The known Laparoscopic appendicectomy is increasingly preferred to open appendicectomy for managing appendicitis in children. The most recent systematic review of their outcomes was published in 2012.
The new Children with uncomplicated appendicitis have a lower risk of post-operative bowel obstruction after laparoscopic appendicectomy than after open appendicectomy, but their higher re-admission rates suggest that they may be discharged before post-operative symptoms have adequately resolved. Post-appendicectomy outcomes were similar for most age groups and hospital types.
The implications Undertaking appendicectomies in children outside tertiary paediatric hospitals is safe, and reduces waiting times, delays in care, and unnecessary travel for their families.
Acute appendicitis is one of the most common paediatric health emergencies requiring surgery, affecting about one in 800 children.1 Until the advent of laparoscopic surgery in the 1980s, the operation traditionally involved the classic McBurney muscle-splitting incision.2 Laparoscopic appendicectomy has since become the most common surgical technique for treating acute appendicitis in children.3 This shift in practice has been attributed to shorter lengths of hospital stay, earlier return to normal function, and a better cosmetic appearance.4 However, whether the post-operative outcomes of laparoscopic appendicectomy are equivalent to those of traditional open appendicectomy is still debated, particularly in cases of complicated appendicitis.
A 2012 systematic review found no difference in the post-operative complication rates of laparoscopic and open appendicectomy in uncomplicated cases of appendicitis in children; for complicated appendicitis, the risk of post-operative wound infections was 58% lower after laparoscopic appendicectomy, but the risk of intra-abdominal abscess was 30% higher.5 The influence of changing surgical management and the effects of characteristics such as age, type of hospital, and inter-hospital transfers on post-operative outcomes have not been comprehensively evaluated during the past decade. Up-to-date population-based information on outcomes is important for informing clinical decision making, resource allocation, and health policy on paediatric health care. The aim of our study was to assess and compare the post-operative outcomes of open and laparoscopic appendicectomy in children.
Materials and methods
We analysed data for all children under 16 years of age who underwent appendicectomy for appendicitis in New South Wales between January 2002 and December 2013. Children with a diagnosis of abdominal pain, intestinal congenital anomalies, obstructive diseases, injuries, or intestinal conditions were excluded.
Data sources
NSW Admitted Patient Data Collection (APDC) and Emergency Department Data Collection (EDDC) records were probabilistically linked by the NSW Centre for Health Record Linkage (www.cherel.org.au) and de-identified data were provided to the investigators. The APDC is a census of all inpatient admissions to public and private hospitals; it includes patient demographic information and relevant diagnoses and procedures for each admission, respectively coded according to the International Classification of Diseases, tenth revision, Australian modification (ICD-10-AM) and the Australian Classification of Health Interventions (ACHI). The EDDC is a statutory collection of data for all presentations to emergency departments in NSW public hospitals, and includes information on patient symptoms or diagnoses coded according to the International Classification of Diseases, ninth revision, clinical modification (ICD-9-CM), ICD-10-AM, and SNOMED-CT.
Cases of appendicitis were classified as either uncomplicated or complicated (with peritonitis, rupture or abscess). The relevant diagnosis and procedure codes are listed in the online Appendix, table 1. Clinical outcomes assessed in our study were length of hospital stay, complications recorded during the initial admission, hospital re-admissions, and emergency department re-presentations within 28 days of discharge that did not require hospitalisation. Post-operative complications during the initial admission were defined as intestinal obstruction, intra-abdominal abscess, respiratory complications, complications affecting other systems (nervous, circulatory, endocrine, unspecified), adverse effects of therapeutic drugs, and wound infections. Re-admission to hospital for complications was distinguished from other re-admissions, and included re-admission for symptomatic conditions (abdominal pain, nausea, vomiting). Re-presentations to an emergency department by patients with post-operative gastrointestinal symptoms (gastroenteritis, abdominal pain) or wound infections within 28 days of discharge were identified. Composite outcomes (intestinal obstruction, intra-abdominal abscess, wound infection, any post-operative complication) were also examined separately for initial admission and within 28 days of discharge.
Explanatory variables assessed included characteristics of the patient and the operation: type of appendicitis (uncomplicated, complicated), age, sex, socio-economic disadvantage (Index of Relative Socio-economic Disadvantage),6 secondary intra-abdominal diagnosis at initial admission, pre-existing conditions, type of hospital, transfers from another hospital, and day (weekday v weekend), season, and period of surgery (2002–2005, 2006–2009, 2010–2013).
