A kernel of wheat contains 8–15% of protein, of which 85–90% is gluten, in turn made up of glutenins and gliadins.1 Gluten gives wheat flour the culinary properties of a binding and extending agent which are valued in cooking.2 As a result, wheat is one of the most important worldwide crops.3 Storage proteins similar to gliadins have been found in rye (secalins) and barley (hordeins), while the avenins of oats are more distantly related.1,2 Coeliac disease is an immune-mediated systemic condition, manifest by small intestinal enteropathy triggered by exposure to dietary gluten in genetically predisposed individuals, almost all of whom have the human leucocyte antigen (HLA) haplotype DQ2 or DQ8.4,5 Coeliac disease is associated with diarrhoea, malabsorption, increased rates of autoimmune disease and gastrointestinal malignancies; however, most of these effects are ameliorated by treatment with a lifelong gluten-free diet.4
Coeliac disease, once considered rare, is now estimated to affect up to one in 100 Australians.6 However, many Australians are believed to monitor and limit their intake of gluten despite having no formal diagnosis of coeliac disease.6 Motivations to adopt a gluten-free diet include adverse symptoms attributed to ingestion, perceived benefits for weight control or general health, relatives on a gluten-free diet, or a preference for gluten-free products based on taste.7 Consequently, there has been rapid growth in the global gluten-free market, which has a current estimated United States market value of over $6 billion.8
An Australia-wide cross-sectional survey found that 7.3% of the population (with suspected and confirmed coeliac disease excluded) report adverse effects associated with gluten ingestion, including gastrointestinal symptoms such as bloating or abdominal discomfort, or extra-intestinal effects such as headache or tiredness.9 This is in line with similar studies from the US, Chile, United Kingdom and Europe that demonstrated a population prevalence of self-reported wheat or gluten sensitivity of between 4% and 13%.9-14 This suggests that a gluten-sensitive condition, separate to coeliac disease and wheat allergy, may be responsible for their symptoms. This condition has attracted increasing international attention and has been labelled non-coeliac gluten sensitivity.15 In this review, we present an overview of the epidemiology, diagnosis, pathogenesis and management of this disorder, based on a synthesis of relevant evidence from PubMed-listed articles until March 2017, including original research, consensus guidelines and opinion papers.
Gluten or wheat?
Gluten may not be wholly responsible for the condition, and non-coeliac gluten or wheat sensitivity (NCG/WS) could be a more accurate term. Wheat contains compounds other than gluten that may have adverse effects on the intestinal mucosa and contribute to gastrointestinal symptoms, and adoption of a gluten-free diet is likely to decrease the ingestion of these compounds. These include fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs), which are associated with precipitation of symptoms in the irritable bowel syndrome (IBS).16 A number of dietary trials have established low FODMAP diets as an effective treatment for patients with IBS.16 The mechanism is believed to relate to poor absorption of FODMAPs, which causes an increase in small bowel water content, colonic gas production and intestinal motility, leading to gastrointestinal symptoms.17 A low FODMAP diet has also been shown to attenuate symptoms of NCG/WS in patients with suspected gluten sensitivity.18 Other potentially pathogenic compounds in wheat include amylase trypsin inhibitors, which have been shown to induce inflammation in duodenal biopsies of patients with coeliac disease in vitro,19 and wheat germ agglutinin, which has been shown to induce inflammation in epithelial cells in vitro.20 These may represent alternative pathways by which wheat-based foods cause gastrointestinal symptoms.
Diagnosis and epidemiology
Diagnosis of NCG/WS is currently based on the Salerno experts’ criteria, and can only be made after exclusion of coeliac disease and wheat allergy (by negative serology and duodenal biopsy, and serum or skin prick IgE-specific tests, respectively) followed by a labour-intensive double-blind crossover dietary challenge (Box 1).21 Those who report an improvement in symptoms on a gluten-free diet are given a blinded challenge of gluten (ideally free of FODMAPs and in a dose of at least 8 g/day) and placebo foodstuff each over a period of one week, followed by a one-week washout.21 Only those whose symptoms recur with gluten challenge but not with placebo are labelled as having NCG/WS (Box 2). A recent systematic review of randomised trials that made a diagnosis of NCG/WS by this method (a total of 231 adults) showed that only 16% of patients who report improvement of their symptoms with a gluten-free diet will actually have reproducible gluten-specific symptoms when strict diagnostic criteria are applied.22
Notably, there is also a strong nocebo response with the placebo challenge trial, making interpretation of the current diagnostic method difficult (40% of subjects reported similar or more symptoms on ingestion of placebo compared with gluten in double-blind randomised controlled trials in the previously mentioned systematic review).22 This suggests that multiple challenges with each of gluten and placebo may be required to confidently diagnose subjects with NCG/WS.23,24 Nevertheless, regarding the prevalence of this condition, it is likely that only a small proportion of Australians who associate adverse symptoms with gluten ingestion are truly sensitive to gluten or wheat. Little is known about the incidence of this disorder.
