- The known: Pregabalin misuse is increasing worldwide, and is associated with acute psychiatric and medical harms, but patterns of pregabalin misuse in Australia have not been reported.
- The new: The rate of pregabalin‐related ambulance attendances has increased tenfold since 2012, associated with an increase in the national prescription rate. Patients frequently misused pregabalin with other sedatives, particularly benzodiazepines, and almost 40% of misuse‐related events requiring paramedic attendance were suicide attempts.
- The implications: Caution is required when prescribing pregabalin for patients using other sedatives. Misuse might be reduced by restricting dispensing of the drug.
Pregabalin is an anticonvulsant and central nervous system (CNS) depressant that was originally developed as an anti‐epileptic agent, but it is now also used to treat fibromyalgia, generalised anxiety disorder, and patients with neuropathic pain. In Australia, pregabalin prescribed as an anti‐epileptic is subsidised and also (since 2013) when prescribed for treating neuropathic pain. The number of prescriptions has risen dramatically since 2013, and by 2015 the total Pharmaceutical Benefits Scheme (PBS) costs for pregabalin were among the highest for any drug.1
Pregabalin misuse is increasing worldwide.2,3,4,5 Individuals take higher than recommended doses of pregabalin for its euphoric effects,4,6 whereby physical dependence has been reported,7 or for self‐harm.8 There is a growing black market for pregabalin in populations at high risk of misuse, including in prisons,9,10,11 where pregabalin is sometimes prescribed for pain relief in preference to opioids.9,12,13 Alcohol should not be consumed while taking pregabalin, and additive side effects are also possible if it is taken with other CNS depressants, including benzodiazepines and narcotic pain medications.7,14,15 Despite these recommendations, the number of reports about pregabalin being misused for recreational purposes in combination with sedatives, including alcohol, opioids, cannabis, and benzodiazepines, is increasing,2 and this concomitant use is associated with risks of respiratory depression16 and death.17
A recent meta‐analysis of risk factors for pregabalin misuse identified a history of substance misuse (particularly of opioids) and comorbid psychiatric conditions as important.4 Caution should be exercised when prescribing pregabalin for people with a history of psychiatric problems, as severe psychiatric side effects are possible, including mood changes, new or increased depression and anxiety, and new onset suicidal ideation and behaviour. The manufacturer's medication guide and other guidelines recommend that the patient should advise the prescribing doctor about previous depression, mood problems, suicidal thoughts or behaviour, and abuse of alcohol or other drugs, and that the physician should be alert to the development of these symptoms during treatment.2,14,15,18
In Australia, adverse event reporting to the Therapeutic Goods Administration (TGA) predominantly detects effects experienced by people to whom the drug has been appropriately prescribed and administered. It is notable that the number of pregabalin‐related adverse events reported to the TGA has declined since 2013 despite the dramatic increase in prescribing.19 However, adverse event recording systems are prone to underreporting;20 Coroners Court of Victoria data indicate that pregabalin‐related mortality has increased since 2013, and that pregabalin is now among the ten drugs most frequently implicated in overdose deaths in Victoria (unpublished document, Coroners Court of Victoria, August 2018).
We analysed ambulance attendance data to assess acute pregabalin‐related harms in the community. These data can help improve our understanding of the characteristics of people who experience acute harms because of pregabalin misuse, including their comorbid psychiatric conditions and concurrent use of alcohol or other CNS depressants and sedatives. Our specific aims were:
- to assess changes in the rates of ambulance attendances related to pregabalin misuse and to compare them with changes in prescribing rates;
- to characterise the patients attended by paramedics for pregabalin misuse‐related harms, including individuals with a history of drug misuse or psychiatric problems that may have contraindicated the prescribing of pregabalin;
- to assess the extent to which the misuse captured by ambulance attendance data is associated with misuse of other sedatives or with suicidal ideation and self‐harm; and
- to compare the characteristics of pregabalin misuse‐related ambulance attendances and harms for people who misuse pregabalin according to whether or not they also used other sedatives.
