The known Inappropriately high rates of psychotropic prescribing in Australian residential aged care facilities (RACFs) have been reported for several decades despite media and political attention and guidelines for reducing use.
The new A multi-strategic, interdisciplinary program implemented in 150 Australian RACFs achieved significant reductions in antipsychotic and benzodiazepine prescribing without substitution by other psychotropic agents. For almost 40% of residents prescribed these agents at baseline, the drugs had been ceased or their doses reduced by 6 months.
The implications Targeted interventions can reduce over-reliance on psychotropic medication for managing mental and psychological symptoms of RACF residents.
Antipsychotic drugs are commonly prescribed to treat the behavioural and psychological symptoms of dementia,1 but their effectiveness in this role is modest, and the associated risks are severe, including falls, stroke, and death.2,3 Similarly, benzodiazepines can be effective for the short term treatment of sleep disturbances, anxiety, and agitation, but their use in older people is associated with increased risks of falls,2 pneumonia,4 and death;5 the risks of falls and death are greater with higher doses and longer treatment.2,5 Consequently, these psychotropic agents should be prescribed cautiously, at the lowest therapeutic doses for as short a time as possible, and their effectiveness and adverse effects monitored regularly.3,6
The high rates of antipsychotic prescribing in residential aged care facilities (RACFs) have been recognised as a problem for decades,7-9 resulting in government inquiries,7,10 prescribing restrictions,3 and interventions9,11,12 and guidelines for reducing their use.3 Benzodiazepine prescribing in RACFs has received less attention, although commonly used6 despite the attendant risks.2,4,5 A recent study concluded that only 10% of psychotropic agents prescribed for RACF residents with dementia were completely appropriate, particularly with respect to indication and therapy duration.13
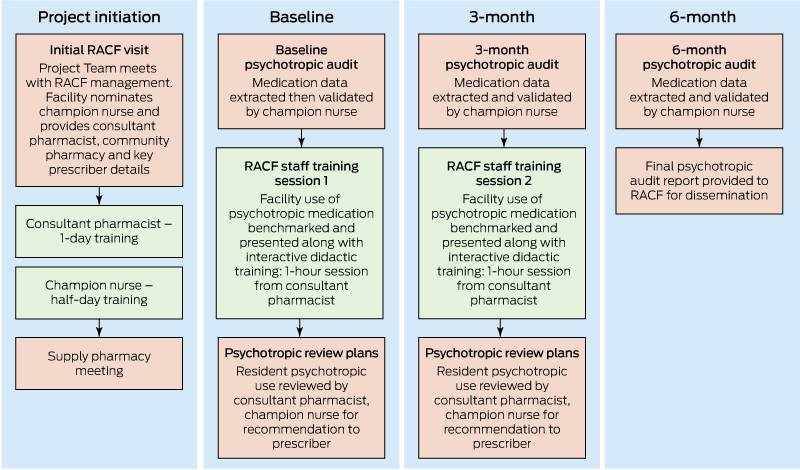
The Reducing Use of Sedatives (RedUSe) intervention was designed to promote the appropriate use of antipsychotics and benzodiazepines in RACFs. “Sedatives” in the RedUSe acronym encompasses both antipsychotics and benzodiazepines. The RedUSe intervention consists of three sequential strategies: audit and feedback; staff education; and interdisciplinary review.12 To test RedUSe, a controlled trial in 25 RACFs was conducted during 2008–09; antipsychotic use was reduced by 8% and benzodiazepine use by 15% in the intervention facilities, whereas psychotropic prescribing rates increased in the control RACFs.12
In 2013, RedUSe received federal funding to expand to 150 RACFs across Australia. The aim of our study was to assess the impact of the intervention on antipsychotic and benzodiazepine use in this large national sample of RACFs.
Methods
Implementation research design
The Theoretical Domains Framework,14 an instrument for assessing behaviour, barriers, and enablers in order to inform the design of complex interventions, was used to enhance the RedUSe program for its expansion. The main barriers and enablers to evidence-based practice were identified by qualitative evaluation of the RedUSe trial,12 and by reviewing other publications.7,11 Barriers included staff believing the medications were highly effective for treating behavioural and psychological symptoms in older people, poor knowledge about their adverse effects, inadequately defined roles for reviewing psychotropic medication use, poor prescriber engagement, and resource constraints on providing non-pharmacological therapy. Enablers included staff education and a structured interdisciplinary review process.11,12 The expanded RedUSe program was enhanced by incorporating several strategies for changing behaviour: developing interactive staff training to challenge positive beliefs about psychotropics; clearly defining health practitioner roles for reviewing psychotropic use; creating a “champion nurse” role (practice leaders working with various disciplines to ensure that guideline implementation and recommendations saturate an organisation),15 and providing educational outreach visits (academic detailing) for prescribers.