Clinical features
In people confidently diagnosed with NCG/WS, wide-ranging symptoms have been reported. These include gastrointestinal complaints such as bloating, abdominal or epigastric pain, diarrhoea and nausea.25 In this regard, there is thus a strong overlap between NCG/WS and functional gastrointestinal disorders such as IBS and functional dyspepsia.26 Extra-intestinal symptoms have also been reported, including a lack of wellbeing, tiredness and headache and, less commonly, anxiety, “foggy mind”, joint pains, rash, depression and rhinitis.25 Symptom onset is usually hours to days after gluten or wheat ingestion.25,27 Studies have reported that only 50–55% of patients with NCG/WS had previously associated their symptoms with wheat or gluten ingestion and had presented with functional gastrointestinal symptoms.25,27
NCG/WS predominantly affects females (the female:male ratio is > 5:1) in their late 30s and 40s.25 The disorder also been associated with low bone mineral density,28 anaemia and weight loss,27 which suggests that in some patients, malabsorption may be present. Patients are also more likely to have a family history of coeliac disease, a history of food allergy in infancy, coexistent atopic disease,27 an increased prevalence of autoimmune disease such as Hashimoto’s thyroiditis and high levels of circulating antinuclear antibodies,29 suggesting overlap with other autoimmune and allergic diseases. Recent epidemiological research has similarly identified an increased risk of autoimmune and rheumatological disease in functional gastrointestinal disorders, further supporting the concept of overlap with NCG/WS.30
Pathogenesis
The pathogenesis of NCG/WS is not well understood; however, early studies suggest that the innate immune system is involved (compared with the adaptive Th1 response seen in coeliac disease), with increased intestinal permeability,31 epithelial cell damage,32 increased expression of Toll-like receptors,33 and interferon-γ expression34 (Box 3). Toll-like receptors on epithelial cells are important in the innate immune response to microbial pathogens, and it is possible that an altered intestinal microbiome is involved in NCG/WS, although experimental evidence is lacking.35 Duodenal and colonic eosinophilia has also been observed in patients with NCG/WS presenting with IBS-type symptoms.27 Notably, duodenal eosinophilia has also been observed in a major subset of patients with the post-prandial distress syndrome subtype of functional dyspepsia presenting with early satiety or post-prandial fullness.36 It is conceivable that one of the underlying explanations for this finding in functional dyspepsia is food intolerance and wheat may play a role.36 A limited role of the adaptive immune system has also been proposed, with increased interferon-γ-producing type 1 innate lymphoid cells demonstrated in the rectal mucosa of NCG/WS patients in response to wheat challenge when compared with IBS controls.37 Despite these early reports, there are still no clearly accepted pathological hallmarks of NCG/WS, nor are there any serological tests or associated enzyme deficiencies, making diagnosis of this syndrome difficult and reliant on a cumbersome dietary trial.21