Methods
The Ambo Project
Data on pregabalin‐related ambulance attendances were collected for the Ambo Project, a collaboration between Turning Point and Ambulance Victoria. The Ambo Project collection and coding methods have been described previously.21,22 In brief, Ambulance Victoria provides Turning Point with data from the Victorian Ambulance Clinical Information System (VACIS), their electronic patient care record system. A filtered dataset of cases involving alcohol, other drugs, or mental health symptomology is provided to Turning Point, where a specialist team of research assistants employ a systematic and validated coding system to extract information from the clinical notes. The core criterion for determining whether alcohol or another drug was involved in a case was whether information in the clinical notes indicated that the immediately preceding or recent (not chronic) over‐ or inappropriate ingestion of the substance or medication was likely to have contributed significantly to the reason for the Ambulance Victoria attendance.
Pregabalin‐related ambulance attendances
All emergency ambulance attendances in Victoria (1 January 2012 – 31 December 2017; ie, the complete dataset available at the time of writing) in which pregabalin misuse was identified as a significant contributor to the attendance were included in our analysis. Pregabalin‐related ambulance attendances were defined as those in which a person prescribed pregabalin had consumed it too frequently or at higher than recommended amounts; a person had consumed pregabalin not prescribed to them; or a person had consumed pregabalin together with other substances that contributed to the ambulance attendance. Pregabalin misuse must have contributed significantly to the attendance, but other drugs or substances may also have been over‐ or inappropriately consumed. Our criteria specifically captured information about misuse‐related events, whereas adverse event reporting to the TGA captures data only for adverse events in people who have used a prescribed medication as directed.
Demographic information
For all pregabalin misuse‐related attendances, patient age (under 18, 18–29, 30–39, 40–49, 50–59, 60 or more years) and sex (male, female) were recorded. Prescribing of pregabalin for people less than 18 years of age is specifically contraindicated.14 Evidence of suicidal ideation or harms to self and concurrent misuse of other sedatives, as recorded by the attending paramedics, was also analysed. Police or prison custody and recent release from prison have been coded since 1 January 2013; we did not include these variables in our analysis of 2012 data.
Suicidality
The Ambo dataset allows differentiation of intent if suicidal thoughts or behaviours are recorded during the attendance. The attendance is coded as being an alcohol or other drug overdose (self‐poisoning); as a suicide modality (suicidal ideation or suicide attempt); an accidental overdose; or an overdose with unknown intent. We excluded cases of completed suicide (fewer than five) because this category is underrepresented in ambulance data; paramedics do not attend all deaths, and it may not be possible to determine intent or substance use when they do attend.
Concurrent sedative use
Concurrent misuse of pregabalin and other sedatives was defined as concomitant use of pregabalin at the time of the attendance and at least one other sedative (alcohol, cannabis, heroin, benzodiazepines, opioid analgesics, or methadone).
History of drug misuse or psychiatric problems
A history of drug misuse or psychiatric problems was defined by historical evidence of depression, self‐harm, suicidal ideation, suicide attempt, or alcohol or other drug misuse; these are problems that may have contraindicated pregabalin prescribing.
Statistical analysis
Changes over time were assessed by aggregating monthly ambulance attendance data into 6‐month blocks. Attendance data were not collected during October–December 2014 because of industrial action by paramedics; the July–December 2014 data therefore included only 3 months’ data. The most recently available monthly prescriptions data (July 2013 – October 2017) were obtained from the PBS Date of Supply report.23 This provides national‐ but not state‐level prescription data and does not detail the conditions for which pregabalin was prescribed. Monthly prescription data were aggregated into the same 6‐month blocks as the ambulance attendance data. Population rates were calculated using Australian Bureau of Statistics estimated resident population data, with the population applied at the end of each 6‐month interval.24
Relationships between categorical variables were analysed in Pearson χ2 tests. The relationship between prescription numbers and ambulance attendances was analysed with the Pearson correlation test. P < 0.05 was deemed statistically significant. Statistical analyses were conducted in Stata Statistical Software 13 (StataCorp).
Ethics approval
Ethics approval was obtained from the Eastern Health Human Research Ethics Committee (reference, E122‐0809).
Results
Numbers of pregabalin‐related ambulance attendances
Between 1 January 2012 and 31 December 2017 there were 1201 pregabalin misuse‐related ambulance attendances in Victoria. The 6‐monthly rate increased more than tenfold, from 0.28 cases per 100 000 population in the first half of 2012 to 3.32 cases per 100 000 in the second half of 2017 (Box 1). The pregabalin misuse‐related attendance rate was strongly correlated with the prescription rate in Australia (July 2013 – October 2017: r = 0.90; P = 0.001), with an 18.4% increase in ambulance attendances for each additional 100 000 prescriptions.