The principal outcome measure was the prevalence of regular charted antipsychotic and benzodiazepine use across RACFs at baseline, and at 3 and 6 months. Secondary measures included:
-
mean RACF chlorpromazine and diazepam equivalent doses/day/resident;
-
proportions of residents for whom antipsychotics or benzodiazepines were ceased, or the doses reduced; and
-
prevalence of antidepressant and pro re nata (prn = as required) antipsychotic and benzodiazepine use, to assess possible substitution of regularly prescribed agents.
Participants
RACFs comprised the main participant group; two further groups were consultant pharmacists who delivered staff education, and community pharmacies that provided prescribing data. Recruiting involved a combination of approaches to achieve a heterogeneous sample. Initially, two large national RACF organisations agreed to participate. Two aged care advocacy bodies, Aged and Community Services Australia and Leading Age Services Australia, featured RedUSe in industry journals, resulting in more than 300 expressions of interest. RACFs with fewer than 26 residents or from outer rural or remote locations16 were excluded. After an RACF had volunteered, their consultant pharmacist and pharmacy were invited to participate (two pharmacists and one pharmacy declined). Recruiting continued until consent was received from 150 facilities and their pharmacists and pharmacies. The final RACF sample was compared with Australian Institute of Health and Welfare (AIHW) aged care data for 2014–1517 to assess its representativeness. All 150 facilities completed the 6-month program, in four stages, between March 2014 and April 2016.
Prescribing data
Full prescribing data was captured for each resident, including agent, dose and frequency, and whether ordered regularly (ie, regular recorded sequence of administration) or prn.18 Medications were classified according to the World Health Organization (WHO) Anatomical Therapeutic Chemical (ATC) code.19 The agents evaluated were antipsychotics (ATC code, N05A, excluding lithium [N05AN] and prochlorperazine [N05AB04], as they are not typically used in RACFs to treat behavioural and psychological symptoms), anxiolytics (N05B), hypnotics (N05C), antidepressants (N06A), and clonazepam (N03AE01). To assess dose variations, antipsychotic doses were converted to chlorpromazine equivalents20 and the mean chlorpromazine dose/day/resident was calculated.18 Benzodiazepine doses were converted to diazepam equivalents21 and the mean diazepam dose/day/resident was calculated.
Intervention strategies
Prescribing data, available from pharmacies that used computerised packing systems (eg, Webstercare systems) to pack residents’ medications into blister-packs or sachets, were extracted by a purpose-built program, securely stored on a web server, and validated by the champion nurse, who also excluded data for residents in respite and palliative care.18 Resident information and unpacked medications (eg, solutions) could be added manually. The validated prescribing data were de-identified and re-checked, then aggregated to produce an audit of psychotropic prescribing rates for each RACF, benchmarked against other participants, as a point prevalence snapshot.18
The staff at each facility were educated about psychotropic medications by the consultant pharmacist, who had completed training in the evidence-based use of psychotropic agents and the implementation of RedUSe (Box 1). One-hour educational sessions were held at baseline and at 3 months, and the level of psychotropic use at their RACF compared with that at other facilities. The main objective of these sessions was to challenge beliefs that antipsychotics and benzodiazepines were highly effective for treating behavioural and psychological symptoms in older people. Didactic education (educational video and presentation outlining the risks and benefits of psychotropic use) was also employed. The second session incorporated enhanced content on non-pharmacological strategies for managing behavioural and psychological symptoms of dementia, insomnia, and anxiety, and the staff were shown graphs tracking psychotropic prescribing at their RACF.
The psychotropic review plan encouraged interdisciplinary review every 3 months. After the initial audit, a plan comprising three sections was prepared for each resident prescribed regular antipsychotics or benzodiazepines. The first two sections contained the recommendations of the pharmacist and the champion nurse, both of whom had attended pre-intervention training which emphasised that residents with serious mental illness, including schizophrenia, were usually managed by mental health specialists, and that adjusting antipsychotic medication for these residents should not be recommended. In the third section, the prescriber recorded the decision about whether or not to adjust the medication. This process was repeated after the 3-month audit.