Unlike in coeliac disease, there is no clear genetic predisposition in NCG/WS. The HLA DQ2 or DQ8 haplotypes, present in almost all patients with coeliac disease, do not seem to be strongly associated with NCG/WS, with a prevalence similar to that seen in the general population (about 40–50%).4,27,38 While endomysial and tissue transglutaminase (tTG) antibodies are not associated with NCG/WS (highly sensitive and specific tests, which when positive suggest a diagnosis of coeliac disease), anti-gliadin antibodies are found in about 50–60% of patients diagnosed with NCG/WS, prompting some authors to suggest it could be used as a diagnostic marker.4,21,27,39 However, these antibodies are neither sensitive nor specific, and are found in low titres in the healthy population, as well as in patients with other disorders including coeliac disease, cow’s milk intolerance and inflammatory bowel disease, and may represent markers of impaired barrier function rather than a harmful food antigen.24,40 Lymphocytic duodenosis is commonly seen in coeliac disease and in up to 90% of patients with non-coeliac gluten sensitivity,27,41,42 although this is a non-specific finding seen in up to 5% of all duodenal biopsies with normal villous architecture, and can also be caused by infections such as Helicobacter pylori, drugs such as non-steroidal anti-inflammatories, and autoimmune disease (Box 3).43,44
Given the known overlap between coeliac disease and NCG/WS, it is likely that a proportion of patients fulfilling current criteria for NCG/WS have coeliac disease but that the diagnosis has not been confirmed. There are several potential explanations. First-line coeliac disease serology with anti-tTG can be negative if subjects are already on a gluten-free diet (or are inadequately challenged with gluten before biopsy),45 or are IgA deficient (although testing for IgA levels and IgG anti-tTG is now common practice). The enteropathy in coeliac disease is patchy, and insufficient biopsy sampling may miss disease.46,47 Also, mild enteropathy (duodenal lymphocytosis) may be interpreted as a non-specific finding in the context of negative serology, but may represent coeliac disease (Box 3).46,47 This has led to the proposal of an incompletely developed form of coeliac disease referred to as “coeliac-lite” syndrome by some authors.24,41 Rosinach and colleagues48 studied a group of patients with negative coeliac disease serology (IgA anti-tTG and anti-endomysial antibodies) but positive HLA DQ2 or DQ8 status, lymphocytic duodenosis on duodenal biopsy, and gastrointestinal symptoms, with clinical and histological remission on a gluten-free diet at inclusion. The patients underwent a blinded, placebo-controlled gluten challenge: 91% (95% CI, 62–98%) of patients in the gluten arm had symptom relapse versus 28.5% (95% CI, 8–64%) in the placebo arm (P < 0.01), supporting a diagnosis of NCG/WS as the definition stands. However, the authors showed that 50% of these subjects demonstrated mucosal anti-tTG deposits and a high γδ intra-epithelial cell count, highly sensitive markers for the diagnosis of coeliac disease.49 This suggests that a subset of patients meeting criteria for NCG/WS have subclinical coeliac disease.50 In much of the literature regarding NCG/WS, these tests have not been done to fully exclude subclinical coeliac disease, making interpretation of the field difficult.41 The potential pathogenic mechanisms are outlined in Box 4.
Treatment
As with coeliac disease, NCG/WS is treated with a gluten-free diet.21 However, unlike in coeliac disease where inadvertent or small amounts of gluten can lead to enteropathy and malabsorption, there is no evidence for benefit in NCG/WS beyond symptom relief, and strict complete exclusion may not be necessary.15 Identification of individuals who are truly sensitive to gluten or wheat is important given that committing a patient to a gluten-free diet has several drawbacks. A recent Australian study suggested that a gluten-free diet was 5.8–16.7% more expensive than a regular diet.51 The diet also has potentially adverse effects on health. Gluten-free products are not necessarily equivalent