The known The tragic death of Phillip Hughes in 2014 challenged the perception that cricket is a safe sport.
The new 174 trauma-related deaths in cricket over 152 years were identified: 83 in organised settings, 91 in informal play. The number of fatalities appears to have dropped dramatically in the past 30 years, probably reflecting the adoption of helmets by batsmen and close-in fielders. All recent deaths were caused by chest and neck injuries.
The implications Fatal injuries resulting from direct trauma in cricket are rare in Australia. Continued investigation of chest and neck protection is important for preventing further fatalities.
Cricket is a sport enjoyed around the world in different formats, from international matches to informal play in backyards and on beaches. Cricket has long been considered a safe, low risk sport from which many people derive the benefits of physical activity. At its top level, bowlers deliver a leather ball to batsmen at speeds of more than 140 km/h from a distance of 20 metres. In informal matches, the delivery pace is substantially slower, but the pitch and ground conditions can make the trajectory more difficult to predict.
In 2014, the death of Australian Test cricketer Phillip Hughes during a state level match focused attention on the risks inherent to cricket. Reaction at the time assumed that the death was a “freak accident” or a “one in a million” event, although cursory newspaper research found that cricket deaths occurred with some regularity.1 Nevertheless, there has been no extensive long term documentation of deaths in cricket in any country where it is a major sport.
A recent article described five cricket-related deaths in a case series of 36 severe craniofacial injuries.2 In Australia, a report of significant injuries in cricket, based on insurance claims during 2004–2013,3 documented 19 deaths in community level cricket, including 15 cardiac arrests, two caused by lightning strikes, and two of unspecified causes, making it unclear whether there were any traumatic cricket-related deaths (ie, direct effects of participation) in Australia during this decade.
A comprehensive review of fatalities in cricket is required to better understand the risks involved in participation. Similar to the World Health Organization model of disease surveillance, preventing sports injuries begins by knowing the number of injuries (or, in this case, deaths) and how they occur.4 With this information, preventive measures, such as rule changes and equipment or training programs, can be designed to moderate the identified risk factors. We therefore undertook a historical review of direct trauma-related deaths in Australian cricket.
Methods
We undertook an extensive search for details of cricket fatalities, primarily focusing on print media reports. Multiple searches of digitised newspapers (Trove [trove.nla.gov.au/newspaper], Australian Newspapers [newspapers.com.au], Fairfax Media), and biomedical journal databases (PubMed, SPORTDiscus) were performed during December 2014 – December 2016, and a request for information was published in Fairfax Press newspapers on 26 March 2016.
Cases were included if a fatality was directly related to participation in a cricket match or training as a player, official, or spectator. We excluded cases in which the deceased had died while travelling to or from cricket, and cases in which death was attributed to non-traumatic medical causes (eg, heart attack), violence, or lightning strike.
The searches included combinations of terms, with “killed by cricket ball”, “fatal accident cricket”, and “cricket fatality” identifying most cases. We also searched for “cricket death”, “cricketer killed”, “cricketer dies”, “batsman killed”, “umpire killed”, “fielder killed”, “spectator killed”, “tragic accident cricket”, “death on cricket field”, “fractured skull cricket”, “hit by cricket ball”, “cricketer struck on head”, “cricketer hit on head”, “cricketer struck” or “hit on chest”, and “cricketer dead”. In addition, we searched for the terms “inquest cricket” and “coroner cricket”. We specifically searched for coroner’s reports on Trove, as these reports yielded the most reliable accounts of the incidents.
We recorded information about the date and location of the incident, the age of the deceased and the level of cricket they were playing, and the circumstances of the incident, including the type of cricket being played (organised match or practice, informal), the activity being undertaken (batting, fielding, umpiring, watching), the site of the blow (head, neck, chest), whether the player was wearing protective equipment, and the subsequent clinical history (eg, died at ground, died later in hospital).
We performed a secondary review of the National Coronial Information System (NCIS; for 2001–2016) to identify cases not identifiable in the media.
Ethics approval
Ethics approval for accessing NCIS data was obtained from the Federation University Human Research Ethics Committee (reference, C16-004) and the Justice Human Research Ethics Committee (reference, CF/16/8934).
