1.2%, respectively).3 It is unclear whether these findings are applicable to paid apps, as they were excluded from this analysis.
Studies suggest that app quality varies greatly. The above evaluation of over 800 free and paid apps resulted in a median quality score (based on their descriptions only) of 14 out of 68 (range, 0–60) for the 645 apps eligible for evaluation.2 While all apps claimed to support adherence, user testing of 144 of the highest ranking apps found 9% were unable to send reliable medication reminders and fewer than half (40%) were able to send reminders for three complex medication schedules (eg, weekly dosing or alternate day dosing). About half provided the ability to postpone reminders, only 61% tracked missed doses or doses taken, and just under half (47%) provided alerts for when to refill a prescription.2
Situations where medication adherence is particularly important and problematic — such as clinical trials, cancer chemotherapy, treatment of some mental illnesses and long term antibiotic use for tuberculosis — may require additional auditing mechanisms or alternative digital strategies. Devices that provide direct or indirect information about pill taking, including automated pillboxes and smart pills that send signals when in contact with gastric acid, are being studied as means of ensuring medication intake.4 Directly observed therapy, a strategy to improve adherence by having someone observe the patient taking the medicine, can now be automated using a camera‐based smartphone app.5
Beyond apps: monitoring adverse effects
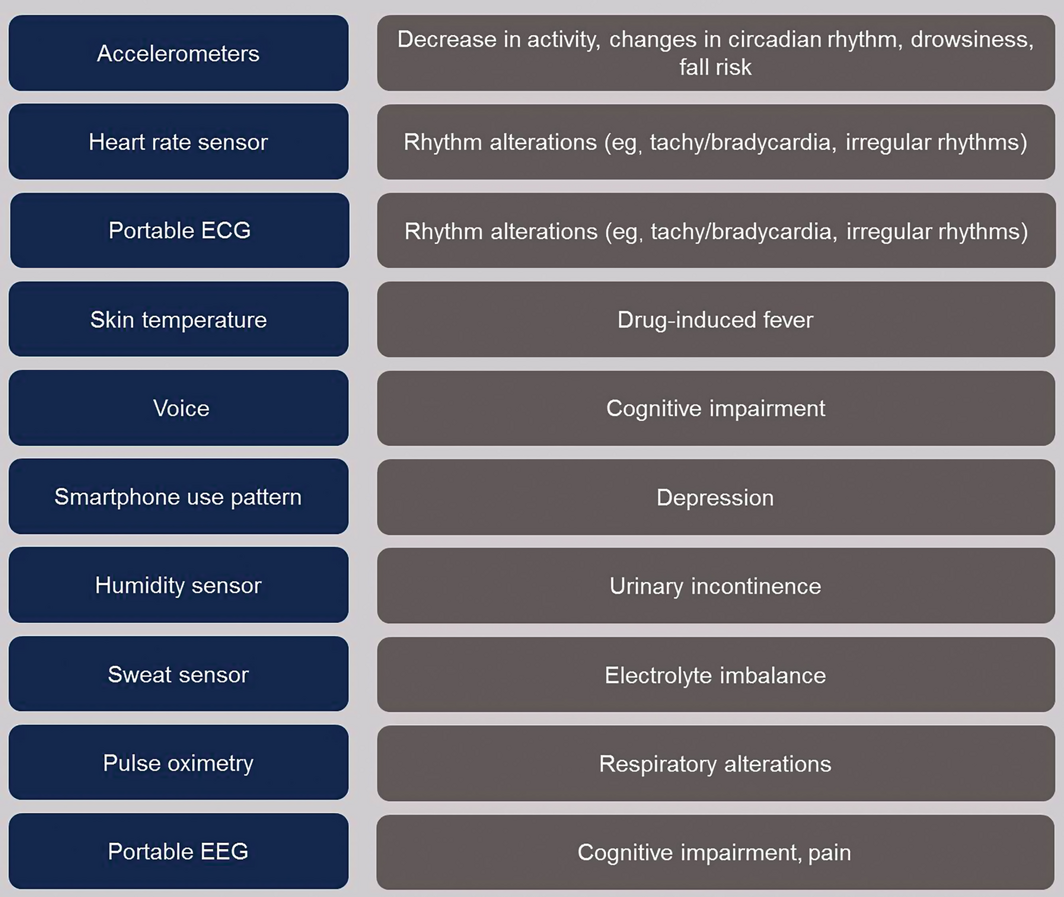
Adverse drug reactions are a major source of medication‐related harm. Recognising and responding to adverse medicine reactions in practice is often challenging, because many adverse effects of medicines are difficult to recognise. Such adverse effects include cognitive impairment and functional impairment; the latter may be due to sedation, muscle weakness or neuropathy, all of which reduce physical activity. Additional symptoms that can be medicine‐induced and hard to detect include loss of appetite, changes in urinary function and changes in respiration. In older people, these types of adverse effects may be misattributed as geriatric syndromes, frailty or “changes due to ageing”. The advent of wearable technologies has the potential to improve our ability to monitor the effects of medicines and facilitate early detection of adverse events (Box).6,7,8,9,10,11,12,13,14,15,16,17,18,19
Wearables are devices for continuously monitoring patients. The most popular are wrist‐worn accelerometers (sensors that detect movement), used for measuring aspects of fitness such as heart rate and counting steps, and health‐grade versions of such devices are in development. Monitoring patient movement patterns via use of accelerometers20 has the potential to detect the impact of medicines on sleep, daytime sedentary behaviour and daytime drowsiness, of which the latter can be a precursor to falls and motor vehicle or machinery accidents. Vital signs, including heart rate and respiratory