Statistical analysis
The population trends in age-specific rates of appendicectomy (population data were obtained from the Australian Bureau of Statistics7) and the proportion of laparoscopic appendicectomies in the study population were evaluated by hospital type and broad age groups (under 9 v 9–15 years of age). The overall trend in inter-hospital transfers was assessed in Cochran–Armitage tests. Patient and operation characteristics were summarised in contingency tables. The associations between appendicectomy type and post-operative outcomes during the initial admission and within 28 days of discharge were assessed in χ2 tests, stratified by appendicitis type (uncomplicated, complicated). Stratification was applied to univariate and multivariate analyses using binary generalised estimating equations with a logit link and exchangeable correlation to estimate the odds of intestinal obstruction, intra-abdominal abscess, wound infections, and any post-operative complications after laparoscopic and open appendicectomy, corrected for patient and operation characteristics and clustering within individual hospitals. We also conducted a sensitivity analysis for the multivariate analysis of complicated appendicitis by excluding patients with diagnoses of acute appendicitis with localised peritonitis (ICD-10-AM, K35.3); this code was introduced during the study period (in 2009). P < 0.05 was deemed statistically significant. All analyses were conducted in SAS 9.4 (SAS Institute).
Ethics approval
Ethics approval for data access was obtained from the NSW Population and Health Services Research Ethics Committee (reference, 2012-12-430).
Results
During 2002–2013, 23 961 children under 16 underwent appendicectomy for appendicitis in NSW, a population prevalence of 14 cases per 10 000 children under 16 years of age. Prevalence increased with age: one case per 10 000 children aged 0–4 years, eight cases per 100 000 children aged 5–8 years, and 23 cases per children aged 9–11 years. A total of 19 336 patients (81%) had diagnoses of uncomplicated appendicitis; 4625 cases (19%) were complicated by abscess, perforation or peritonitis. The proportion of uncomplicated cases increased with age (0–4 years, 42%; 5–8 years, 72%; 9–11 years, 82%; 12–15 years, 85%).
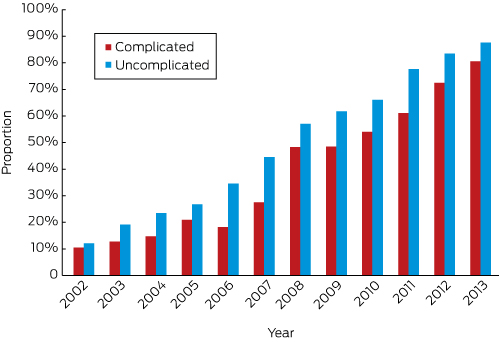
During the study period, open appendicectomy was undertaken in 12 300 children (51%), and laparoscopic appendicectomy in 11 661 (49%), but the proportion of laparoscopic appendicectomies rose from 11.8% in 2002 to 85.8% in 2013 (for trend, P < 0.001), with similar increases for uncomplicated and complicated appendicitis (Box 1) and in all age groups (online Appendix, figure 1A).
The proportion of laparoscopic appendicectomies increased with the age of the children (2002–2013: 0–4 years, 28%; 12–15 years, 56%); it was greater for children from the most disadvantaged backgrounds than for those from the most advantaged (57% v 45%), and greater for girls than boys (55% v 44%) (Box 2). The increased use of laparoscopic appendicectomy for both complicated and uncomplicated appendicitis applied to all hospital types (for trend, P < 0.001); in 2013, it was employed by tertiary paediatric, metropolitan and private hospitals in more than 90% of cases, and in 71% of cases in regional and rural hospitals (online Appendix, figure 1B).
A total of 2888 children (12% of cases) were transferred from the initial presenting hospital, most frequently to tertiary paediatric or regional hospitals. The proportion of children under 9 years of age transferred to tertiary paediatric hospitals increased until 2010, after which it declined; there were no consistent trends for transfers to other hospital types or for older children (online Appendix, figures 2A and B).
Open appendicectomy was associated with longer hospital stays than laparoscopic appendicectomy; 56% of children with complicated appendicitis who underwent open appendicectomy stayed for more than 5 days, compared with 46% of those who underwent laparoscopic appendicectomy (Box 3). For all children undergoing appendicectomy, the proportion staying for longer than 5 days decreased with age: 0–4 years, 57% (392 children); 5–8 years, 22% (784 children); 9–11 years, 14% (1053 children); 12–15 years, 13% (1612 children) (for trend, P < 0.001).
Uncomplicated appendicitis
For children with uncomplicated appendicitis, the post-operative complication rate after laparoscopic appendicectomy was higher than for open appendicectomy (7.4% v 5.8%), chiefly because the rates of re-admission (5.0% v 4.1%) and re-presentation to EDs were higher (4.6% v. 3.0%) (Box 3).
Children under 9 years of age were more likely to have a complication than those aged 12–15 years; those with pre-existing conditions or co-existing intra-abdominal diagnoses at time of operation were more likely to have complications than those who did not. After adjusting for patient and surgery factors, there was no association between type of operation and having any post-operative complications (laparoscopic v open appendicectomy: adjusted odds ratio [aOR)], 1.13; 95% confidence interval [CI], 0.98–1.30) (online Appendix, table 4).