Demographic characteristics of patients
There was no sex difference in the numbers of pregabalin misuse‐related ambulance attendances (602 men [50.1%], 596 women [49.9%]). More than half the attendances were for people aged 30–49 years; by age group, the numbers of attendances were: under 18 years, 45 (3.7%); 18–29 years, 219 (18.2%); 30–39 years, 321 (26.7%); 40–49 years, 285 (23.7%), 50–59 years, 192 (16.0%); 60 years or more, 139 (11.6%). Of the 1201 attendances, 593 (49.3%) were for people who had a history of depression, self‐harm, suicidal ideation, suicide attempt, or misuse of alcohol or other drugs that may have contraindicated prescribing pregabalin. Of the five pre‐existing conditions that contributed to such histories, the most frequent were a history of depression (485 patients, 40.4%) or a suicide attempt (195, 16.2%). A small number of pregabalin misuse‐related attendances were for people in police or prison custody (15, 1.2%) or who had recently been released from prison (10, 0.8%).
Concurrent sedative use and self‐harming behaviours
Concurrent use of other sedatives and suicide attempts were frequently recorded during pregabalin misuse‐related attendances (Box 2). In 812 pregabalin misuse‐related attendances (67.6%), patients had used pregabalin together with at least one other sedative. A total of 187 attendances (15.6%) were for people who had attempted suicide and concurrently used pregabalin and benzodiazepines, 147 (12.2%) for people who had attempted suicide and concurrently used pregabalin and alcohol, and 121 (10.1%) for people who had attempted suicide and concurrently used pregabalin and opioid analgesics.
Features of pregabalin‐related ambulance attendances for people misusing both pregabalin and other sedatives
The characteristics of patients who had misused pregabalin differed according to whether they had also taken another sedative (Box 3). A greater proportion of attendances for men than for women involved concurrent misuse of pregabalin and other sedatives (54% v 46%); a higher proportion of patients who had missed pregabalin and another sedative presented with a Glasgow Coma Scale score below 13 (23% v 12% for pregabalin misuse alone). However, the proportions of patients with current suicidal ideation or harms to self were similar whether patients had also used other sedatives or not.
Discussion
The rate of pregabalin‐related ambulance attendances in Victoria has dramatically increased since 2012, parallel with increases in prescribing rates. This finding is consistent with those of other investigations of pregabalin‐related mortality,17 but may also reflect increasing levels of prescription drug misuse25 or a shift toward pregabalin misuse by people who misuse other drugs. In any case, the increased availability of pregabalin affords more opportunities for its misuse.
The age and sex distribution of the patients seen in pregabalin‐related ambulance attendances were similar to those for people who misuse other pharmaceuticals in Australia.25 However, it is worrying that almost half the pregabalin misuse‐related attendances were for people with a history of drug misuse or psychiatric problems that may have contraindicated its prescription (history of depression, self‐harm, suicidal ideation, suicide attempt, misuse of alcohol or other drugs). As the source of pregabalin was not recorded, we could not determine in individual cases whether the drug was obtained on prescription or by diversion or other illegal means. Nevertheless, our findings suggest that there is a group of people who are likely to misuse pregabalin and may be at risk of its undesirable psychiatric side effects. Clinicians should carefully review the indications for prescribing pregabalin and remind patients that it is illegal to give their medications to other people.
There was considerable overlap between pregabalin‐related attendances in which a suicide attempt was recorded or the concurrent use of another sedative (most frequently, benzodiazepines) was noted. Concurrent use with other sedatives was more frequent for men and patients aged 30–59 years, but the proportions of patients with a history of drug misuse or psychiatric problems were similar whether another sedative was used or not. The proportion of patients with Glasgow Coma Scale scores below 13 (ie, moderate or more severe brain injury) was higher for those who combined pregabalin with another sedative, but the frequencies of current suicidal ideation or harms to self were similar in both groups. Collectively, these findings suggest that people who misuse pregabalin while taking other sedatives are at greater risk of medical harms than those who misuse it alone, but are at no greater risk of acute psychiatric harms.
The Ambo dataset records information about patients attended by an ambulance, and data collection ends at the point when paramedics either treat the individual or transport them to further care; that is, final clinical outcomes are not captured. The trajectory and clinical outcomes of those with pregabalin‐related ambulance attendances should be further explored by linking ambulance attendance data with other datasets (eg, emergency department and hospital admissions data).