Results
We obtained details of 174 deaths, the first being in 1858 and the most recent the death of Hughes in 2014 (online Appendix). Ages ranged from a young baby to a 78-year-old umpire. The numbers of deaths, separated into those related to organised and informal play, increased until the 1930s and 1940s, and steadily declined from the 1950s (Box 1). No additional cases were identified in the NCIS database. Only three deaths have been recorded since 2000. There were 83 deaths in organised matches or training and 91 in informal settings (31 while playing in a schoolyard and 60 in backyard, street, or beach cricket games).
As the data for fatalities in organised settings are more complete, we restricted further analysis to these cases. Of 83 deaths caused by trauma during organised cricket, 62 injuries (75%) occurred in official club matches (Box 2). There were also five deaths in “social matches”, three in school matches, and 13 deaths at club practice or practice matches. All but one of the 83 deceased were male (including seven aged 14 years or less); one woman sustained fatal abdominal injuries after being struck by the ball during a women’s match.
Of the 83 people who died from injuries sustained during organised cricket — the first in 1864, the most recent the death of Philip Hughes in 2014 — details of their activity at the time of the injury were available for 72. Forty-five were batsmen (Box 3), of whom 28 died from injuries caused by a ball to the head (temple, forehead, or face), to the side of the head, below or behind the ear, or on the neck (Box 4).
The second most common cause of fatal cricket-related injuries to batsmen was a direct blow to the chest (13 deaths), presumably causing commotio cordis. Nine of the 13 batsmen killed in this manner were under 25 years of age. Deaths from subarachnoid haemorrhage following vertebral artery dissection (VAD/SAH) have only been confirmed by autopsy in two cases, but the clinical history for at least four further cases (classified as “head injury”) were consistent with this diagnosis; there was also cause for suspicion in a further seven cases. Three batsmen died of peritonitis following a blow to the abdomen, while another developed tetanus after an arm fracture.
Eleven fieldsmen died, five following collisions with other fielders or the boundary fence (three during games and two at practice) and six after being struck by balls during matches or practice. One bowler was killed when struck by a ball at practice. Six wicketkeepers were fatally injured during matches, four after being struck on the head by balls delivered by bowlers and one by a ball returned by a fielder; one died after being struck by a bat during the batsman’s follow-through (Box 3).
Three spectators were fatally injured, two watching matches and one watching practice; in addition, one bystander was struck by a ball from a nearby ground. Three umpires have died during matches after being hit in the head: one at square leg, one by a ball thrown by a fielder, and one by a ball straight driven by a batsman. Finally, two players preparing the pitch for play were killed when stuck by wayward balls from teams that were warming up (Box 3).
In the past 30 years, three of the five confirmed cricket-related deaths, all of batsmen, were attributed to commotio cordis and two to VAD/SAH; there have been no deaths linked with head injuries.
Discussion
While cricket has generally been regarded as a safe sport, there have been a surprisingly large number of fatalities directly associated with the game. The reported deaths were fairly evenly spread among organised games and training and informal play, including school play and backyard and street cricket. Most deaths in organised cricket (45 of 72 for which details were available) were of batsmen. The clearest finding of our study was the reduction in the number deaths after the 1950s, particularly since 1980.
The major sources of information for this investigation were newspaper articles. Many of Australia’s major metropolitan, suburban and country newspapers are digitised and available on the Trove website, but copyright legislation restricts coverage after mid-1954. We identified 146 deaths to 1954 in Trove. Twenty-eight cricket fatalities were identified in other digitised newspaper resources and with internet search engines, and as the result of a public appeal in the Fairfax press for information.
Media files have been used as a primary data source by the United States-based National Centre for Catastrophic Sport Injury Research (www.nccsir.edu.nc). Media-based investigations have been most thoroughly undertaken for boxing and baseball; the Manuel Velazquez collection has documented nearly 2000 boxing-related deaths,5 and baseball deaths are comprehensively documented in Death at the ballpark. A comprehensive study of game-related fatalities of players, other personnel and spectators in amateur and professional baseball, 1862–2007.6 As with our series, these publications were based on details of deaths obtained from media sources, primarily newspapers.