Laparoscopic appendicectomy was associated with lower odds of intestinal obstruction (aOR, 0.59; 95% CI, 0.36–0.97), but not of intra-abdominal abscess or wound infections (Box 4).
Complicated appendicitis
In cases of complicated appendicitis, post-operative complications were more frequent following open appendicectomy (22.9% v 18.8%). There was no difference in the overall frequency of complications during the initial admission, but open appendicectomy was associated with more respiratory complications and wound infections. Re-admission within 28 days of discharge was more frequent following open appendicectomy (12.5% v 9.5%), particularly because of intra-abdominal abscess and wound infections (Box 3).
The odds of any post-operative complication (aOR, 0.78; 95% CI, 0.68–0.90) (online Appendix, table 5) and of wound infections (aOR, 0.55; 95% CI, 0.44–0.69) were lower for laparoscopic appendicectomy, but there was no association between the type of operation and intestinal obstruction or intra-abdominal abscess (Box 4). After excluding 1674 cases with localised peritonitis, there was no association between type of operation and any post-operative complication (aOR, 0.98; 95% CI, 0.83–1.16), intestinal obstruction (aOR, 0.97; 95% CI, 0.62–1.52), or intra-abdominal abscess (aOR, 1.06; 95% CI, 0.72–1.55); the odds of wound infection following laparoscopic appendicectomy were lower (aOR, 0.67; 95% CI: 0.50–0.90).
Discussion
We found that laparoscopic appendicectomies as a proportion of all appendicectomies in children with uncomplicated or complicated appendicitis rose markedly during 2002–2013. In general, outcomes were similar for laparoscopic and open appendicectomy, and the overall complication rates were also similar for most age groups and hospital types. However, children with uncomplicated appendicitis undergoing laparoscopic appendicectomy were more likely to be re-admitted to hospital or to re-present to an emergency department with symptoms of abdominal pain or fever, although less likely to have post-operative intestinal obstruction. For complicated appendicitis, laparoscopic appendicectomy was associated with reduced odds of wound infection.
During the past 20 years, laparoscopic appendicectomy has become the standard procedure for treating acute appendicitis in children.4 Our finding that 86% of cases were managed with laparoscopic appendicectomy in 2013 is similar to reported rates in the United States (2010, 90%)8 and the Netherlands (2010, 94%),9 and higher than in Germany (2010–2012, 76%),10 Canada (2010, 66%)11 and Taiwan (2012, 57%).12
The post-operative outcome rates we report are only partially consistent with the findings of the most recent relevant systematic review, which pooled the results of 19 studies (2000–2011) encompassing 107 000 children.5 For children with uncomplicated appendicitis, the authors of the systematic review found no differences between the two operation types with regard to the overall incidence of post-surgery complications and the odds of intestinal obstruction.5 The differing findings regarding the latter might reflect different definitions of bowel obstruction and different levels of follow-up. An earlier meta-analysis found a 50% reduced risk of bowel obstruction after laparoscopic appendicectomy in children.13
The 2012 review also found that laparoscopic appendicectomy was associated with shorter hospital lengths of stay for both uncomplicated and complicated appendicitis.5 We found similar results for the initial admission, but we also found a higher re-presentation rate following laparoscopic appendicectomy for uncomplicated appendicitis. It is possible that children undergoing laparoscopic appendicectomy recover more slowly than is recognised, and that the discomfort of laparoscopy may take time to subside.14 Children have smaller abdominal cavities than adults, and insufflation with carbon dioxide is often required for a laparoscopic appendicectomy; the additional stretching of the anterior abdominal wall and diaphragm can cause post-operative discomfort. It is also possible that the perceived advantages of laparoscopic appendicectomy for recovery may not apply to children. The balance between early discharge and increased rates of re-admission and re-presentation should be more comprehensively evaluated — including consideration of post-operative outcomes and pain management, discharge criteria, and post-discharge care and health costs — in order to optimise the initial admission length of stay while reducing the likelihood of re-presentation.
For children with complicated appendicitis, our findings are consistent with those of the 2012 systematic review, which reported a lower overall risk of complications and of wound infections after laparoscopic appendicectomy.5 A recent German population-based study of 8110 patients also reported that the risk of re-admission for complications was reduced after laparoscopic appendicectomy.10 We found no association between surgical technique and intra-abdominal abscess, and the findings of other studies have been inconsistent,5,9,12 perhaps because of differences in peri-operative management, surgical technique, and the reporting of intra-abdominal abscess. This is highlighted by the results of our sensitivity analysis: after cases of appendicitis with localised peritonitis (milder complicated cases) were excluded, differences in the odds of post-operative complications between open and laparoscopic appendicectomy were no longer evident. This supports the interpretation that lower rates of post-operative complications after laparoscopic appendicectomy are explained by case selection, as complex cases are more likely to proceed to open appendicectomy. Similarly, the reduced likelihood of complications for children undergoing appendicectomy in private hospitals may also reflect the lower complexity of their cases.