Pregabalin misuse was frequently combined with misuse of benzodiazepines, alcohol, or opioid analgesics. Pregabalin is sometimes prescribed off‐label for tapering benzodiazepine therapy for people with generalised anxiety disorder,26 but the combination of pregabalin and benzodiazepines can also elicit a particularly desirable euphoria,27making it attractive for recreational users. The concurrent misuse of pregabalin and opioid analgesics entails specific risks, particularly depression of CNS and respiratory function,14 increasing opioid‐related mortality risk by as much as 68%.28 Clinicians should ensure that consumers are aware of the risks of these interactions, and be particularly cautious when considering prescribing pregabalin for patients who are taking other sedatives. They should also direct patients to the NPS MedicineWise guidelines on how to safely take pregabalin.29
Limitations
Our study was limited by our analysing secondary data collected for operational purposes, as collection and coding biases and incomplete or inconsistent recording of variables are possible. Further, ambulances do not attend all suicides, so that suicide is underrepresented in the Ambo dataset; consequently, the contribution of pregabalin misuse to suicide in Victoria could not be determined, as this would require analyses of, for instance, coronial data. The involvement of a substance in the reason for an ambulance attendance is determined from information provided by the patient, others at the scene, or the paramedics’ clinical observations and assessment, not from toxicology testing. A patient's history of drug misuse and psychiatric problems is determined in a similar manner. Further, the Ambo data referred to ambulance attendances in Victoria, whereas pregabalin prescription data were collated nationally and may therefore not reflect state‐based prescribing patterns. Finally, we analysed data for publicly funded PBS prescriptions, not privately purchased pregabalin; any resulting underestimation of rates, however, is likely to be minor because of the high cost of private prescriptions.
Conclusion
We found that pregabalin misuse as reflected in data for ambulance attendances has increased dramatically in Victoria over the past 6 years, that a large of proportion of people who misuse pregabalin and require paramedic assistance concurrently use other sedatives, and that pregabalin misuse is associated with acute psychiatric and medical harms. Our study was based on unique information about the acute harms resulting from pregabalin misuse that is not available from other sources, providing detailed insights into the context of pregabalin misuse and the characteristics of pregabalin‐related ambulance attendances. Our novel, Australian‐specific findings can guide clinical practice and pregabalin prescribing, meeting the acute care needs of patients during an ambulance attendance related to pregabalin misuse, and regulatory programs such as real time prescription monitoring in Victoria by SafeScript (https://www2.health.vic.gov.au/safescript). Our findings are consistent with overseas reports on trends in pregabalin misuse, and interventions being considered in other countries may be relevant to Australia, including changes to scheduling, as implemented or planned in the United Kingdom, the United States and Norway, and limits on dispensing to minimise the risks of pregabalin misuse.
Box 1 – Pregabalin misuse‐related ambulance attendances (Victoria) and pregabalin prescriptions (Australia), 2012–2017, by 6‐month period
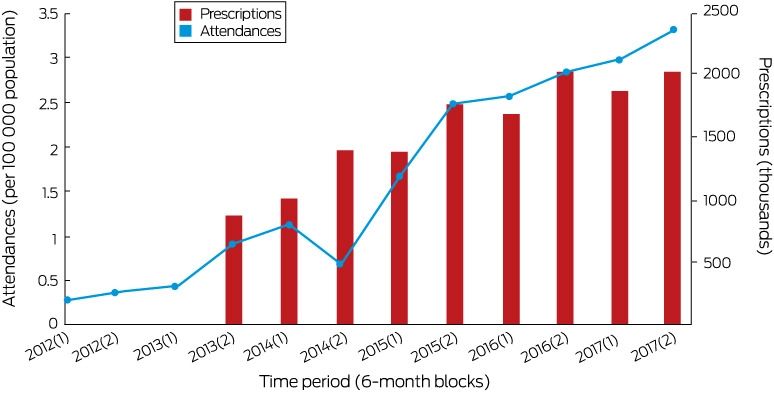
* Because of industrial action by paramedics during October–December 2014, only 3 months’ attendance data are available for the period July–December 2014. [Correction added on 11 December 2018, after first online publication: The axes on the graph were incorrectly labelled and have been corrected. The changes do not influence the interpretation of the results.]
