The known Rates of severe mental illness and substance use among homeless people in large cities are high.
The new We confirmed that mental illness and substance use is common among homeless people attending mental health clinics at three Sydney homeless hostels. We could broadly distinguish between recently homeless and the more disabled chronically homeless people. 21% of attenders had lost a public housing tenancy.
The implications The homeless generate health and other costs that probably exceed the cost of providing suitable housing. More emergency housing for the temporarily homeless is needed, as well as a new model of supported units for the chronically homeless.
Studies of homeless people in inner city Sydney1-3 and other Australian cities4,5 have identified high rates of serious mental illness and substance use disorders. Further investigation is warranted by changes in the circumstances of vulnerable Australians — including the cost and availability of housing, patterns of substance use, and changes in mental health services — that may have influenced the reasons for becoming homeless and the characteristics of the homeless population.
Mental illness and homelessness are strongly associated, both because the social disability resulting from severe mental illness can affect the capacity to find and retain accommodation, and because being homeless adversely affects mental and physical health.5 Studies conducted in Sydney, the most recent of which was published in 2003,2 have found that between 11% and 36% of homeless people had a diagnosis of schizophrenia.1-3,6 Another study found that about 70% of homeless men had a substance use disorder,3 of whom more than half had a comorbid psychiatric disorder.7 A study of homelessness in Melbourne identified five major contributing factors to becoming homeless: a psychiatric disorder, domestic violence, substance misuse, a housing crisis, and adolescence.8 Other studies have emphasised the effect of combinations of psychiatric disorder, substance use, and social circumstances.9,10
The aims of our study were to describe the characteristics of a large cohort of patients seen at the mental health clinics of three inner city hostels for the homeless, and to investigate the reasons these people became homeless.
Methods
We report findings for a consecutive sample of people presenting to mental health clinics at the three large homeless hostels in inner city Sydney: the Matthew Talbot Hostel (run by the Society of St Vincent de Paul), Edward Eager Lodge (run by the Wesley Mission), and Foster House (run by the Salvation Army).
The Matthew Talbot Hostel provides overnight accommodation for 98 men in single rooms and eight-bed dormitories, as well as providing meals, clothing, and health care facilities for up to 250 men each day, many of whom live in the open. The hostel clinic dispenses medications (most frequently psychotropic medication) to about 100 men each day. Edward Eagar Lodge provides accommodation for 63 men and 13 women, and provides a mental health clinic that serves hostel residents and people referred by other agencies. Foster House has 97 beds and a general practice and psychiatric clinic. People can refer themselves to the clinic, or be referred by hostel staff, by welfare services in the hostels, or by external agencies, including hospitals, emergency departments, and parole officers.
Socio-demographic and clinical information was extracted from the records of assessment and ongoing care of a consecutive series of patients who presented to the clinics of one or more of the homeless hostels between 21 July 2008 and 31 December 2016. Socio-demographic variables included age, sex, employment history, marital status, social security benefits received, financial management order, forensic history, history of sleeping in the open, duration of homelessness, and history of losing a public housing tenancy. Clinical variables included psychiatric diagnosis, currently prescribed psychotropic medication, adherence to medication, pattern of symptoms, past psychiatric hospital admissions, presence of documented cognitive impairment, presence and nature of substance use disorder, and history of childhood or adult trauma.
The reasons for becoming homeless, the duration of homelessness, and the number of previous episodes of homelessness according to clinic notes were recorded both in a narrative account and by categorical ratings. The data collected thus comprised both quantitative data, because of the large number of individual patients, and qualitative data, because some of the data collected for each patient reflected judgements by the clinicians performing the assessment.
Conflicting data in duplicate entries from multiple assessments and other ambiguous data points were scored as 0 for binary variables. The data were analysed by compiling a table of frequencies of the main clinical and social variables. Sixteen variables were chosen a priori (by ON), based on clinical experience, for entry into a two-step cluster analysis, the aim of which was to identify as yet unrecognised groups of homeless people attending the clinics. The cluster analysis applied a log-likelihood method and the Schwarz Bayesian information criterion, without specifying the number of clusters.
We also analysed a hierarchical selection of patients based on the chronicity of homelessness, because the cluster analysis found that chronic homelessness was associated with greater disability and comorbid psychosis, and that more recent homelessness was associated with release from prison, discharge from hospital, and loss of a public housing tenancy.