rate, both of which can be affected by medicines, could also be monitored by digital technologies.21 Underwear that can detect incontinence events is being trialled, which may help identify medicines associated with incontinence.22 Wearables with voice recording are a potential mechanism for detecting medicine‐induced changes in cognition, with current research showing that machine learning can be used to process speech transcripts and recordings to identify changes in cognitive function.23 The application of digital technologies to adverse event prevention is currently limited. While there are studies demonstrating the value of wearable technologies for predicting falls in certain populations, such as people with dementia24 and diabetes,24 they are not yet being studied as methods for detecting and managing medicine‐induced adverse events in broader patient groups.
The evidence and barriers to adoption
While there is potential for medication management apps to help consumers adhere to their medication regimens, widespread adoption cannot yet be recommended. Current research provides limited evidence for their effectiveness. A 2018 review of smart technology to improve medication adherence in patients with cardiovascular disease found 47 studies evaluating phone calls and ten evaluating SMS, but only five evaluating web‐based tools and three evaluating apps.26 A 2015 systematic review evaluating the impact of mobile digital interventions on medication adherence included 27 randomised controlled trials. Of these, 15 showed statistically significant effects of digital interventions, two found mixed results and ten showed no differences.27 Another meta‐analysis of randomised clinical trials which assessed the effect of mobile telephone text messaging on medication adherence in chronic disease found a small to moderate effect size (Cohen d, 0.41; 95% CI, 0.23‐0.59).28 However, due to heterogeneous study methods and insufficient reporting, effect sizes are hard to precisely determine and tend to be smaller when more rigorous study designs are used.29
A research base that develops deeper, more comprehensive knowledge is required to encourage and guide practical applications of apps and wearables for medication management. Research to develop and assess medication management apps needs to be positioned within health services research that provides a basis for rigorous, mixed methods research to understand the process of user engagement with and use of apps,30 rather than clinical research that limits studies to randomised controlled designs that only assess effectiveness. Researchers in this field need to explore aspects of app design that affect adoption, such as cost, presence of advertisements, simplicity of language and required operating systems. They also need to consider aspects that affect ongoing use (adherence), such as types of reminders provided and tracking capacity. Other factors that may affect ongoing use, which should be studied, include the capacity to order repeat prescriptions, and the relevance of medicines information that is provided.