Treatment guidelines (online Appendix) based on the recommendations of professional bodies3,6 and incorporating dose reduction schedules for both psychotropic classes were provided to all RACF staff. Key prescribers, identified by their respective RACFs, were sent intervention information and guidelines, and encouraged to discuss the intervention with the champion nurse. Academic detailing sessions by trained facilitators were also offered to attending GPs and nurse practitioners. Finally, pamphlets on benzodiazepine and antipsychotic use, developed with consumer representatives, were disseminated by RACFs to residents and relatives. Further details on intervention strategies have been published elsewhere.22
Statistical analysis
The distribution of the RedUSe RACF sample was compared with AIHW data for 2014–1517 in a χ2 test. Prevalence of psychotropic agent use was expressed as the mean proportions of residents in each facility prescribed these medications, with 95% confidence intervals (CIs). Changes in psychotropic prescribing during the intervention were estimated in linear mixed effects models. Random slopes and intercepts were modelled for each facility to account for uncontrolled differences in prescribing between RACFs. Model assumptions were checked with standard graphical methods, including examination of residuals; log transformations were applied to data when appropriate. All statistical analyses were undertaken in R 3.3.2 for Windows (R Foundation for Statistical Computing). Linear mixed effects models were fitted with the R package lme4, and multiple comparisons within medication classes were adjusted with the Tukey method as implemented by the multcomp R package.
Ethics approval
Ethics approval for this study was obtained from the Human Research Ethics Committee (Tasmania) Network (reference, H0013545). Consent was provided at the institutional level; individual resident consent was not required because data were de-identified.
Results
One hundred and fifty RACFs were recruited; they ranged in size from 26 to 172 residents (total, 12 157 residents). According to AIHW data on RACFs,17 the RedUSe sample was representative in terms of Geographical Standard Remoteness Areas distribution, but not with respect to state (RedUSe sample had fewer facilities in New South Wales and Western Australia, more in South Australia and the Australian Capital Territory) or facility size (mean, 81 residents; AIHW mean, 60 residents17) (Box 2). Demographic information was available for 24% of residents; their mean age was 85.8 years (standard deviation, 8.6 years).
The mean prevalence of antipsychotic agent use declined from 21.6% (95% CI, 20.4–22.9%) at baseline to 18.9% (95% CI, 17.7–20.1%; P < 0.001) at 6 months, a 13% reduction (Box 3). The mean prevalence of benzodiazepine use declined from 22.2% (95% CI, 21.0–23.5%) at baseline to 17.6% (95% CI, 16.5–18.7; P < 0.001) at 6 months, a 21% reduction (Box 3). In total, 115 RACFs (77%) reduced antipsychotic prescribing and 127 facilities (85%) benzodiazepine prescribing; 99 (66%) recorded reductions for both classes.
The mean chlorpromazine equivalent dose declined from 22.9 mg/resident/day (95% CI, 19.8–26.0 mg/resident/day) at baseline to 20.2 mg/resident/day (95% CI, 17.5–22.9 mg/resident/day) at 6 months, a 12% decrease (P < 0.001). The mean diazepam equivalent dose declined from 1.4 mg/resident/day (95% CI, 1.3–1.5 mg/resident/day) to 1.1 mg/resident/day (95% CI, 0.9–1.2 mg/resident/day), a 23% reduction (P < 0.001).
A total of 2195 residents regularly prescribed antipsychotics and 2247 residents receiving regular benzodiazepines at baseline were present for all three audits. For 40% of these residents, the medications were reduced (15%) or ceased altogether (24%) during the 6-month intervention (Box 4).
Possible substitution was assessed by examining the prescribing of antidepressants and prn psychotropic drugs. There was no change in the overall prevalence of antidepressant prescribing (P = 0.17), indicating that these medications were not substituted for antipsychotics and benzodiazepines. Nor was there a shift to prn prescribing of psychotropic agents; overall prn prescribing of antipsychotics declined by 13% (P = 0.004) and benzodiazepines by 8% (P = 0.020) (Box 5).
Discussion
The multi-strategic, interdisciplinary RedUSe intervention in 150 Australian RACFs reduced the prevalence of regular antipsychotic prescribing in these facilities by 13% and that of benzodiazepines by 21%, without an increase in prn prescribing of psychotropic drugs.