Analyses were performed in SPSS Statistics 24 (IBM).
The relationships between people diagnosed with psychotic illness, those who had substance misuse problems, and patients who were chronically homeless (defined as being homeless for more than one year) were summarised in a Venn diagram.
Ethics approval
Approval to conduct this study was obtained from the St Vincent’s Hospital Human Research Ethics Committee (SVH file number, 11/180).
Results
General and mental health characteristics
The sample comprised 2388 individual patients (men: 2232, 93.4%) with a mean age of 42.3 years (standard deviation [SD], 12.8 years). Data for the sample were near complete for the variables of interest, with missing data items for less than 1% of the sample. Most people (1587, 66.1%) had a current diagnosis of substance use disorder, and half (1222, 51.2%) had been diagnosed with a psychotic illness, typically schizophrenia. Other common psychiatric diagnoses included acquired brain injury (345, 14.4%) and intellectual disability (119, 5.0%). A history of early life or recent trauma was reported by 42% of the sample, and by 35.5% of those with a diagnosis of psychosis. More than half the sample (1398, 58.8%) had been homeless for more than a year, and about one-third (824, 34.5%) reported sleeping in the open. There was a large overlap between chronic homelessness and having a diagnosis of psychosis or substance use disorder (Box 1).
Cluster analysis of the main patterns of homelessness
A two-step cluster analysis of the factors associated with homelessness identified two clusters of similar size. The first included people who were less likely to have been homeless for more than a year, and more likely to have ever been married and employed than those in the second cluster. Those in the second group were more likely to have been chronically homeless, were much more likely to be receiving a disability support pension, to have a diagnosis of psychotic illness, and to sleep in the open. The clusters did not differ significantly with regard to age, sex, or rates of substance use, gambling problems, or previous imprisonment (Box 2).
Pathways to homelessness
A hierarchical classification of the main pathways to homelessness confirmed that large proportions of clinic attenders who were chronically homeless had diagnoses of comorbid psychotic illness or substance use disorder. Recent release from prison, discharge from a psychiatric hospital, and loss of public housing tenancy were recorded for about half of all those who had recently become homeless (Box 3).
The proportion of patients recently released from prison with a substance use disorder was greater than for other attenders who had recently become homeless, but the people in this group were less likely to be receiving a disability support pension and far less likely to sleep in the open than the chronically homeless. The proportion diagnosed with psychotic illness was unsurprisingly higher among those recently discharged from a psychiatric hospital, and the proportion with a substance use disorder was smaller in this group than among the chronically homeless. The only marked features of the group of patients who had lost public housing tenancies were higher proportions of women and of people receiving disability pensions than in the other groups of recently homeless people (Box 3). Although not statistically significant, another pathway to homelessness involved financial problems arising from the salience of addictions, including addiction to illegal drugs and gambling, and also relationship crises resulting in the eviction of male partners (data not shown).
Discussion
Our study highlights the high prevalence of psychotic illness, substance use disorders, and the high proportion of chronically homeless people among patients attending psychiatric clinics in the three main homeless hostels in inner city Sydney.
Cluster analysis distinguished two groups of homeless clinic attenders with overlapping characteristics according to the severity of psychiatric disability and the chronicity of homelessness. Hierarchical analysis of the pathways to homelessness was dominated by the large number of clinic attenders who had been homeless for more than a year and more likely to have a comorbid disability.
Substance use and homelessness
A striking feature was the generally high rates of substance use disorders. A current diagnosis of a substance use disorder (other than nicotine dependence) was reported by 66.1% of patients, comparable with the rates found by previous studies.2,7 Substance use is both a cause and a consequence of homelessness. It can affect the ability to secure and maintain housing in a range of ways, particularly by diverting spending of the limited amount of available money from rent to alcohol and other drugs. Increased substance use can be a consequence of living in an environment where drugs are readily available, and peer pressure to participate is typical.7 Substance use may also be a coping mechanism for dealing with the challenges of homelessness. Continued substance use was a barrier to returning to stable accommodation for many patients, because of both the lack of money for rent and its effect on many patients’ organisational skills and other aspects of social performance. The relationship between substance use, mental illness, and homelessness is complex, but social disadvantage and exposure to substance-using subcultures predispose people to both mental illness and homelessness.2 Another factor is the cost of tobacco, as 85% of clinic attenders reported daily smoking, with some indicating they would prefer to sleep in the open to not having tobacco; an intervention to help clinic attenders stop smoking was not very successful.11 Substance use also contributes to the poor physical health12 and high rate of mortality13 in this population.