Box 2 – Other sedative use, current suicidal ideation, and harms to self for patients in 1201 pregabalin misuse‐related ambulance attendances in Victoria, 2012–2017
|
|
Number* |
||||||||||||||
|
|
|||||||||||||||
|
Total number of pregabalin misuse‐related attendances |
1201 |
||||||||||||||
|
Concurrent consumption of other sedatives: any |
812 (67.6%) |
||||||||||||||
|
Benzodiazepines |
440 (36.6%) |
||||||||||||||
|
Alcohol |
321 (26.7%) |
||||||||||||||
|
Opioid analgesics |
254 (21.1%) |
||||||||||||||
|
Heroin |
100 (8.3%) |
||||||||||||||
|
Methadone |
53 (4.4%) |
||||||||||||||
|
Cannabis |
43 (3.6%) |
||||||||||||||
|
None |
389 (32.4%) |
||||||||||||||
|
Current suicidal ideation or harms to self |
|||||||||||||||
|
Suicide attempt |
472 (39.3%) |
||||||||||||||
|
Suicidal ideation |
22 (1.8%) |
||||||||||||||
|
Self‐injury |
19 (1.6%) |
||||||||||||||
|
Self‐injury threat |
0 |
||||||||||||||
|
Nature of overdose |
|||||||||||||||
|
Alcohol or drug overdose as a suicide modality |
478 (39.8%) |
||||||||||||||
|
Accidental overdose |
81 (6.7%) |
||||||||||||||
|
Intent unknown |
253 (21.1%) |
||||||||||||||
|
|
|||||||||||||||
|
Multiple sedatives or behaviours may have been involved in individual attendances. |
|||||||||||||||
Box 3 – Characteristics of patients in 1201 pregabalin‐related ambulance attendances in Victoria, 2012–2017, by concurrent use of other sedatives
|
|
Pregabalin misuse |
P |
|||||||||||||
|
Without other sedatives |
With other sedatives |
||||||||||||||
|
|
|||||||||||||||
|
Total |
389 |
812 |
|
||||||||||||
|
Sex |
|
|
< 0.001 |
||||||||||||
|
Men |
165 (42.4%) |
437 (53.8%) |
|
||||||||||||
|
Women |
221 (56.8%) |
375 (46.2%) |
|
||||||||||||
|
Age (years) |
|
|
< 0.001 |
||||||||||||
|
Under 18 |
32 (8.2%) |
13 (1.6%) |
|
||||||||||||
|
18–29 |
64 (16.5%) |
155 (19.1%) |
|
||||||||||||
|
30–39 |
96 (24.7%) |
225 (27.7%) |
|
||||||||||||
|
40–49 |
87 (22.4%) |
198 (24.4%) |
|
||||||||||||
|
50–59 |
43 (11.1%) |
149 (18.3%) |
|
||||||||||||
|
60 or more |
67 (17.2%) |
72 (8.9%) |
|
||||||||||||
|
History of drug misuse or psychiatric problems* |
|
|
0.06 |
||||||||||||
|
Absent |
212 (54.5%) |
396 (48.8%) |
|
||||||||||||
|
Present |
177 (45.5%) |
416 (51.2%) |
|
||||||||||||
|
Physical presentation |
|||||||||||||||
|
Glasgow Coma Scale score < 13 |
47 (12%) |
185 (22.8%) |
< 0.001 |
||||||||||||
|
Outcome |
|||||||||||||||
|
Transported to hospital |
341 (87.7%) |
728 (89.7%) |
0.30 |
||||||||||||
|
Current suicidal ideation or harms to self |
|||||||||||||||
|
Suicide attempt |
157 (40.4%) |
315 (38.8%) |
0.60 |
||||||||||||
|
Self‐injury |
7 (2%) |
12 (1.5%) |
0.68 |
||||||||||||
|
Suicidal ideation |
6 (2%) |
16 (2.0%) |
0.60 |
||||||||||||
|
|
|||||||||||||||
|
Multiple sedatives or behaviours may have been involved in individual attendances. *History of depression, self‐harm, suicidal ideation, suicide attempt, or misuse of alcohol or other drugs. |
|||||||||||||||
Received 10 April 2018, accepted 11 July 2018
- Rose Crossin1
- Debbie Scott1
- Shalini Arunogiri1
- Karen Smith2
- Paul M Dietze3
- Dan I Lubman1
- 1 Turning Point Alcohol and Drug Centre, Eastern Health Clinical School, Monash University, Melbourne, VIC
- 2 Ambulance Service of Victoria, Melbourne, VIC
- 3 Centre for Epidemiology and Population Health Research, Burnet Institute, Melbourne, VIC
This study was funded by the Victorian Department of Health and Human Services as part of the Ambo Project. Funding bodies had no involvement in the decision to publish this study, and researchers are independent of the funder. Paul Dietze is a National Health and Medical Research Council Research Fellow (117291).