Several international initiatives have aimed to reduce antipsychotic prescribing in RACFs. In 2009, the United Kingdom Department of Health pledged to reduce prescribing them for people with dementia by two-thirds within 3 years.7 Although this announcement focused attention on the issue, a subsequent analysis of more than 600 UK RACFs found that their use in this population had not decreased.23 In 2012, the United States Centers for Medicare and Medicaid Services (CMS) launched a national initiative to reduce antipsychotic use in RACFs, including public reporting of antipsychotic prescribing rates.9 By 2015, prescribing had been reduced by 27%. However, nearly 10% of residents (those with diagnoses of schizophrenia, Huntington disease or Tourette syndrome) were excluded from the analysis; if these residents had been included in the analysis, as they were for the RedUSe intervention, the mean reduction over 6 months was 3%,9 much lower than our 13%.
One of the most successful interventions for reducing antipsychotic use in RACFs was the UK Focussed Intervention Training and Support (FITS) program, which included extensive education of nurses about psychosocial approaches to care for people with dementia, and support by psychologists.11 However, the recruitment target of 150 facilities was not achieved when FITS was expanded during 2012–2014, and final data were available for only 53 RACFs; the high dropout rate was attributed to insufficient staff time.11
Few interventions have attempted to reduce benzodiazepine prescribing in RACFs. A French intervention during 2011–2012 (more than 3900 residents) assessed the impact of interdisciplinary meetings and audit on benzodiazepine use. No significant reduction was achieved; the authors concluded that specifically designed interventions were required.24
A major strength of our study was that the reductions in antipsychotic and benzodiazepine prescribing we found were based on the total RACF population, not just residents with dementia. Nor were residents excluded by psychiatric diagnosis; in the US, suspicions have been expressed that residents are diagnosed with schizophrenia to justify antipsychotic use.9 Another strength is that prescribing information was obtained from pharmacy packing programs.18 In the CMS initiative and FITS, antipsychotic prescribing was reported by staff, resulting in potential reporting bias.9,11 Auditing of medication charts also places demands on nurses’ time. A major advantage of RedUSe was its feasibility; unlike FITS, the entire sample of 150 RACFs completed the intervention.
An important finding was the considerable proportion of residents for whom antipsychotics or benzodiazepines were stopped or their dose reduced, leading to significant reductions in the mean chlorpromazine and diazepam equivalent doses for the 150 RACFs. As mortality and fall rates have been linked to higher doses and longer duration of psychotropic medication,2,5 RedUSe can have an effect on these important outcomes; we have consequently published interim findings from a sub-study assessing clinical and economic outcomes.22
A recent Australian study in 17 NSW RACFs found that less than 5% of prescribed psychotropic medications were ceased or their doses reduced in routine practice over 6 months.25 Our finding that the prescribing of antipsychotics and benzodiazepines had been reduced or ceased altogether for 39% of residents over 6 months shows that a multi-strategic, interprofessional intervention can markedly increase the frequency of review of these medications for potential discontinuation, consistent with guideline recommendations.3,6
We could not determine which of the RedUSe strategies was the most influential because they were not tested separately. However, interim qualitative evaluation indicates that the strategies were perceived as building upon each other, starting with awareness raising by dissemination of local prescribing data, reinforced by staff education, and followed by interdisciplinary review. This appraisal is supported by a review which concluded that multi-strategic interventions are more likely to reduce benzodiazepine prescribing in RACFs.26
Lack of funding did not permit a follow-up investigation, so the sustainability of RedUSe is untested. In the RedUSe pilot trial,12 however, the level of psychotropic prescribing was re-assessed 12 months after the intervention;27 benzodiazepine use and the mean diazepam dose equivalent level had continued to decline in the year after the active intervention, but antipsychotic prescribing returned to baseline levels in the absence of an active intervention, with mean chlorpromazine equivalent levels static.27 The pilot trial was restricted to Tasmania and conducted 9 years ago; psychotropic prescribing in other Australian states may be different.