We found that the outcomes for children managed in metropolitan, regional or rural general hospitals were not different from those for children who were treated in tertiary paediatric hospitals, regardless of age. This is consistent with findings of similar post-surgery outcomes for high, medium and low volume children’s hospitals in California.3 Another Californian study found no effect of age on post-operative wound infection and intra-abdominal abscess rates following complicated and uncomplicated appendicitis.15
Our results have important implications for managing emergency surgery for children. During the middle of the first decade of this century, children in NSW with non-complex emergency surgical conditions, such as appendicitis, were often transferred from metropolitan general hospitals to tertiary paediatric hospitals.16,17 In response to this problem, a statewide paediatric surgery framework was proposed in 200818 and adopted in 2014.19 The framework aimed to facilitate the care of children with non-complex emergency surgical conditions at metropolitan general hospitals, reducing waiting times, delays in appropriate care, and unnecessary travel or hospital transfers for the families of children who required an appendicectomy. We found an encouraging reduction in the proportion of children transferred to paediatric tertiary hospitals since 2010, which suggests a positive response to this framework by non-paediatric hospitals. Our findings indicate that the framework is safe, supporting the recommendation to further lower the age threshold at non-paediatric hospitals to 8 years.
The main strength of our study is its analysis of large, record-linked population-based datasets, providing robust and generalisable results. This is the first investigation of post-appendicectomy presentations to emergency departments. One limitation is that we did not have pathology information that confirmed the diagnosis of appendicitis; however, we restricted our analysis to children with a primary diagnosis of appendicitis to mitigate this potential bias. Further, we did not have information about whether appendicectomies were performed by paediatric or general surgeons. However, the emergency services provided by paediatric surgeons outside tertiary paediatric hospitals are very limited in NSW. Results from a recent systematic review suggest that there are no differences in the rates of post-surgery complications, re-admissions, and mortality following appendicectomies in children performed by general and paediatric surgeons.20
Conclusion
Laparoscopic appendicectomy is now the most common surgical approach to managing appendicitis in children. The lower incidence of bowel obstruction following laparoscopic appendicectomy in children with uncomplicated appendicitis, and the similar rates in complicated appendicitis following either surgical approach, support preferring laparoscopic appendicectomy for children. However, the balance between earlier discharge and higher rates of re-presentations and re-admission after laparoscopic appendicectomy require further evaluation. For children with complicated appendicitis, post-operative complications were more likely to be associated with the severity of the condition than with the type of surgery. Our findings support the current NSW framework for the surgical management of acute appendicitis in children.
Box 1 – Laparoscopic appendicectomies as a proportion of all appendicectomies in children under 16 years of age, New South Wales, 2002–2013, by type of appendicitis (complicated, uncomplicated)
Box 2 – Patient and surgery characteristics for appendicectomies for appendicitis in children under 16 years of age, New South Wales, 2002–2013*
Patient and surgery characteristics |
Both operation forms |