There are several possible explanations for the reduced numbers of cricket-related fatalities since the 1950s. We may not have identified all cricket-related deaths; some may have been missed because of our more limited access to newspaper articles published after 1954. Although not all newspapers after this date have been digitised, we had access to electronic versions of a number of major titles. We are confident that internet searches will have identified all relevant deaths during the past decade, as significant public interest for sports-related deaths ensures that cases are likely to be reported in some form of media.7
Our data are consistent with those reported by other studies. A 10-year retrospective analysis of 19 740 autopsies in New South Wales during 2006–2015 reported five cricket-related deaths: four were cardiac disease-related and therefore not included in our study, and the fifth was the 2014 Hughes death (personal communication: John Orchard, University of Sydney, January 2018). An Australian Institute of Health and Welfare report on 36 237 sport-related hospitalisations during the 12-month period 2011–12 included 913 related to playing cricket, but there were no deaths.8 Finally, our review of cases in the NCIS database found no additional cricket-related deaths during 2001–2015.
The decline in the number of fatalities since the 1980s parallels the rise of the widespread use of helmets by batsmen. Prior to the 1980s, batsmen generally played without head protection, and the most common cause of cricket-related death was being struck on the head. Helmets were introduced at the professional level during the 1980s, and they were also widely adopted at higher levels of club cricket and in all junior cricket. Close-in fielders have also worn helmets for the past two decades. In the 30-year period since the adoption of helmets, no deaths have been linked with head injuries, formerly the most common cause of death in cricket.
The reduced number of head injuries after the introduction of helmets for batsmen was noted in a study of junior cricketers in the Sutherland shire (NSW) which found that the frequency of head, neck and facial injuries to batsmen fell from 62% in 2002–03 to 35% in 2003–04, and to just 4% in 2004–05, after headgear became compulsory.9
In American baseball, head protection for batters has been required in the National League since 1956 and in the American League since 1958. Players were initially allowed to use inserts and liners in their caps, but helmets have been compulsory in the professional leagues since 1971. The authors of Death at the ballpark wrote that, “while helmets have not entirely eliminated deaths from beanings, they have dramatically reduced the number of fatalities”, and that “helmets were the most important piece of protective equipment to be developed”.6
It is possible that improved medical management of head injuries contributed to reducing the numbers of deaths from blows to the head in cricket and baseball, but, were this the main explanation, a similar reduction in deaths from head injuries in other sports would also be expected. In boxing, the rate has remained steady after the number of deaths had steadily declined from the 1920s (233 deaths) to the 1970s (97 deaths).10 There has been no decline in the number of head trauma-related deaths in American football, which have been well documented over the past 50 years.11
After trauma to the head, the most common cause of death in cricket was a direct blow to the chest, with death presumably due to commotio cordis (Latin, “agitation of the heart”). The condition was first specifically described in 1876, when it was reported that a porter had died after the yoke he had been pulling snapped and he fell chest-first onto the ground.12
Most reports of commotio cordis are from the United States, largely as a result of the establishment of the National Commotio Cordis Registry in Minneapolis in 1995. A review of 224 cases recorded by the registry over its first 15 years indicated that the mean age of patients was 15 years (standard deviation, 9 years); 26% were under 10, and only 9% were 25 or older.13 We similarly found that most cricket-related deaths attributed to commotio cordis were of young people.
Primary prevention of commotio cordis in some sports has focused on chest protectors and vests.14-18 However, registry data indicate that the most popular commercially available protectors do not offer absolute protection from arrhythmia after a blow to the chest,14,19-21 with almost 20% of the cases of commotio cordis in competitive football, baseball, lacrosse and ice hockey involving people who had been wearing equipment marketed as protecting against traumatic chest injury.14,20-22 Chest protectors are not commonly used by cricketers except at the highest level, where batsmen face balls travelling at more than 140 km/h. The purpose of chest protectors in this context, however, is to protect the ribcage from fracture or bruising rather than against commotio cordis.
Phillip Hughes’ death drew attention to VAD/SAH as a potential cause of death in cricket. We identified one further confirmed case,23 and the description of the circumstances of a number of others previously classified as “head trauma” also suggested this diagnosis. Since Hughes’ death, a number of neck guards have been developed and trialled in an attempt to protect the neck area over the vertebral artery where Hughes was struck. These guards have not yet been adopted universally, but it is anticipated that they will eventually become part of the standard helmet.