Limitations
As dedicated implementation research, the funding rules precluded a controlled trial design, so that psychotropic prescribing may have been influenced by factors other than the intervention. Further, ascertainment bias is possible because many RACFs volunteered to participate, although more than one-third of facilities were nominated by their parent organisation. Another limitation was that prn psychotropic agents listed in medication charts may not have been taken by the resident;8 this could not be assessed. The prescribing of opioids and gabapentinoids for sedation in substitution practice was not assessed. A final limitation was the suboptimal participation of prescribers; only 51% of those invited participated in academic detailing, although their engagement was promoted by other means. Despite this shortcoming, the reductions in antipsychotic and benzodiazepine prescribing were substantial, reflecting the strong influence of staff and pharmacists on psychotropic use in RACFs.
Conclusion
The national expansion of the RedUSe intervention led to statistically significant reductions in the prescribing of antipsychotic agents and benzodiazepines for residents of RACFs. The program should be made available to all Australian RACFs to reduce the inappropriate prescribing of psychotropic medications.
Box 2 – Residential aged care facilities (RACFs) in Australia: Australian Institute of Health and Welfare (AIHW) aged care data and the RedUSe sample, 2014–15
|
|
AIHW data16 |
RedUSe sample |
P* |
||||||||||||
|
|
|||||||||||||||
|
Number of RACFs |
2510 |
150 |
|
||||||||||||
|
State |
|
|
< 0.001 |
||||||||||||
|
New South Wales |
842 (33.5%) |
29 (19%) |
|
||||||||||||
|
Victoria |
693 (27.6%) |
33 (22%) |
|
||||||||||||
|
Queensland |
415 (16.5%) |
35 (23%) |
|
||||||||||||
|
South Australia |
246 (9.8%) |
32 (21%) |
|
||||||||||||
|
Western Australia |
223 (8.9%) |
5 (3%) |
|
||||||||||||
|
Tasmania |
66 (2.6%) |
10 (7%) |
|
||||||||||||
|
Australian Capital Territory |
25 (1.0%) |
6 (4%) |
|
||||||||||||
|
Geographical Standard Remoteness Areas15 |
|
0.09 |
|||||||||||||
|
Major city (RA1) |
1638 (65.3%) |
106 (71%) |
|
||||||||||||
|
Inner regional (RA2) |
596 (23.7%) |
36 (24%) |
|
||||||||||||
|
Outer regional (RA3) |
276 (11.0%) |
8 (5%) |
|
||||||||||||
|
RACF size |
|
|
0.002 |
||||||||||||
|
21–40 beds |
467 (18.6%) |
13 (9%) |
|
||||||||||||
|
41–60 beds |
649 (25.9%) |
34 (23%) |
|
||||||||||||
|
61–80 beds |
466 (18.6%) |
30 (20%) |
|
||||||||||||
|
81–100 beds |
360 (14.3%) |
36 (24%) |
|
||||||||||||
|
More than 100 beds |
568 (22.6%) |
37 (25%) |
|
||||||||||||
|
|
|||||||||||||||
|
* χ2 tests. |
|||||||||||||||
Box 3 – Mean prevalence of antipsychotic and benzodiazepine prescribing (with 95% confidence intervals) in 150 residential aged care facilities at baseline and at 3 and 6 months after implementation of the RedUSe program
|
|
Audit |
P* |
|||||||||||||
|
Baseline |
3 months |
6 months |
|||||||||||||
|
|
|||||||||||||||
|
Residents audited |
12 157 |
12 185 |
12 154 |
|
|||||||||||
|
Antipsychotics |
21.6% (20.4–22.9%) |
19.7% (18.4–20.9%) |
18.9% (17.7–20.1%) |
< 0.001 |
|||||||||||
|
Atypical |
20.1% (18.8–21.3%) |
18.3% (17.1–19.5%) |
17.7% (16.5–18.9%) |
< 0.001 |
|||||||||||
|
Typical |
1.7% (1.6–1.9%) |
1.5% (1.2–1.8%) |
1.3% (1.3–1.1%) |
0.001 |
|||||||||||
|
Benzodiazepines |
22.2% (21.0–23.5%) |
19.6% (18.4–20.8%) |
17.6% (16.5–18.7%) |
< 0.001 |
|||||||||||
|
Anxiolytic |
12.4% (11.5–13.4%) |
11.4% (10.4–12.3%) |