Lack of scientific evidence is not the only barrier to adoption. New technology must provide clear value if it is to be prescribed and used in clinical settings. This may be achieved by solving a particular problem for patients (eg, by providing reminders) or by improving data quality. One of the advantages of consumer‐directed apps with external tracking capacity where data can be shared with clinicians is that they foster social accountability. In the future, integration with existing health records (including personal health records such as My Health Record) could simplify data curation tasks and improve reliability.
Finally, as with many digital technologies, there may be concerns about safety and privacy of patient information. Currently, medication management apps are not considered medical devices in Australia and are not regulated by the Therapeutic Goods Administration. In the United States, the Food and Drug Administration (FDA) has taken a risk‐based approach, and placed most medication adherence apps in an intermediate category which “may meet the definition of medical device but for which the FDA will exercise enforcement discretion”.31 Future regulation needs to consider the delicate balance between innovation and safety, so technology improvements can be made available to the public in a safe and cost‐effective way.
Conclusion
Many innovations for improving medication management with consumer health technology are in development, but there are still significant challenges relating to adoption. Rigorous research and sound clinical judgement are needed to move consumer technology forward.
Provenance: Commissioned; externally peer reviewed.
- 1. Westbrook JI, Baysari MT. Nudging hospitals towards evidence‐based decision support for medication management. Med J Aust 2019; 210 (6 Suppl): S22‐S24.
- 2. Dayer LE, Shilling R, Van Valkenburg M, et al. Assessing the medication adherence app marketplace from the health professional and consumer vantage points. JMIR Mhealth Uhealth 2017; 5: e45.
- 3. Ahmed I, Ahmad NS, Ali S, et al. Medication adherence apps: review and content analysis. JMIR Mhealth Uhealth 2018; 6: e62.
- 4. Frias J, Virdi N, Raja P, et al. Effectiveness of digital medicines to improve clinical outcomes in patients with uncontrolled hypertension and type 2 diabetes: prospective, open‐label, cluster‐randomized pilot clinical trial. J Med Internet Res 2017; 19: e246.
- 5. Labovitz DL, Shafner L, Reyes Gil M, et al. Using artificial intelligence to reduce the risk of nonadherence in patients on anticoagulation therapy. Stroke 2017; 48: 1416–1419.
- 6. Dobkin BH. Wearable motion sensors to continuously measure real‐world physical activities. Curr Opin Neurol 2013; 26: 602–608.
- 7. Lee SP, Ha G, Wright DE, et al. Highly flexible, wearable, and disposable cardiac biosensors for remote and ambulatory monitoring. npj Digital Med 2018; 1: 2.
- 8. Tanaka A, Utsunomiya F, Douseki T. Wearable self‐powered diaper‐shaped urinary‐incontinence sensor suppressing response‐time variation with 0.3‐V start‐up converter. IEEE Sens J 2016; 16: 3472–3479.
- 9. Lyall LM, Wyse CA, Graham N, et al. Association of disrupted circadian rhythmicity with mood disorders, subjective wellbeing, and cognitive function: a cross‐sectional study of 91105 participants from the UK Biobank. Lancet Psychiatry 2018; 5: 507–514.
- 10. Abbasi J. Wearable digital thermometer improves fever detection. JAMA 2017; 318: 510.
- 11. Koh A, Kang D, Xue Y, et al. A soft, wearable microfluidic device for the capture, storage, and colorimetric sensing of sweat. Sci Transl Med 2016; 8: 366ra165.
- 12. He J, Choi W, Yang Y, et al. Detection of driver drowsiness using wearable devices: a feasibility study of the proximity sensor. Appl Ergon 2017; 65: 473–480.
- 13. Gold M, Amatniek J, Carrillo MC, et al. Digital technologies as biomarkers, clinical outcomes assessment, and recruitment tools in Alzheimer's disease clinical trials. Alzheimers Dement (N Y) 2018; 4: 234–242.