Psychotic illness and homelessness
The proportion of patients with a diagnosis of psychotic illness was higher than in other studies of homeless people,14-16 but our study was concerned with clinic attenders rather than homeless hostel residents or people sleeping in the open in general. However, there was a marked overlap between those diagnosed with psychotic illness and substance use disorder, and the proportions of people with psychotic illness among those released from prison and those reporting a history of trauma were also large, suggesting that the disabling effect of chronic psychotic illness is just one of several factors contributing to homelessness.
This finding confirms those of other studies which have shown that many patients with severe mental illness become homeless if not provided adequate psychosocial support.15 The finding that one-fifth of our sample had lost a public housing tenancy suggests that the social disability associated with severe forms of mental illness prevents many patients from maintaining tenancy without support. Moreover, the lack of secure and affordable housing continues to be a barrier to participation in both treatment and community life for people with severe mental illness, resulting in continued reliance on services for homeless people,17 indicating the need for stable housing as a prerequisite for adequate treatment of severe mental illness.18,19
Imprisonment and homelessness
More than one-quarter (28%) of recently homeless clinic attenders reported release from prison into homelessness, in part because of the high rate of offending associated with using illegal drugs, and the lack of social supports for many people released from prison. Ex-prisoners are more vulnerable to homelessness than the general population because of discrimination when attempting to secure accommodation, because there are long waiting lists, and because eligibility criteria for public housing can be difficult to satisfy.20 In addition, prisoners often lose accommodation through the breakdown of relationships or the loss of tenancy after arrest. The institutional setting can make it difficult for those completing long prison sentences to adjust to the demands of life in the community, including finding accommodation and accessing other services. Recidivism is higher among homeless former prisoners,20 possibly because of their increased visibility and contact with police while living in the open. Moreover, 5–7% of prisoners in New South Wales have schizophrenia,21 many of whom rotate between prisons and the homeless sector. Graded release and increased financial and psychological support around the time of release might reduce the rate of homelessness in this population, and also the rates of recidivism.22
Loss of public housing tenancy and homelessness
A somewhat surprising finding was the relatively high number of clinic attenders who had lost a public housing tenancy, as public housing has generally been viewed as a solution to homelessness. We did not explicitly examine the reasons for the loss of tenancy, but they included eviction because of disruptive behaviour related to substance use or mental illness, the exploitation of vulnerable tenants (often with a psychotic illness) by resuming or illegally subletting their flats, and imprisonment, as a tenancy is usually annulled after 3 months in custody. The homeless generate health and other costs that exceed the cost of providing housing, and there is a growing body of evidence supporting a Housing First strategy for improving outcomes and reducing the overall costs to society of caring for homeless people with mental illness.23
Limitations
One limitation of our study is that we examined a sample of clinic attenders, rather than a general sample of hostel residents or people sleeping in the open. However, the sample was drawn from three hostels with different cultures, and included many people who were not residing in the hostels. Another limitation was that two of the hostels only accepted men, so that homeless women were under-represented.24 A further limitation was that the data are largely based on self-reports by people from whom it was often difficult to elicit a reliable history. A data linkage study might provide a more accurate picture of the relationship between homelessness and contact with other agencies.
Conclusion and implications
We found that a high proportion of people attending clinics in Sydney homeless shelters were previously in either institutional care or in public housing, which suggests a failure of government policy in meeting the needs of people who are vulnerable to becoming homeless. The loss of what should be secure public housing tenancy reveals the need for more supported accommodation for people whose social skills are limited by severe psychiatric and intellectual disabilities. The numbers of people released from prison and psychiatric hospitals to homelessness indicate that better discharge and pre-release planning is needed.
Short term homelessness could probably be reduced by improving the supply of accessible low cost housing. Chronic homelessness of people with severe disability and comorbid conditions, however, requires a more comprehensive strategy that ensures continuity of psychiatric care, the treatment of substance use disorders, and a range of models for social support in order to improve this key indicator of the health of our society.