Paul Dietze has received investigator‐driven funding from Gilead Sciences for hepatitis C studies and an untied educational grant from Indivior unrelated to this investigation. He has served as an unpaid member on a Mundipharma advisory board for an intranasal naloxone product. These funders had no input into any aspect of this study.
- 1. Mabbott V, Storey P. Australian statistics on medicines 2015. Canberra: Pharmaceutical Benefits Division, 2016. http://www.pbs.gov.au/info/statistics/asm/asm-2015 (viewed Oct 2018).
- 2. Schifano F. Misuse and abuse of pregabalin and gabapentin: cause for concern? CNS Drugs 2014; 28: 491–496.
- 3. Gahr M, Freudenmann RW, Hiemke C, et al. Pregabalin abuse and dependence in Germany: results from a database query. Eur J Clin Pharmacol 2013; 69: 1335–1342.
- 4. Evoy KE, Morrison MD, Saklad SR. Abuse and misuse of pregabalin and gabapentin. Drugs 2017; 77: 403–426.
- 5. Cairns R, Schaffer AL, Ryan N, et al. Rising pregabalin use and misuse in Australia: trends in utilization and intentional poisonings. Addiction 2018; https://doi.org/10.1111/add.14412 [Epub ahead of print].
- 6. Bonnet U, Scherbaum N. How addictive are gabapentin and pregabalin? A systematic review. Eur Neuropsychopharmacol 2017; 27: 1185–1215.
- 7. Pfizer. Lyrica (pregabalin) prescribing information and medication guide 2016. Revised Dec 2016. http://labeling.pfizer.com/showlabeling.aspx?id=561#S9 (viewed Oct 2018).
- 8. Daly C, Griffin E, Ashcroft DM, et al. Intentional drug overdose involving pregabalin and gabapentin: findings from the National Self‐Harm Registry Ireland, 2007–2015. Clin Drug Investig 2018; 38: 373–380.
- 9. Bicknell M. The pain of pregabalin prescribing in prisons. Br J Gen Pract 2013; 63: 405.
- 10. Morrison E, Sandilands E, Webb D. Gabapentin and pregabalin: do the benefits outweigh the harms? J Royal Coll Physicians Edinb 2017; 47: 310–313.
- 11. Spence D. Bad medicine: gabapentin and pregabalin. BMJ 2013; 347: f6747.
- 12. Goodman CW, Brett AS. Gabapentin and pregabalin for pain — is increased prescribing a cause for concern? N Engl J Med 2017; 377: 411–414.
- 13. Lawson E. Lesser‐known prescribed and over‐the‐counter drugs of misuse. Prescriber 2011; 22(21): 12–17.
- 14. Pfizer. Lyrica (pregabalin) medication guide. Updated Dec 2013. https://www.fda.gov/downloads/Drugs/DrugSafety/UCM152825.pdf (viewed Oct 2018).
- 15. Public Health England. Advice for prescribers on the risk of the misuse of pregabalin and gabapentin (PHE publications gateway no. 2014586; NHS England publications gateway no. 02387). Dec 2014. https://www.gov.uk/government/publications/pregabalin-and-gabapentin-advice-for-prescribers-on-the-risk-of-misuse (viewed Oct 2018).
- 16. Lyndon A, Audrey S, Wells C, et al. Risk to heroin users of polydrug use of pregabalin or gabapentin. Addiction 2017; 112: 1580–1589.
- 17. Häkkinen M, Vuori E, Kalso E, et al. Profiles of pregabalin and gabapentin abuse by postmortem toxicology. Forensic Sci Int 2014; 241: 1–6.