- 14. Guner D, Tiftikcioglu BI, Tuncay N, Zorlu Y. Contribution of quantitative EEG to the diagnosis of early cognitive impairment in patients with idiopathic Parkinson's disease. Clin EEG Neurosci 2017; 48: 348–354.
- 15. Meilan JJG, Martinez‐Sanchez F, Carro J, et al. Voice markers of lexical access in mild cognitive impairment and Alzheimer's disease. Curr Alzheimer Res 2018; 15: 111–119.
- 16. Gerbelot R, Koenig A, Goyer C, et al. A wireless patch for sleep respiratory disorders applications. Conf Proc IEEE Eng Med Biol Soc 2015; 2015: 2279–2282.
- 17. Rajagopalan R, Litvan I, Jung T‐P. Fall prediction and prevention systems: recent trends, challenges, and future research directions. Sensors (Basel) 2017; 17: 2509.
- 18. Saeb S, Zhang M, Karr CJ, et al. Mobile phone sensor correlates of depressive symptom severity in daily‐life behavior: an exploratory study. J Med Internet Res 2015; 17: e175.
- 19. Karydis T, Foster SL, Mershin A. Self‐calibrating protocols as diagnostic aids for personal medicine, neurological conditions and pain assessment. Proceedings of the 9th ACM International Conference on PErvasive Technologies Related to Assistive Environments; Corfu Island (Greece), June 29 – July 1, 2016. Article No. 61.
- 20. Gubelmann C, Heinzer R, Haba‐Rubio J, et al. Physical activity is associated with higher sleep efficiency in the general population: the CoLaus study. Sleep 2018; 41(7): zsy070.
- 21. Ge L, Zhang J, Wei J. Single‐frequency ultrasound‐based respiration rate estimation with smartphones. Comput Math Methods Med 2018; 2018: 3675974.
- 22. Long A, Edwards J, Worthington J, et al. Clinical evaluation of a prototype underwear designed to detect urine leakage from continence pads. J Wound Ostomy Continence Nurs 2015; 42: 632–639.
- 23. Toth L, Hoffmann I, Gosztolya G, et al. A speech recognition‐based solution for the automatic detection of mild cognitive impairment from spontaneous speech. Curr Alzheimer Res 2018; 15: 130–138.
- 24. Schwenk M, Hauer K, Zieschang T, et al. Sensor‐derived physical activity parameters can predict future falls in people with dementia. Gerontology 2014; 60: 483–492.
- 25. Najafi B, Armstrong DG, Mohler J. Novel wearable technology for assessing spontaneous daily physical activity and risk of falling in older adults with diabetes. J Diabetes Sci Technol 2013; 7: 1147–1160.
- 26. Treskes RW, Van der Velde ET, Schoones JW, Schalij MJ. Implementation of smart technology to improve medication adherence in patients with cardiovascular disease: is it effective? Expert review of medical devices. 2018; 15: 119–126.
- 27. Hamine S, Gerth‐Guyette E, Faulx D, et al. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res 2015; 17: e52.
- 28. Thakkar J, Kurup R, Laba TL, et al. Mobile telephone text messaging for medication adherence in chronic disease: a meta‐analysis. JAMA Intern Med 2016; 176: 340–349.
- 29. Pai ALH, McGrady M. Systematic review and meta‐analysis of psychological interventions to promote treatment adherence in children, adolescents, and young adults with chronic illness. J Pediatr Psychol 2014; 39: 918–931.
- 30. Gray K, Gilbert C. Digital health research methods and tools: suggestions and selected resources for researchers. In: Holmes DE, Jain LC, editors. Advances in biomedical informatics. Cham: Springer International Publishing, 2018: 5–34.
- 31. US Food and Drug Administration. Mobile medical applications 2015. https://www.fda.gov/MedicalDevices/DigitalHealth/MobileMedicalApplications/default.htm (viewed July 2018).





Elizabeth Roughead is supported by an NHMRC grant (APP 1110139).
Elizabeth Roughead is currently a member of the Digital Health Safety and Quality Governance Committee, an advisory committee of the Australian Digital Health Agency.