10.5% (9.6–11.4%) |
< 0.001 |
|||||||||||
|
Hypnotic |
11.7% (10.8–12.6%) |
9.8% (9.0–10.6%) |
8.3% (7.6–8.9%) |
< 0.001 |
|||||||||||
|
|
|||||||||||||||
|
* Linear mixed effects models. |
|||||||||||||||
Box 4 – Psychotropic modification at 6 months of antipsychotic and benzodiazepine medication prescribed for residents of aged care facilities who underwent the entire 6-month RedUSe intervention
|
Agent class |
Residents taking agents |
Agent ceased |
Dose reduced |
Dose unchanged |
Dose increased |
Agent changed |
|||||||||
|
|
|||||||||||||||
|
Antipsychotics |
2195 |
483 (22%) |
354 (16%) |
1144 (52%) |
160 (7.5%) |
54 (2.5%) |
|||||||||
|
Benzodiazepines |
2247 |
576 (26%) |
332 (15%) |
1211 (54%) |
81 (3.5%) |
47 (2.0%) |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 5 – Prevalence of antidepressant and prn drug prescribing (with 95% confidence intervals) in 150 RedUSe residential aged care facilities (RACFs)
|
|
Audit |
P* |
|||||||||||||
|
Baseline |
3 months |
6 months |
|||||||||||||
|
|
|||||||||||||||
|
Antidepressant prescribing |
|
|
|
|
|||||||||||
|
Residents audited (145 RACFs) |
11 891 |
11 927 |
11 896 |
|
|||||||||||
|
All antidepressants |
41.3% (39.7–42.9%) |
40.4% (38.7–42.1%) |
40.0% (38.2–41.7%) |
0.17 |
|||||||||||
|
Selective serotonin re-uptake inhibitors (SSRIs) |
20.0% (19.0–21.1%) |
19.5 (18.4–20.5%) |
19.5% (18.4–20.6%) |
0.31 |
|||||||||||
|
Mirtazapine |
12.0% (11.0–13.0%) |
11.7% (10.7–12.7%) |
11.7% (10.7–12.6%) |
0.18 |
|||||||||||
|
Tricyclic antidepressants |
4.6% (4.1–5.1%) |
4.4% (3.9–5.0%) |
4.2% (3.7–4.8%) |
0.09 |
|||||||||||
|
Pro re nata (prn) prescribing |
|
|
|
|
|||||||||||
|
Residents audited (143 RACFs) |
11 629 |
11 649 |
11 625 |
|
|||||||||||
|
Antipsychotics (prn) |
10.8% (9.5–12.1%) |
10.2% (8.9–11.5%) |
9.4% (8.2–10.6%) |
0.004 |
|||||||||||
|
Benzodiazepines (prn)† |
30.1% (27.6–32.6%) |
28.8% (26.3–31.4%) |
27.8% (25.3–30.3%) |
0.020 |
|||||||||||
|
Anxiolytics |
17.8% (15.9–19.6%) |
17.0% (15.1–18.9%) |
16.3% (14.5–18.2%) |
0.035 |
|||||||||||
|
Hypnotics |
16.2% (14.7–17.7%) |
15.4% (13.9–16.8%) |
14.7% (13.2–16.1%) |
0.008 |
|||||||||||
|
|
|||||||||||||||
|
* Linear mixed effects models. † As some residents were taking several prn benzodiazepines, the overall reduction is slightly less than that for the benzodiazepine subtypes. |
|||||||||||||||
Received 30 August 2017, accepted 11 December 2017
- Juanita L Westbury1
- Peter Gee2
- Tristan Ling2
- Donnamay T Brown1
- Katherine H Franks1
- Ivan Bindoff2
- Aidan Bindoff1
- Gregory M Peterson2
- 1 Wicking Dementia Research and Education Centre, University of Tasmania, Hobart, TAS
- 2 University of Tasmania, Hobart, TAS
The national expansion of the RedUSe intervention was supported by the Australian Department of Health as part of the Aged Care Services Improvement and Healthy Ageing Grants (ACSIHAG) program (3-6D8KE). Juanita Westbury was supported by a National Health and Medical Research Council Translating Research Into Practice (TRIP) Fellowship during 2014–2016. We acknowledge the contributions of our collaborators, our steering group, and project staff. We especially thank the staff and residents at all 150 participating RACFs, their consultant pharmacists, supply community pharmacies, and the prescribers providing medical care to the residents.
No relevant disclosures.
- 1. Hollingworth S, Siskind D, Nissen LM, et al. Patterns of antipsychotic medication use in Australia: 2002–2007. Aust N Z J Psychiatry 2010; 44: 372-377.