- 18. NPS MedicineWise. Pregabalin (Lyrica) for neuropathic pain. Radar [website]; 4 Apr 2013. https://www.nps.org.au/radar/articles/pregabalin-lyrica-for-neuropathic-pain (viewed Oct 2018).
- 19. Therapeutic Goods Administration. Database of adverse event notifications (DAEN). 19 July 2018. https://www.tga.gov.au/database-adverse-event-notifications-daen (viewed Oct 2018).
- 20. Hazell L, Shakir SA. Under‐reporting of adverse drug reactions. Drug Saf 2006; 29: 385–396.
- 21. Lloyd BK, McElwee P. Trends over time in characteristics of pharmaceutical drug‐related ambulance attendances in Melbourne. Drug Alcohol Rev 2011; 30: 271–280.
- 22. Dietze P, Cvetkovski S, Rumbold G, Miller P. Non‐fatal heroin overdose in Melbourne: establishment and analysis of a database of ambulance service records. Drug Alcohol Rev 2000; 19: 27–33.
- 23. Pharmaceutical Benefits Scheme and Repatriation Pharmaceutical Benefits Scheme. Section 85 Supply Data. Updated June 2018. http://www.pbs.gov.au/info/statistics/dos-and-dop/dos-and-dop (viewed June 2018).
- 24. Australian Bureau of Statistics. 3101.0. Australian demographic statistics, Mar 2018. Sept 2018. http://www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 (viewed Oct 2018).
- 25. Australian Institute of Health and Welfare. National Drug Strategy Household Survey (NDSHS) 2016 — detailed findings (Cat. No. PHE 214). Canberra: Australian Institute of Health and Welfare, 2017.
- 26. Hadley SJ, Mandel FS, Schweizer E. Switching from long‐term benzodiazepine therapy to pregabalin in patients with generalized anxiety disorder: a double‐blind, placebo‐controlled trial. J Psychopharmacol 2012; 26: 461–470.
- 27. Schifano F, D'Offizi S, Piccione M, et al. Is there a recreational misuse potential for pregabalin? Analysis of anecdotal online reports in comparison with related gabapentin and clonazepam data. Psychother Psychosom 2011; 80: 118–122.
- 28. Gomes T, Greaves S, van den Brink W, et al. Pregabalin and the risk for opioid‐related death: a nested case–control study. Ann Intern Med 2018; https://doi.org/10.7326/m18-1136.
- 29. NPS MedicineWise. Pregabalin for nerve pain. Jan 2018. https://www.nps.org.au/medical-info/consumer-info/pregabalin-for-nerve-pain (viewed Oct 2018).





Abstract
Objective: To compare changes in pregabalin prescribing and misuse‐related ambulance attendances; to characterise the patients attended by paramedics for pregabalin misuse‐related harms; to assess the association of pregabalin misuse with use of other sedatives and with suicidal ideation and self‐harm; to compare the characteristics of pregabalin misuse‐related harms in people who misuse pregabalin according to whether or not they also used other sedatives.
Design, setting, participants: Retrospective analysis of data on ambulance attendances in Victoria, January 2012 – December 2017, for which pregabalin misuse‐related harms were a contributing factor.
Main outcome measures: Rates of pregabalin misuse‐related ambulance attendances, pregabalin prescription rates (each 6‐monthly); patient characteristics, including age, sex, history of drug misuse or psychiatric problems, concurrent use of other sedatives, and current suicidal ideation and self‐harm.
Results: There were 1201 pregabalin misuse‐related attendances during the study period; the rate increased from 0.28 cases per 100 000 population in the first half of 2012 to 3.32 cases per 100 000 in the second half of 2017. The attendance rate was strongly correlated with prescription rates in Australia (r = 0.90; P = 0.001). 593 attendances (49%) were for people with a history that may have contraindicated prescribing pregabalin. Pregabalin was frequently misused with other sedatives (812 attendances, 68%), particularly benzodiazepines (440, 37%); 472 attendances (39%) were associated with suicide attempts. People who misused pregabalin with other sedatives more frequently presented with moderate to severe impairments of consciousness, but the frequency of suicide attempts was similar whether other sedatives were concurrently used or not.
Conclusions: Rates of pregabalin misuse‐related ambulance attendances in Victoria have increased markedly over the past 6 years. Caution is required when prescribing pregabalin for people taking other sedatives. Limiting the dispensing of this drug may reduce the risks associated with its misuse.