Box 1 – Overlap between the three key sample characteristics: diagnosis of psychosis, diagnosis of substance use disorder, and chronic homelessness
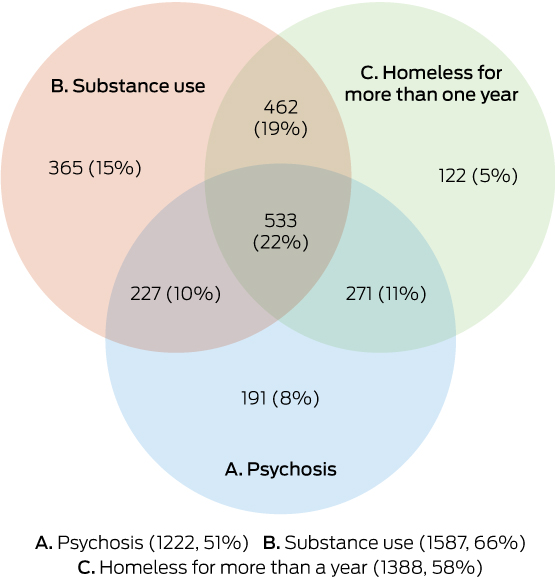
Total number of patients attending the clinics: 2388; number of people not included in A, B, or C: 217.
Box 2 – Cluster analysis of factors associated with homelessness
|
|
Total sample* |
Cluster 1 |
Cluster 2 |
||||||||||||
|
|
|||||||||||||||
|
Total number of people |
2388 |
1218 |
1159 |
||||||||||||
|
Sex (men) |
2232 (93.6%) |
1139 (94%) |
1082 (93%) |
||||||||||||
|
Age (years), mean (standard deviation) |
42.3 (11.1) |
41.7 (11.4) |
42.9 (10.7) |
||||||||||||
|
Current status |
|
|
|
||||||||||||
|
Homeless for more than one year |
1388 (58.5%) |
533 (44%) |
845 (73%) |
||||||||||||
|
Receiving disability support pension |
1330 (55.7%) |
209 (17%) |
1115 (96%) |
||||||||||||
|
Subject to financial management order (public trustee) |
186 (7.8%) |
11 (1%) |
167 (14%) |
||||||||||||
|
Sleeps in the open |
824 (34.5%) |
243 (20%) |
568 (49%) |
||||||||||||
|
Social history |
|
|
|
||||||||||||
|
Ever employed for more than one year |
1443 (60.4%) |
999 (82%) |
444 (38%) |
||||||||||||
|
Ever married |
817 (34.4%) |
589 (48%) |
224 (19%) |
||||||||||||
|
Lost public housing tenancy |
489 (20.9%) |
191 (16%) |
298 (26%) |
||||||||||||
|
Experienced trauma as child or adult |
1031 (42.2%) |
591 (49%) |
435 (38%) |
||||||||||||
|
Released from prison |
675 (28.3%) |
311 (24%) |
364 (31%) |
||||||||||||
|
Released from a psychiatric hospital |
507 (21.2%) |
158 (13%) |
346 (30%) |
||||||||||||
|
Mental health comorbidities |
|
|
|
||||||||||||
|
Psychotic illness |
1222 (51.1%) |
317 (26%) |
900 (78%) |
||||||||||||
|
Intellectual disability |
119 (5.0%) |
21 (2%) |
98 (8%) |
||||||||||||
|
Acquired brain injury |
345 (14.4%) |
125 (10%) |
217 (19%) |
||||||||||||
|
Current substance use disorder |
1587 (66.1%) |
818 (67%) |
761 (66%) |
||||||||||||
|
Problem gambling |
289 (12.1%) |
162 (13%) |
127 (11%) |
||||||||||||
|
|
|||||||||||||||
|
* Missing data points prevented allocating 11 people to either cluster. |
|||||||||||||||
Box 3 – Characteristics of homeless people attending the three clinics according to their pathways to homelessness
|
|
Homeless more than a year |
Homeless less than one year |
|||||||||||||
|
All recently homeless |
Release from prison |
Discharge from psychiatric hospital |
Loss of public housing |
Loss of other accommodation |
|||||||||||
|
|
|||||||||||||||
|
Total number of people |
1388 (58%) |
1000 (42%) |
210 |
121 |
207 |
462 |
|||||||||
|
Sex (men) |
1331 (96%) |
900 (90%) |
200 (95%) |
109 (90%) |
174 (84%) |
417 (98%) |
|||||||||
|
Age (years), mean (standard deviation) |
42.1 (10.6) |
41.2 (10.6) |
40.2 (9.8) |
39.3 (11.8) |
45.0 (11.7) |
42.7 (12.3) |
|||||||||
|
Current status |
|
|
|
|
|
|
|||||||||
|
Sleeps in the open |
721 (52%) |
93 (9%) |
22 (10%) |
16 (13%) |
21 (10%) |
34 (8%) |
|||||||||
|
Receiving disability support pension |
857 (62%) |
442 (44%) |
91 (43%) |
64 (53%) |
138 (67%) |