Number of operations (proportion of appendicectomies in this group and year) |
|||||||||||||
Open appendicectomy |
Laparoscopic appendicectomy |
||||||||||||||
2002–2013 |
2002–2013 |
2002–2005 |
2006–2009 |
2010–2013 |
|||||||||||
All patients |
23 961 |
12 300 (51.3%) |
11 661 (48.7%) |
1478 (19.5%) |
3712 (47.1%) |
6471 (76.2%) |
|||||||||
Age (years) |
|||||||||||||||
0–4 |
691 (2.9%) |
497 (71.9%) |
194 (28.1%) |
10 (4.7%) |
41 (19.9%) |
143 (52.2%) |
|||||||||
5–8 |
3528 (14.7%) |
2229 (63.2%) |
1299 (36.8%) |
96 (8.7%) |
355 (31.6%) |
848 (64.9%) |
|||||||||
9–11 |
7448 (31.1%) |
4202 (56.4%) |
3246 (43.6%) |
394 (15.5%) |
996 (41.6%) |
1856 (73.8%) |
|||||||||
12–15 |
12 294 (51.3%) |
5372 (43.7%) |
6922 (56.3%) |
978 (26.2%) |
2320 (55.8%) |
3624 (82.4%) |
|||||||||
Sex |
|||||||||||||||
Boys |
13 794 (57.6%) |
7726 (56.0%) |
6068 (44.0%) |
599 (13.8%) |
1867 (41.0%) |
3602 (73.3%) |
|||||||||
Girls |
10 167 (42.4%) |
4574 (45.0%) |
5593 (55.0%) |
879 (27.0%) |
1845 (55.5%) |
2869 (80.1%) |
|||||||||
Socio-economic disadvantage (quintile) | |||||||||||||||
1 (most disadvantaged) |
5237 (21.9%) |
2247 (42.9%) |
2990 (57.1%) |
332 (21.1%) |
988 (57.7%) |
1670 (85.4%) |
|||||||||
2–4 |
14 529 (60.6%) |
7776 (53.5%) |
6753 (46.5%) |
914 (19.6%) |
2113 (44.5%) |
3726 (72.9%) |
|||||||||
5 (least disadvantaged) |
4082 (17.0%) |
2227 (54.6%) |
1855 (45.4%) |
224 (17.1%) |
579 (42.1%) |
1052 (75.1%) |
|||||||||
Pre-existing chronic diseases or major congenital anomalies† | |||||||||||||||
Yes |
669 (2.8%) |
403 (60.2%) |
266 (39.8%) |
76 (20.3%) |
84 (54.5%) |
106 (75.2%) |
|||||||||
No |
23 292 (97.2%) |
11 897 (51.1%) |
11 395 (48.9%) |
1402 (19.4%) |
3628 (47.0%) |
6365 (76.2%) |
|||||||||
Co-existing diagnosis‡ |
|||||||||||||||
Yes |
1646 (6.9%) |
447 (27.2%) |
1199 (72.8%) |
131 (42.5%) |
344 (70.8%) |
724 (85.0%) |
|||||||||
No |
22 315 (93.1%) |
11 853 (53.1%) |
10 462 (46.9%) |
1347 (18.5%) |
3368 (45.6%) |
5747 (75.2%) |
|||||||||
Hospital |
|||||||||||||||
Tertiary paediatric |
6125 (25.6%) |
2628 (42.9%) |
3497 (57.1%) |
237 (15.9%) |
1092 (54.0%) |
2168 (82.9%) |
|||||||||
Metropolitan |
6124 (25.6%) |
2740 (44.7%) |
3384 (55.3%) |
474 (21.7%) |
1085 (57.0%) |
1825 (89.6%) |
|||||||||
Regional/rural |
9356 (39.0%) |
5809 (62.1%) |
3547 (37.9%) |
511 (17.4%) |
1090 (33.8%) |
1946 (60.9%) |
|||||||||
Private |
2356 (9.8%) |
1123 (47.7%) |
1233 (52.3%) |
256 (26.2%) |
445 (60.9%) |
532 (82.2%) |
|||||||||
Transfers from other hospitals | |||||||||||||||
Yes |
2888 (12.1%) |
1415 (49.0%) |
1473 (51.0%) |
124 (16.5%) |
446 (45.3%) |
903 (78.3%) |
|||||||||
No |
21 073 (87.9%) |
10 885 (51.7%) |
10 188 (48.3%) |
1354 (19.8%) |
3266 (47.4%) |
5568 (75.8%) |
|||||||||
Type of appendicitis |
|||||||||||||||
Uncomplicated |
19 336 (80.7%) |
9738 (50.4%) |
9598 (49.6%) |
1300 (20.4%) |
3245 (49.4%) |
5053 (78.9%) |
|||||||||
Complicated |
4625 (19.3%) |
2562 (55.4%) |
2063 (44.6%) |
178 (14.7%) |
467 (35.5%) |
1418 (67.7%) |
|||||||||
Season of surgery |
|||||||||||||||
Summer |
5897 (24.6%) |
3211 (54.5%) |
2686 (45.5%) |
332 (17.5%) |
854 (43.3%) |
1500 (74.0%) |
|||||||||
Autumn |
5929 (24.7%) |
3112 (52.5%) |
2817 (47.5%) |
331 (17.6%) |
882 (46.1%) |
1604 (75.1%) |
|||||||||
Winter |
5937 (24.8%) |
2973 (50.1%) |
2964 (49.9%) |
380 (20.8%) |
926 (48.0%) |
1658 (76.0%) |
|||||||||
Spring |
6198 (25.9%) |
3004 (48.5%) |
3194 (51.5%) |
435 (21.9%) |
1050 (50.9%) |
1709 (79.6%) |
|||||||||
Day of surgery |
|||||||||||||||
Weekday |
18 210 (76.0%) |
9273 (50.9%) |
8937 (49.1%) |
1122 (19.6%) |
2875 (47.9%) |
4940 (76.3%) |
|||||||||
Weekend |
5751 (24.0%) |
3027 (52.6%) |
2724 (47.4%) |
356 (19.2%) |
837 (44.5%) |
1531 (75.9%) |
|||||||||