to their gluten-containing counterparts regarding their macronutrient and micronutrient content. Several studies have demonstrated that gluten-free diets may not provide adequate amounts of trace elements and vitamins such as calcium, vitamin D, folate, thiamine, riboflavin and niacin.52-54 This translates to clinical studies which have demonstrated high rates of micronutrient deficiencies, such as folate and vitamin B in patients treated with a gluten-free diet.52,54 The diet also differs in regards to protein55 and fat54,56 content, although accounts vary in regards to the specific breakdown. A gluten-free diet may adversely affect cardiovascular risk factors such as total cholesterol levels,57 weight gain leading to obesity,57 glucose tolerance57 and blood pressure58 and may lead to development of the metabolic syndrome.58 A potential explanation for this is the higher glycaemic load of gluten-free foods.54,59 Again, accounts vary, with other studies demonstrating a potentially beneficial effect of a gluten-free diet on cardiovascular risk factors, for instance by increasing serum high-density lipoprotein levels.57,60 A gluten-free diet may lead to exposure to toxins, with recent reports of high levels of arsenic being found in the urine of patients who self-reported adherence to a gluten-free diet.61 This may be due to the high arsenic content of rice and rice flour, often a substitute for wheat in gluten-free products.62 Many of these observations are limited to studies in patients with coeliac disease who are on a gluten-free diet, and there is less in the literature regarding the health effects of a gluten-free diet in patients with NCG/WS. A gluten-free diet has also been shown to influence the intestinal microbiome, with a reduction in Veillonellaceae, a pro-inflammatory bacterial genus, after treatment with a gluten-free diet.63 Other changes described include decreases in the normal Bifidobacterium and Lactobacillus species, as well as an increase in Enterobacteriaceae species.64
Current research and future directions
NCG/WS is a controversial disorder which potentially affects a significant proportion of the population, and may manifest as a wide range of gastrointestinal or extra-intestinal symptoms. However, there are likely to be many in the community who incorrectly attribute adverse physiological symptoms to wheat ingestion, and unnecessarily subject themselves to a gluten-free diet. Some concerns regarding the effect of a gluten-free diet suggest that it may not be as benign a treatment as once thought. Problems with the only current method of diagnosis for NCG/WS, the double-blind crossover trial, as well as inadequate exclusion of coeliac disease in some studies, cloud the interpretation of the literature. Further work is needed to define the place of NCG/WS in the context of other wheat-sensitive and functional gastrointestinal diseases, and to identify the patients most likely to benefit from a gluten-free diet. Following recommended guidelines for the diagnosis of coeliac disease will help confirm this diagnosis by enabling a clear differentiation between coeliac disease and NCG/WS.47 As a diagnostic method, the dietary trial is unlikely to be practicable in a clinical setting, and further insights into the pathogenesis of the disease, including the role of the microbiome, may lead to the uncovering of a biomarker that will facilitate diagnosis and negate the need for the problematic dietary crossover trial.
Box 1 – Double-blind, randomised, placebo-controlled, dietary gluten challenge for diagnosis of non-coeliac gluten sensitivity (NCGS)
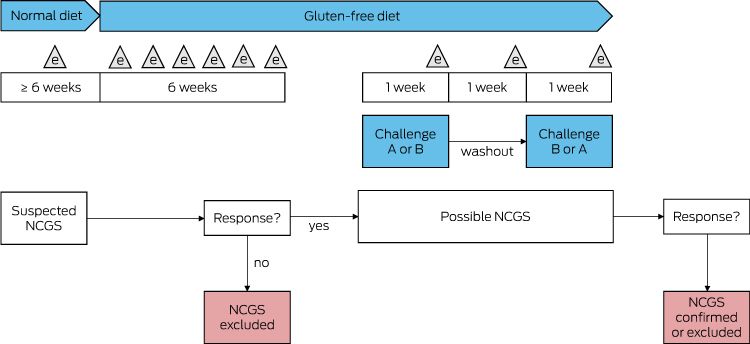