179 (42%) |
|||||||||
|
Subject to financial management order (public trustee) |
123 (9%) |
55 (6%) |
8 (4%) |
6 (5%) |
16 (8%) |
25 (6%) |
|||||||||
|
Social history |
|
|
|
|
|
|
|||||||||
|
Ever employed for more than one year |
770 (55%) |
673 (67%) |
139 (66%) |
72 (60%) |
123 (59%) |
339 (80%) |
|||||||||
|
Ever married |
389 (28%) |
425 (42%) |
97 (46%) |
38 (31%) |
94 (45%) |
196 (46%) |
|||||||||
|
Experienced trauma as child or adult |
618 (45%) |
413 (41%) |
91 (43%) |
41 (34%) |
86 (42%) |
195 (46%) |
|||||||||
|
Mental health comorbidities |
|
|
|
|
|
|
|||||||||
|
Psychotic illness |
804 (58%) |
418 (42%) |
87 (41%) |
81 (67%) |
99 (48%) |
151 (35%) |
|||||||||
|
Intellectual disability |
74 (5%) |
45 (4%) |
11 (5%) |
4 (3%) |
12 (6%) |
18 (4%) |
|||||||||
|
Acquired brain injury |
227 (16%) |
118 (12%) |
29 (14%) |
9 (7%) |
29 (14%) |
51 (12%) |
|||||||||
|
Current substance use disorder |
995 (72%) |
592 (59%) |
155 (74%) |
62 (51%) |
117 (57%) |
258 (61%) |
|||||||||
|
Problem gambling |
173 (12%) |
116 (12%) |
31 (15%) |
11 (9%) |
24 (12%) |
50 (12%) |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 31 August 2017, accepted 30 November 2017
- Olav B Nielssen1
- William Stone2
- Naidene M Jones2
- Sarah Challis3
- Amelia Nielssen4
- Gordon Elliott5
- Nicholas Burns5,6
- Astrid Rogoz7
- Lucy E Cooper2
- Matthew M Large8
- 1 Macquarie University, Sydney, NSW
- 2 Matthew Talbot Hostel, St Vincent de Paul, Sydney, NSW
- 3 Sydney Children's Hospital (Randwick), Sydney, NSW
- 4 University of Newcastle, Newcastle, NSW
- 5 Justice Health and Forensic Mental Health Network, Sydney, NSW
- 6 Bloomfield Hospital, Orange, NSW
- 7 St Vincent's Hospital, Sydney, NSW
- 8 University of New South Wales, Sydney, NSW
No relevant disclosures.
- 1. Doutney CP, Buhrich N, Virgona A, et al. The prevalence of schizophrenia in a refuge for homeless men. Aust N Z J Psychiatry 1985; 19: 233-238.
- 2. Teesson M, Hodder T, Buhrich N. Alcohol and other drug use disorders among homeless people in Australia. Subst Use Misuse 2003; 38: 463-474.
- 3. Teesson M, Hodder T, Buhrich N. Psychiatric disorders in homeless men and women in inner Sydney. Aust N Z J Psychiatry 2004; 38: 162-168.
- 4. Harvey C, Killackey E, Groves A, et al. A place to live: housing needs for people with psychotic disorders identified in the second Australian National Survey of Psychosis. Aust N Z J Psychiatry 2012; 46: 840-850.
- 5. Lee S, Castella A, Freidin J, et al. Mental health care on the streets: an integrated approach. Aust N Z J Psychiatry 2010; 44: 505-512.
- 6. Doutney C, Buhrich N, Virgona A, et al. The prevalence of schizophrenia in a refuge for homeless men. Aust N Z J Psychiatry 1985; 19: 233-238.
- 7. Teesson M, Hodder T, Buhrich N. Substance use disorders among homeless people in inner Sydney. Soc Psychiatry Psychiatr Epidemiol 2000; 35: 451-456.
- 8. Johnson G. On the move: a longitudinal study of pathways in and out of homelessness (PhD thesis). Melbourne: RMIT University, 2016. https://researchbank.rmit.edu.au/view/rmit:6220 (viewed Nov 2017).