Conclusion
We identified 174 deaths directly related to cricket over the past 152 years in Australia. The most striking feature of our findings was the reduced number of fatalities since helmets have been generally worn by batsmen and close-in fielders. It is likely that the introduction of helmets for batsmen and close-in fielders has reduced the incidence of deaths in cricket, and almost eliminated deaths from blows to the head causing intracerebral haemorrhage. In the past 30 years, three cricket-related deaths have been attributed to commotio cordis, two to VAD/SAH, and none to head injuries. Efforts to protect players, particularly batsmen, from commotio cordis and VAD/SAH should be undertaken.
Box 1 – Cricket-related fatalities in organised and informal settings, by decade
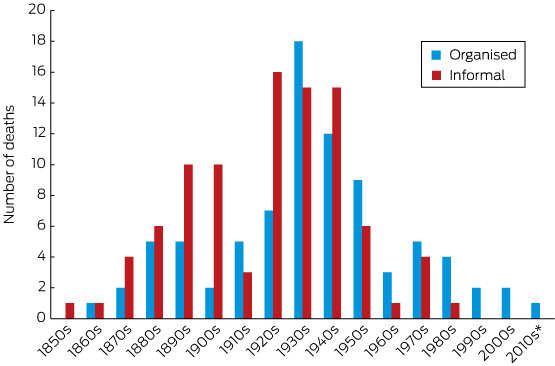
* For the period 2010–2016.
Box 2 – Cricket-related fatalities: type of cricket match
|
Type of cricket match |
Number of deaths |
||||||||||||||
|
|
|||||||||||||||
|
Organised cricket (total deaths: 83) |
|
||||||||||||||
|
Official matches |
62 |
||||||||||||||
|
Social matches |
5 |
||||||||||||||
|
School matches |
3 |
||||||||||||||
|
Practice/practice matches |
13 |
||||||||||||||
|
Informal cricket (total deaths: 91) |
|
||||||||||||||
|
School |
26 |
||||||||||||||
|
Home |
10 |
||||||||||||||
|
Park |
7 |
||||||||||||||
|
Street |
3 |
||||||||||||||
|
Beach |
1 |
||||||||||||||
|
Unknown |
44 |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 18 September 2017, accepted 8 December 2017
- Peter Brukner1
- Thomas J Gara2
- Lauren V Fortington3
- 1 La Trobe Sport and Exercise Medicine Research Centre (LASEM), La Trobe University, Melbourne, VIC
- 2 South Australian Museum, Adelaide, SA
- 3 Australian Centre for Research into Injury in Sport and its Prevention (ACRISP), Federation University Australia, Ballarat, VIC
We acknowledge the assistance of John Orchard with this study, and financial support from Cricket Australia. The Australian Centre for Research into Injury in Sport and its Prevention is one of the Research Centres for the Prevention of Injury and Protection of Athlete Health supported by the International Olympic Committee (IOC).
Peter Brukner was employed as the Cricket Australia team doctor during 2012–2017. Thomas Gara received funding for this study from Cricket Australia.
- 1. Bull A. Cricket has had too many “freak” deaths: players need better protection. The Guardian (Australian edition) 9 Dec 2014. https://www.theguardian.com/sport/2014/dec/09/cricket-freak-deaths-players-need-protection (viewed Dec 2017).
- 2. Tripathi M, Shukla DP, Bhat DI, et al. Craniofacial injuries in professional cricket: no more a red herring. Neurosurg Focus 2016; 40: E11.
- 3. Joseph C, Finch CF. The incidence of injury in Australian community level cricket players: a national overview of insurance claims from 2004–2013 (abstract). 5th World Congress of Science and Medicine in Cricket, 23-27 March 2015, Sydney; p. 40. http://slideslip.com/doc/79736/abstracts (viewed Dec 2017).
- 4. van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med 1992; 14: 82-99.
- 5. Svinth JR. Death under the spotlight: the Manuel Velasquez collection. Journal of Combative Sport [online]. Oct 2011. http://ejmas.com/jcs/velazquez/ (viewed Dec 2017).
- 6. Gorman RM, Weeks D. Death at the ballpark. A comprehensive study of game-related fatalities of players, other personnel and spectators in amateur and professional baseball, 1862-2007. Jefferson (NC): McFarland & Co., 2009.
- 7. Fortington LV, Bekker S, Finch CF. Online news media reporting of football-related fatalities in Australia: a matter of life and death. J Sci Med Sport 2017; doi:10.1016/j.jsams.2017.06.015 [Epub ahead of print].