* To conserve space, only the summary data for open appendicectomies are included in this table; the full data are included in table 2 of the online Appendix. The data are also presented with column percentages in the online Appendix as table 3. † Diabetes, chronic kidney disease, obesity, chronic asthma, epilepsy, heart or other major anomalies. ‡ Secondary diagnosis of peritoneal adhesions, Meckel diverticulum, volvulus, ileus, ovarian cysts. | |||||||||||||||
Box 3 – Outcomes of appendicectomies for appendicitis in children under 16 years of age, New South Wales, 2002–2013
Outcomes following appendicectomy |
Uncomplicated appendicitis |
Complicated appendicitis |
|||||||||||||
Open appendicectomy |
Laparoscopic appendicectomy |
Open appendicectomy |
Laparoscopic appendicectomy |
||||||||||||
Number of patients |
9738 |
9598 |
2562 |
2063 |
|||||||||||
Length of hospital stay (days) |
|||||||||||||||
< 2 |
1082 (11.1%) |
1808 (18.8%) |
86 (3.4%) |
154 (7.5%) |
|||||||||||
2–3 |
4014 (41.2%) |
3857 (40.2%) |
290 (11.3%) |
381 (18.5%) |
|||||||||||
4–5 |
3884 (39.9%) |
3230 (33.7%) |
753 (29.4%) |
581 (28.2%) |
|||||||||||
≥ 5 |
758 (7.8%) |
703 (7.3%) |
1433 (55.9%) |
947 (45.9%) |
|||||||||||
Complications during initial admission |
|||||||||||||||
Post-operative intestinal obstruction |
34 (0.3%) |
27 (0.3%) |
104 (4.1%) |
68 (3.3%) |
|||||||||||
Post-operative intra-abdominal abscess |
0 |
0 |
19 (0.7%) |
24 (1.2%) |
|||||||||||
Respiratory complications |
21 (0.2%) |
15 (0.2%) |
36 (1.4%) |
13 (0.6%) |
|||||||||||
Complications of other organs, or unspecified |
35 (0.4%) |
49 (0.5%) |
35 (1.4%) |
35 (1.7%) |
|||||||||||
Wound infections or sepsis |
21 (0.2%) |
20 (0.2%) |
98 (3.8%) |
41 (2.0%) |
|||||||||||
Adverse effect of therapeutic drugs |
53 (0.5%) |
57 (0.6%) |
33 (1.3%) |
31 (1.5%) |
|||||||||||
Any post-operative complication |
146 (1.5%) |
174 (1.8%) |
266 (10.4%) |
184 (8.9%) |
|||||||||||
Complications during re-admission (within 28 days) | |||||||||||||||
Intestinal obstruction |
28 (0.3%) |
14 (0.1%) |
45 (1.8%) |
22 (1.1%) |
|||||||||||
Intra-abdominal abscess |
41 (0.4%) |
43 (0.4%) |
89 (3.5%) |
48 (2.3%) |
|||||||||||
Wound infections or sepsis |
94 (1.0%) |
109 (1.1%) |
131 (5.1%) |
66 (3.2%) |
|||||||||||
Symptomatic (abdominal pain, fever, nausea or vomiting) |
86 (0.9%) |
144 (1.5%) |
60 (2.3%) |
53 (2.6%) |
|||||||||||
Any post-operative complication requiring re-admission* |
301 (3.1%) |
361 (3.8%) |
290 (11.3%) |
167 (8.1%) |
|||||||||||
Any re-admission |
395 (4.1%) |
478 (5.0%) |
319 (12.5%) |
196 (9.5%) |
|||||||||||
Re-presentation to emergency department (within 28 days), not requiring hospital admission | |||||||||||||||
Symptomatic (abdominal pain, fever, nausea or vomiting) |
60 (0.6%) |
128 (1.3%) |
45 (1.8%) |
48 (2.3%) |
|||||||||||
Wound infections or sepsis |
48 (0.5%) |
52 (0.5%) |
25 (1.0%) |
15 (0.7%) |
|||||||||||
Any post-operative complication |
164 (1.7%) |
221 (2.3%) |
100 (3.9%) |
79 (3.8%) |
|||||||||||
Any emergency department presentation |
291 (3.0%) |
442 (4.6%) |
152 (5.9%) |
123 (6.0%) |
|||||||||||
All complications |
|||||||||||||||
Intestinal obstruction† |
54 (0.6%) |
38 (0.4%) |
141 (5.5%) |
89 (4.3%) |
|||||||||||
Intra-abdominal abscess |
41 (0.4%) |
45 (0.5%) |
107 (4.2%) |
72 (3.5%) |
|||||||||||
Wound infections or sepsis† |
151 (1.6%) |
175 (1.8%) |
239 (9.3%) |
118 (5.7%) |
|||||||||||
Any post-operative complication† |
569 (5.8%) |
708 (7.4%) |
586 (22.9%) |
388 (18.8%) |
|||||||||||
* Includes post-operative complications of nervous, endocrine, circulatory, other digestive, or genito-urinary systems, and complications related to anaesthesia. † Some children had complications during surgery admission and within 28 days of separation; as a result, total figures may not equal sum of the individual components. | |||||||||||||||