- 9. Sullivan G, Burnam A, Koegel P. Pathways to homelessness among the mentally ill. Soc Psychiatry Psychiatr Epidemiol 2000; 35: 444-450.
- 10. Fowler PJ, Toro PA, Miles BW. Pathways to and from homelessness and associated psychosocial outcomes among adolescents leaving the foster care system. Am J Public Health 2009; 99: 1453-1458.
- 11. Power J, Mallat C, Bonevski B, et al. An audit of assessment and outcome of intervention at a quit smoking clinic in a homeless hostel. Australas Psychiatry 2015; 23: 528-530.
- 12. Nielssen O, Chudleigh A, Chen M, et al. Results of a metabolic health clinic at a hostel for homeless men. Australas Psychiatry 2017; 25: 270-273.
- 13. Babidge NC, Buhrich N, Butler T. Mortality among homeless people with schizophrenia in Sydney, Australia: a 10-year follow-up. Acta Psychiatr Scand 2001; 103: 105-110.
- 14. Buhrich N, Hodder T, Teesson M. Prevalence of cognitive impairment among homeless people in inner Sydney. Psychiatr Serv 2000; 51: 520-521.
- 15. Pearson GS, Linz S. Linking homelessness with mental illness. Perspect Psychiatr Care 2011; 47: 165-166.
- 16. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med 2008; 5: e225.
- 17. Gilmer TP, Stefancic A, Ettner SL, et al. Effect of full-service partnerships on homelessness, use and costs of mental health services, and quality of life among adults with serious mental illness. Arch Gen Psychiatry 2010; 67: 645-652.
- 18. Whittaker E, Swift W, Roxburgh A, et al. Multiply disadvantaged: health and service utilisation factors faced by homeless injecting drug consumers in Australia. Drug Alcohol Rev 2015; 34: 379-387.
- 19. Holmes A, Carlisle T, Vale Z, et al. Housing First: permanent supported accommodation for people with psychosis who have experienced chronic homelessness. Australas Psychiatry 2017; 25: 56-59.
- 20. Baldry E, McDonnell D, Maplestone P, Peeters M. Ex-prisoners, homelessness and the state in Australia. Aust N Z J Criminol 2006; 39: 1-14.
- 21. Nielssen O, Misrachi S. Prevalence of psychoses on reception to male prisons in New South Wales. Aust N Z J Psychiatry 2005; 39: 453-459.
- 22. Ventura LA, Cassel CA, Jacoby JE, et al. Case management and recidivism of mentally ill persons released from jail. Psychiatr Serv 1998; 49: 1330-1337.
- 23. Evans J, Collins D, Anderson J. Homelessness, bedspace and the case for Housing First in Canada. Soc Sci Med 2016; 168: 249-256.
- 24. Virgona A, Buhrich N, Teesson M. Prevalence of schizophrenia among women in refuges for the homeless. Aust N Z J Psychiatry 1993; 27: 405-410.





Abstract
Objective: To describe the characteristics of people attending mental health clinics at shelters for the homeless in inner city Sydney.
Design: Retrospective review of medical records of homeless hostel clinic attenders.
Setting: Mental health clinics located in three inner city homeless hostels.
Participants: Consecutive series of clinic attenders, 21 July 2008 – 31 December 2016.
Main outcome measures: Demographic characteristics; social, medical and mental health histories of homeless people.
Results: 2388 individual patients were seen at the clinics during the 8.5-year study period. Their mean age was 42 years (standard deviation, 13 years), 93% were men, and 56% were receiving disability support pensions. 59% of attenders had been homeless for more than a year, and 34% of all attenders reported sleeping in the open. The most common diagnoses were substance use disorder (66%), psychotic illness (51%), acquired brain injury (14%), and intellectual disability (5%). Most patients had more than one diagnosis. Early life and recent trauma was reported by 42% of patients. Pathways to homelessness included release from prison (28% of the homeless), discharge from a psychiatric hospital (21%), loss of public housing tenancy (21%), and inability to pay rent because of problem gambling.
Conclusions: The high rates of substance use and mental disorder among homeless people in inner Sydney confirms the need for increased access to treatment for these conditions in this setting. Homelessness among those with mental illness might be reduced by developing alternative housing models, and supporting people with multiple problems to retain tenancy.