- 8. Kreisfeld R, Harrison JE, Pointer S. Australian sports injury hospitalisations 2011–12 (AIHW Cat. No. INJCAT 168; Injury Research and Statistics Series No. 92). Canberra: Australian Institute of Health and Welfare, 2014.
- 9. Shaw L, Finch CF. Injuries to junior club cricketers: the impact of helmet regulations. Br J Sports Med 2008; 42: 437-440.
- 10. Baird LC, Newman CB, Volk H, et al. Mortality resulting from head injury in professional boxing: case report. Neurosurgery 2010; 67: E519-E520.
- 11. Boden BP, Breit I, Beachler JA, et al. Fatalities in high school and college football players. Am J Sports Med 2013; 41: 1108-1116.
- 12. Neélaton A. Éléments de pathologie chirurgicale. 2nd edition, volume 4. Paris: Librairie Germer Ballière et Cie, 1876.
- 13. Maron BJ, Estes NAM. Commotio cordis. N Engl J Med 2010; 362: 917-927.
- 14. Doerer JJ, Haas TS, Estes NAMI, et al. Evaluation of chest barriers for protection against sudden death due to commotio cordis. Am J Cardiol 2007; 99: 857-859.
- 15. Drewniak EI, Spenciner DB, Crisco JJ. Mechanical properties of chest protectors and the likelihood of ventricular fibrillation due to commotio cordis. J Appl Biomech 2007; 23: 282-288.
- 16. Janda DH, Viano DC, Andrzejak DV, et al. An analysis of preventive methods for baseball-induced chest impact injuries. Clin J Sport Med 1992; 2: 172-179.
- 17. Link MS, Bir C, Dau N, et al. Protecting our children from the consequences of chest blows on the playing field: a time for science over marketing. Pediatrics 2008; 122: 437-439.
- 18. Viano DC, Andrzejak DV, Polley TZ, et al. Mechanism of fatal chest injury by baseball impact: development of an experimental model. Clin J Sport Med 1992; 2: 166-171.
- 19. Maron BJ, Doerer JJ, Haas TS, et al. Commotio cordis and the epidemiology of sudden death in competitive lacrosse. Pediatrics 2009; 124: 966-971.
- 20. Maron BJ, Gohman TE, Kyle SB, et al. Clinical profile and spectrum of commotio cordis. JAMA 2002; 287: 1142-1146.
- 21. Maron BJ, Poliac L, Kaplan JA, et al. Blunt impact to the chest leading to sudden death from cardiac arrest during sports activities. N Engl J Med 1995; 333: 337-342.
- 22. Kaplan JA, Karofsky PS, Volturo GA. Commotio cordis in two amateur ice hockey players despite the use of commercial chest protectors: case reports. J Trauma 1993; 34: 151-153.
- 23. Opeskin K, Burke MP. Vertebral artery trauma. Am J Forensic Med Pathol 1998; 19: 206-217.





Abstract
Objective: To undertake a historical review of direct trauma-related deaths in Australian cricket, both organised and informal.
Design, setting and participants: We conducted an extensive search of digitised print media (three databases) and traditional scientific literature (two databases) for on-field cricket incidents in Australia that resulted in deaths during the period 1858–2016.
Main outcomes and measures: Numbers of cricket-related deaths by decade; type of cricket match (organised match or training, or informal play); site of fatal injury (eg, head, chest); activity at the time of the incident (eg, batting, fielding, watching).
Results: 174 relevant deaths were identified. The number peaked in the 1930s (33 fatalities), with five deaths in the past 30 years. There were 83 deaths in organised settings, and 91 deaths in informal play (at school, 31; backyard, street or beach cricket, 60). Of the 72 deaths in organised settings for which the activity of the deceased was reported, 45 were batsmen, 11 were fielders, six were wicketkeepers, one a bowler, and three were umpires. Of the 45 batsmen, 26 died of injuries resulting from a blow by a ball to the head, 13 of blows to the chest, three of peritonitis, at least two of vertebral artery dissection, and one of tetanus. None of the five cricket-related deaths over the past 30 years were caused by head injuries.
Conclusions: There appears to have been a substantial decline in the number of cricket-related deaths in recent years, probably linked with the widespread use of helmets by batsmen and close-in fielders.