- 2. Sterke C, van Beeck EF, van der Velde N, et al. New insights: dose–response relationship between psychotropic drugs and falls: a study in nursing home residents with dementia. J Clin Pharmacol 2012; 52: 947–955.
- 3. Royal Australian and New Zealand College of Psychiatrists. Antipsychotic medications as a treatment of behavioural and psychological symptoms of dementia (Professional Practice Guideline 10). Aug 2016. https://www.ranzcp.org/Files/Resources/College_Statements/Practice_Guidelines/pg10-pdf.aspx (viewed Apr 2017).
- 4. Taipale H, Tolppanen AM, Koponen M, et al. Risk of pneumonia associated with incident benzodiazepine use among community-dwelling adults with Alzheimer disease. Can Med Assoc J 2017; 189: E519-E529.
- 5. Maust D, Kim H, Seyfried L, et al. Antipsychotics, other psychotropics, and the risk of death in patients with dementia. JAMA Psychiatry 2015; 72: 438-445.
- 6. Royal Australian College of General Practitioners. Benzodiazepines. 3.4. Older patients. In: Prescribing drugs of dependence in general practice, Part B. Melbourne: RACGP, 2015. http://www.racgp.org.au/your-practice/guidelines/drugs-of-dependence-b/3-contraindications-and-precautions-in-special-groups/34-older-patients/ (viewed Mar 2017).
- 7. Banerjee S. The use of antipsychotic medication for people with dementia: time for action. Department of Health (UK), 2009. https://www.rcpsych.ac.uk/pdf/Antipsychotic%20Bannerjee%20Report.pdf (viewed Mar 2017).
- 8. Snowdon J, Galanos D, Vaswani D. Patterns of psychotropic medication use in nursing homes: surveys in Sydney, allowing comparisons over time and between countries. Int Psychogeriatr 2011; 23: 1520-1525.
- 9. Center for Clinical Standards and Quality/Survey and Certification Group (Centers for Medicare & Medicaid Services, US Department of Health and Human Services). Update report on the National Partnership to Improve Dementia Care in Nursing Homes (S&C: 16-28-NH) [memorandum]. June 2016. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-16-28.pdf (viewed Mar 2017).
- 10. The Senate Community Affairs References Committee. Care and management of younger and older Australians living with dementia and behavioural and psychiatric symptoms of dementia (BPSD). Mar 2014. http://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/Dementia/Report/index (viewed Mar 2017).
- 11. Brooker D, Latham I, Evans S, et al. FITS into practice: translating research into practice in reducing the use of anti-psychotic medication for people with dementia living in care homes. Aging Ment Health 2016; 20: 709-718.
- 12. Westbury J, Jackson SL, Gee PR, et al. An effective approach to decrease antipsychotic and benzodiazepine use in nursing homes: the RedUSe project. Int Psychogeriatr 2010; 22: 26-36.
- 13. van der Spek K, Gerritsen D, Smalbrugge M, et al. Only 10% of the psychotropic drug use for neuropsychiatric symptoms in patients with dementia is fully appropriate. The PROPER I-study. Int Psychogeriatr 2016; 28: 1589-1595.
- 14. French S, Green, S, O’Connor D, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci 2012; 7: 38.
- 15. Ploeg J, Skelly J, Rowan M, et al. The role of nursing best practice champions in diffusing practice guidelines: a mixed methods study. Worldviews Evid Based Nurs 2010; 7: 238-251.
- 16. Australian Government Department of Health. Australian Statistical Geographical Standard Remoteness Areas (2011) locator. DoctorConnect [website]. http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/ASGSRA_locator (viewed Apr 2017).
- 17. Australian Institute of Health and Welfare. Residential aged care and home care 2014–15: supporting data. https://www.gen-agedcaredata.gov.au/Resources/Access-data/2015/December/Residential-aged-care-and-Home-Care-2014%E2%80%9315-suppo (viewed Mar 2017).
- 18. Ling T, Gee P, Westbury J, et al. An internet-based method for extracting nursing home resident sedative medication data from pharmacy packing systems: descriptive evaluation. J Med Internet Res 2017; 19: e283.
- 19. World Health Organization Collaborating Centre for Drug Statistics Methodology. ATC/DDD index: N. Nervous system. https://www.whocc.no/atc_ddd_index/?code=N (viewed Mar 2017).
- 20. Woods S. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry 2003; 64: 663-667.