Box 4 – Simple and multivariate analysis of complications by operation mode
|
Post-operative complications |
Crude odds ratio* |
Adjusted odds ratio* |
|||||||||||||
Open appendicectomy |
Laparoscopic appendicectomy |
||||||||||||||
Uncomplicated appendicitis |
|||||||||||||||
Any complication |
569 (5.8%) |
708 (7.4%) |
1.28 (1.14–1.44) |
1.13 (0.98–1.30) |
|||||||||||
Intestinal obstruction |
54 (0.6%) |
38 (0.4%) |
0.72 (0.45–1.14) |
0.59 (0.36–0.97) |
|||||||||||
Intra-abdominal abscess |
41 (0.4%) |
45 (0.5%) |
1.12 (0.74–1.70) |
1.12 (0.73–1.70) |
|||||||||||
Wound infections |
151 (1.6%) |
175 (1.8%) |
1.24 (0.96–1.59) |
1.11 (0.81–1.52) |
|||||||||||
Complicated appendicitis |
|||||||||||||||
Any complication |
586 (22.9%) |
388 (18.8%) |
0.77 (0.66–0.90) |
0.78 (0.68–0.90) |
|||||||||||
Intestinal obstruction |
141 (5.5%) |
89 (4.3%) |
0.77 (0.55–1.08) |
0.76 (0.53–1.08) |
|||||||||||
Intra-abdominal abscess |
107 (4.2%) |
72 (3.5%) |
0.80 (0.59–1.10) |
0.94 (0.63–1.39) |
|||||||||||
Wound infections |
239 (9.3%) |
118 (5.7%) |
0.60 (0.51–0.72) |
0.55 (0.44–0.69) |
|||||||||||
Complicated appendicitis† |
|||||||||||||||
Any complication |
471 (22.8%) |
211 (23.9%) |
1.05 (0.91–1.23) |
0.98 (0.83–1.16) |
|||||||||||
Intestinal obstruction |
113 (5.5%) |
49 (5.6%) |
1.01 (0.67–1.52) |
0.97 (0.62–1.52) |
|||||||||||
Intra-abdominal abscess |
95 (4.6%) |
47 (5.3%) |
1.09 (0.82–1.46) |
1.06 (0.72–1.55) |
|||||||||||
Wound infections |
193 (9.3%) |
69 (7.8%) |
0.84 (0.66–1.08) |
0.67 (0.50–0.90) |
|||||||||||
* Laparoscopic v open appendicectomy; adjusted odds ratio adjusted for all patient and surgery characteristics, period (years), and clustering within hospitals. † Sensitivity analysis: 1674 patients with localised peritonitis were omitted. | |||||||||||||||
Received 5 June 2017, accepted 3 October 2017
- Francisco J Schneuer1
- Susan E Adams2
- Jason P Bentley1
- Andrew JA Holland3
- Carmen Huckel Schneider1
- Leslie White4
- Natasha Nassar1
- 1 Menzies Centre for Health Policy, University of Sydney, Sydney, NSW
- 2 Sydney Children's Hospital, Sydney, NSW
- 3 The Children's Hospital at Westmead, Sydney, NSW
- 4 University of New South Wales, Sydney, NSW
We thank the NSW Ministry of Health for providing access to population health data, and the NSW Centre for Health Record Linkage for linking the datasets. The findings and views reported in this study, however, are those of the authors. This work was funded by a National Health and Medical Research Council (NHMRC) Project Grant (APP1047263). Natasha Nassar was supported by an NHMRC Career Development Fellowship (APP1067066).
No relevant disclosures.
- 1. Coward S, Kareemi H, Clement F, et al. Incidence of appendicitis over time: a comparative analysis of an administrative healthcare database and a pathology-proven appendicitis registry. PLoS One 2016; 11: e0165161.
- 2. Bhattacharya K. Kurt Semm: a laparoscopic crusader. J Minim Access Surg 2007; 3: 35-36.
- 3. Jen HC, Shew SB. Laparoscopic versus open appendectomy in children: outcomes comparison based on a statewide analysis. J Surg Res 2010; 161: 13-17.
- 4. Esposito C, Calvo AI, Castagnetti M, et al. Open versus laparoscopic appendectomy in the paediatric population: a literature review and analysis of complications. J Laparoendosc Adv Surg Tech A 2012; 22: 834-839.
- 5. Markar SR, Blackburn S, Cobb R, et al. Laparoscopic versus open appendectomy for complicated and uncomplicated appendicitis in children. J Gastrointest Surg 2012; 16: 1993-2004.
- 6. Australian Bureau of Statistics. 2033.0.55.001. Census of population and housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011. IRSD. Mar 2013. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001∼2011∼Main%20Features∼IRSD∼10005 (viewed Feb 2018).
