Current information on the out-of-pocket costs incurred by Australians being treated for cancer is limited. We therefore investigated these costs for participants in the QSkin Sun and Health Study.1 Study participants diagnosed during November 2010 – November 2011 with histologically confirmed melanoma or cancer of the breast, prostate, colon/rectum, or lung were identified by linkage with Queensland Cancer Registry data. Linkage with Medicare data (for a minimum of 2 years from diagnosis) identified all services for consultations, tests, imaging, procedures, and pharmaceuticals billed through Medicare. Excluded were additional patient costs, such as travel, parking, and income lost through interruptions during work hours. The study was approved by the QIMR Berghofer Human Ethics Research Committee (reference, P1309).
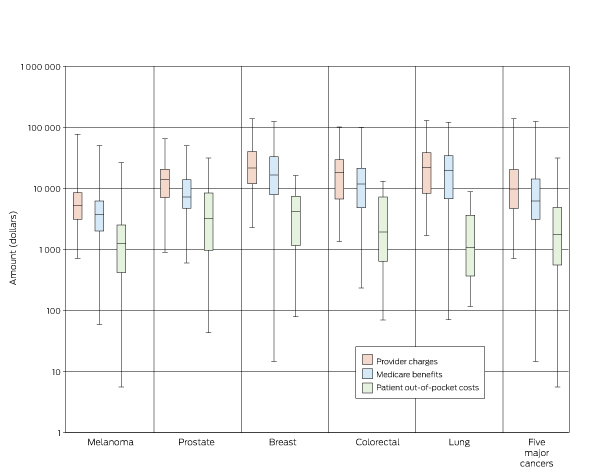
A total of 452 QSkin participants had a primary diagnosis of one of the five major cancers during the 12-month window: 200 with melanoma (44%), 114 with prostate cancer (25%), 84 with breast cancer (19%), 30 with colorectal cancer (7%) and 24 with lung cancer (5%). Over 2 years, total provider fees were highest for those with lung (median, $22 011; interquartile range [IQR], $8346–38 387) or breast cancer (median, $21 581; IQR, $11 982–40 350), and lowest for those with melanoma (median, $5248; IQR, $3132–8513). However, median out-of-pocket expenses were highest for patients with breast ($4192; IQR, $1165–7459) and prostate cancer ($3175; IQR, $971–8431) and lowest for participants with lung cancer ($1078; IQR, $367–3619) (Box). The median proportion of provider fees covered by Medicare subsidies was 63% (range, 51% [prostate cancer] to 89% [lung cancer]). The largest median out-of-pocket costs (five cancers) were for therapeutic procedures ($670; IQR, $0–2591), professional attendances ($414; IQR, $140–786) and medications ($288; IQR, $52–620). The median provider fee (five cancers) was $9821 (IQR, $4645–20 551); the median Medicare subsidy was $6280 (IQR $3342–14 768).
The finding of higher out-of-pocket costs for patients with breast cancer corroborates a recent report on nearly 2000 Australian women that included direct and indirect medical costs and found that three-quarters of the patients had incurred up to $17 200 in out-of-pocket expenses during the 5 years after diagnosis.2
We found that medical costs for patients with some types of cancer are high; one-quarter of these cancer survivors paid upfront doctors’ fees of more than $20 000 over 2 years. The consequences can be devastating for individuals experiencing financial hardship, including serious impacts such as delays of or non-adherence to therapy and increased morbidity.
It is difficult for individuals and their doctors to predict what co-payments are likely to be requested during cancer treatment. Private health insurance premiums continue to increase each year with rising provider fees, the introduction of new technologies, and increasing numbers of services per patient.3 The private health insurance rebate for the privately insured (costing $6.5 billion per year3), together with the Medicare benefits paid mean that the federal government continues to make substantial payments for insured individuals, money that might otherwise be re-directed to strengthening the public health system. Practical solutions for alleviating the financial burden on patients with cancer would include lower medical fees and greater transparency in charging.4,5
Received 21 August 2017, accepted 12 December 2017
- 1. Olsen CM, Green AC, Neale RE, et al. Cohort profile: the QSkin Sun and Health Study. Int J Epidemiol 2012; 41: 929-929i.
- 2. Deloitte Access Economics. Financial impacts of breast cancer in Australia [report for Breast Cancer Network Australia]. Nov 2016. https://www.bcna.org.au/media/5608/financial-impacts-of-breast-cancer-deloitte-access-economics.pdf (viewed Feb 2018).
- 3. Savage E. The multi-billion-dollar subsidy for private health insurance isn’t worth it. The Conversation 27 Apr 2017. https://theconversation.com/the-multi-billion-dollar-subsidy-for-private-health-insurance-isnt-worth-it-76446?sa=pg1&sq=Elizabeth+Savage&sr=2 (viewed Feb 2018).
- 4. Duckett S. Many Australians pay too much for health care — here’s what the government needs to do. The Conversation 13 July 2016. https://theconversation.com/many-australians-pay-too-much-for-health-care-heres-what-the-government-needs-to-do-61859?sa=pg1&sq=Duckett&sr=6 (viewed Feb 2018).
- 5. Doggett J. Out of pocket: rethinking health copayments. Sydney: Centre for Policy Development, 2009. https://cpd.org.au/wp-content/uploads/2009/07/Out-of-Pocket.pdf (viewed Feb 2018).





This study was supported in part by the National Health and Medical Research Council (552429). David Whiteman is supported by a fellowship from the National Health and Medical Research Council.
No relevant disclosures.