- 21. Drug and Alcohol Services South Australia. Benzodiazepines: information for GPs. Aug 2014. http://www.sahealth.sa.gov.au/wps/wcm/connect/dbd6d500407749f193d6bb222b2948cf/Benzodiazepines+-+GPs+2017.pdf?MOD=AJPERES&CACHEID=dbd6d500407749f193d6bb222b2948cf&CACHE=NONE (viewed Mar 2017).
- 22. Westbury J, Gee P, Ling T, et al. Reducing the Use of Sedative medication in aged care facilities: implementation of the RedUSe' project into everyday practice. Full final report. Hobart: Australian Government Department of Health, Wicking Dementia Research and Education Centre, University of Tasmania, 2016. http://ecite.utas.edu.au/120987 (accessed Mar 2017).
- 23. Szczepura A, Wild D, Khan AJ, et al. Antipsychotic prescribing in care homes before and after launch of a national dementia strategy: an observational study in English institutions over a 4-year period. BMJ Open 2016; 6: e009882.
- 24. de Souto Barreto P, Lapeyre-Mestre M, Cestac P, et al. Effects of a geriatric intervention aiming to improve quality care in nursing homes on benzodiazepine use and discontinuation. Br J Clin Pharmacol 2015; 81: 759-767.
- 25. Yang Y, Chen T, Beazley B, et al. An audit of psychotropic medication monitoring in Australian aged care facilities [abstract]. Australasian Pharmaceutical Society of Australia, Brisbane, 5–7 December 2014; paper 132. http://apsa-online.org/files/2014ConferenceProceedings.pdf (viewed Mar 2017).
- 26. Smith A, Tett S. Improving the use of benzodiazepines: is it possible? A non-systematic review of interventions tried in the last 20 years. BMC Health Serv Res 2010; 10: 321.
- 27. Westbury J, Tichleaar L, Peterson G, et al. A 12-month follow-up study of “RedUSe”: a trial aimed at reducing antipsychotic and benzodiazepine use in nursing homes. Int Psychogeriatr 2011; 23: 1260-1269.





Abstract
Objective: To assess the impact of a multi-strategic, interdisciplinary intervention on antipsychotic and benzodiazepine prescribing in residential aged care facilities (RACFs).
Design, setting: Prospective, longitudinal intervention in Australian RACFs, April 2014 – March 2016.
Participants: 150 RACFs (with 12 157 residents) comprised the main participant group; two further groups were consultant pharmacists (staff education) and community pharmacies (prescribing data). Data for all RACF residents, excluding residents receiving respite or end-stage palliative care, were included.
Intervention: A multi-strategic program comprising psychotropic medication audit and feedback, staff education, and interdisciplinary case review at baseline and 3 months; final audit at 6 months.
Main outcome measure: Mean prevalence of regular antipsychotic and benzodiazepine prescribing at baseline, and at 3 and 6 months. Secondary measures: chlorpromazine and diazepam equivalent doses/day/resident; proportions of residents for whom drug was ceased or the dose reduced; prevalence of antidepressant and prn (as required) psychotropic prescribing (to detect any substitution practice).
Results: During the 6-month intervention, the proportion of residents prescribed antipsychotics declined by 13% (from 21.6% [95% CI, 20.4–22.9%] to 18.9% [95% CI, 17.7–20.1%]), and that of residents regularly prescribed benzodiazepines by 21% (from 22.2% [95% CI, 21.0–23.5%] to 17.6% [95% CI, 16.5–18.7]; each, P < 0.001). Mean chlorpromazine equivalent dose declined from 22.9 mg/resident/day (95% CI, 19.8–26.0) to 20.2 mg/resident/day (95% CI, 17.5–22.9; P < 0.001); mean diazepam equivalent dose declined from 1.4 mg/resident/day (95% CI, 1.3–1.5) to 1.1 mg/resident/day (95% CI, 0.9–1.2; P < 0.001). For 39% of residents prescribed antipsychotics and benzodiazepines at baseline, these agents had been ceased or their doses reduced by 6 months. There was no substitution by sedating antidepressants or prn prescribing of other psychotropic agents.
Conclusions: The RedUSe program achieved significant reductions in the proportions of RACF residents prescribed antipsychotics and benzodiazepines.
Trial registration: Australian New Zealand Clinical Trials, ACTRN12617001257358.