- 7. Australian Bureau of Statistics. 3101.0. Australian demographic statistics, Jun 2017; Table 51. Dec 2017. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3101.0Jun%202017?OpenDocument (viewed Feb 2018).
- 8. Gasior AC, St Peter SD, Knott EM, et al. National trends in approach and outcomes with appendicitis in children. J Pediatr Surg 2012; 47: 2264-2267.
- 9. van den Boom AL, Gorter RR, van Haard PM, et al. The impact of disease severity, age and surgical approach on the outcome of acute appendicitis in children. Pediatr Surg Int 2015; 31: 339-345.
- 10. Gosemann JH, Lange A, Zeidler J, et al. Appendectomy in the paediatric population-a German nationwide cohort analysis. Langenbecks Arch Surg 2016; 401: 651-659.
- 11. Cheong LH, Emil S. Paediatric laparoscopic appendectomy: a population-based study of trends, associations, and outcomes. J Pediatr Surg 2014; 49: 1714-1718.
- 12. Luo CC, Chien WK, Huang CS, et al. National trends in therapeutic approaches and outcomes for paediatric appendicitis: a Taiwanese nationwide cohort study. Pediatr Surg Int 2015; 31: 647-651.
- 13. Aziz O, Athanasiou TV, Tekkis PP, et al. Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg 2006; 243: 17-27.
- 14. Tomecka MJ, Bortsov AV, Miller NR, et al. Substantial postoperative pain is common among children undergoing laparoscopic appendectomy. Paediatr Anaesth 2012; 22: 130-135.
- 15. Lee SL, Yaghoubian A, Kaji A. Laparoscopic vs open appendectomy in children: outcomes comparison based on age, sex, and perforation status. Arch Surg 2011; 146: 1118-1121.
- 16. Beasley SW. Are changes in referral patterns always justified? ANZ J Surg 2012; 82: 572-573.
- 17. Wilson BE, Cheney L, Patel B, et al. Appendicectomy at a children’s hospital: what has changed over a decade? ANZ J Surg 2012; 82: 639-643.
- 18. NSW Surgical Services Taskforce Paediatric Surgery Sub Group. Paediatric surgery model for designated area paediatric surgical sites. Sydney: NSW Department of Health, 2008. https://www.aci.health.nsw.gov.au/resources/surgical-services/delivery/predictable-surgery/documents/paediatric-surgery.pdf (viewed Jan 2017).
- 19. NSW Kids and Families. Surgery for children in metropolitan Sydney: strategic framework. Sydney: NSW Department of Health, 2014. http://www.health.nsw.gov.au/kidsfamilies/paediatric/Publications/surgery-for-children-framework.pdf (viewed Jan 2017).
- 20. Healy DA, Doyle D, Moynagh E, et al. Systematic review and meta-analysis on the influence of surgeon specialization on outcomes following appendicectomy in children. Medicine (Baltimore) 2015; 94: e1352.





Abstract
Objective: To assess and compare the post-operative outcomes of open and laparoscopic appendicectomy in children.
Design: Record linkage analysis of administrative hospital (Admitted Patient Data Collection) and emergency department (Emergency Department Data Collection) data.
Participants, setting: Children under 16 years of age who underwent an appendicectomy in a public or private hospital in New South Wales between January 2002 and December 2013.
Main outcome measures: Association between type of appendicectomy and post-operative complications within 28 days of discharge, adjusted for patient characteristics and type of hospital.
Results: Of 23 961 children who underwent appendicectomy, 19 336 (81%) had uncomplicated appendicitis and 4625 (19%) had appendicitis complicated by abscess, perforation, or peritonitis. The proportion of laparoscopic appendicectomies increased from 11.8% in 2002 to 85.8% in 2013. In cases of uncomplicated appendicitis, laparoscopic appendicectomy was associated with more post-operative complications (mostly symptomatic re-admissions or emergency department presentations) than open appendicectomy (7.4% v 5.8%), but with a reduced risk of post-operative intestinal obstruction (adjusted odds ratio [aOR], 0.59; 95% CI, 0.36–0.97). For cases of complicated appendicitis, the risk of wound infections was lower for laparoscopic appendicectomy (aOR, 0.67; 95% CI, 0.50–0.90), but not the risks of intestinal obstruction (aOR, 0.97; 95% CI, 0.62–1.52) or intra-abdominal abscess (aOR, 1.06; 95% CI, 0.72–1.55).
Conclusion: Post-appendicectomy outcomes were similar for most age groups and hospital types. Children with uncomplicated appendicitis have lower risk of post-operative bowel obstruction after laparoscopic appendicectomy than after open appendicectomy, but may be discharged before their post-operative symptoms have adequately resolved.