Adapted from Catassi et al.21 A, B = gluten or placebo. e = evaluation (weekly during the first part of the study, daily during the gluten and placebo challenge).
Box 2 – Salerno experts’ criteria for diagnosis of non-coeliac gluten sensitivity21
|
|
|||||||||||||||
|
All the following conditions need to be met to fulfil the criteria for diagnosis:
|
|||||||||||||||
|
|
|||||||||||||||
|
*Includes abdominal pain, heartburn, acid regurgitation, bloating, nausea and vomiting, borborygmus, abdominal distension, eructation, increased flatus, increased or decreased passage of stools, loose or hard stools, urgent need for defecation, feeling of incomplete evacuation, extra-intestinal symptoms, dermatitis, headache, foggy mind, numbness of the limbs, joint/muscle pains, fainting and oral/tongue lesions. † At least 8 g gluten/day, ideally free of fermentable oligo-, di-, and monosaccharides and polyols and indistinguishable from the gluten-free placebo. |
|||||||||||||||
Box 3 – Duodenal biopsies and non-coeliac gluten/wheat sensitivity
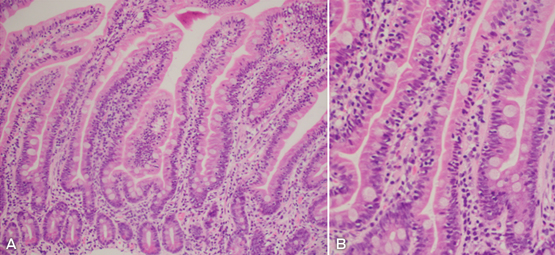
A (original magnification, × 10; haematoxylin–eosin stain) and B (original magnification, × 20; haematoxylin–eosin stain): Lymphocytic duodenosis (up to 65 intra-epithelial lymphocytes/100 enterocytes) and increased eosinophils in the lamina propria in a duodenal biopsy from a patient with non-coeliac gluten/wheat sensitivity. Intraepithelial duodenosis (≥ 25 lymphocytes per 100 enterocytes) is seen in both coeliac disease and non-coeliac gluten sensitivity, but not in functional dyspepsia.41,42 Duodenal mucosal eosinophilia is seen in both non-coeliac gluten sensitivity and functional dyspepsia.27,36
Box 4 – Potential mechanisms for the pathogenesis of non-coeliac gluten or wheat sensitivity
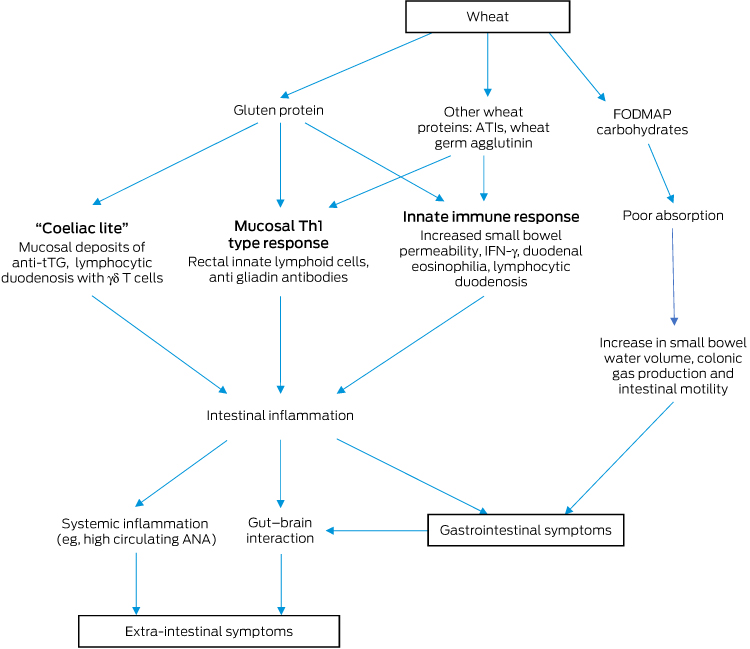
ANA = antinuclear antibody. ATI = amylase trypsin inhibitor. FODMAP = fermentable oligo-, di-, and monosaccharides and polyols. IFN = interferon. tTG = tissue transglutaminase. Ingestion of wheat exposes the intestinal mucosa to wheat proteins (gluten, ATIs, wheat germ agglutinin and other proteins) and carbohydrates (including FODMAPs). This leads to small bowel inflammation through innate and adaptive immune responses and subsequent gastrointestinal symptoms. Poor absorption of FODMAPs leads to increases in small bowel water content, colonic gas production and intestinal motility, again generating gastrointestinal symptoms.17 Subsequent systemic inflammation and possible interaction between the gastrointestinal and central nervous systems leads to generation of extra-intestinal symptoms.
Provenance: Commissioned; externally peer reviewed.
- Michael DE Potter1
- Marjorie M Walker1
- Nicholas J Talley1,2
- 1 University of Newcastle, Newcastle, NSW
- 2 Medical Journal of Australia, Sydney, NSW
Nicholas Talley is Editor-in-Chief of the Medical Journal of Australia.
- 1. Schuppan D, Dennis MD, Kelly CP. Celiac disease: epidemiology, pathogenesis, diagnosis, and nutritional management. Nutr Clin Care 2005; 8: 54-69.
- 2. Biesiekierski JR. What is gluten? J Gastroenterol Hepatol 2017; 32 Suppl 1: 78-81.
- 3. Shewry PR, Halford NG, Belton PS, Tatham AS. The structure and properties of gluten: an elastic protein from wheat grain. Philos Trans R Soc Lond B Biol Sci 2002; 357: 133-142.
- 4. Fasano A, Catassi C. Clinical practice. Celiac disease. N Engl J Med 2012; 367: 2419-2426.
- 5. Walker MM, Ludvigsson JF, Sanders DS. Coeliac disease: review of diagnosis and management. Med J Aust 2017; 207: 173-178.
- 6. Anderson RP, Henry MJ, Taylor R, et al. A novel serogenetic approach determines the community prevalence of celiac disease and informs improved diagnostic pathways. BMC Med 2013; 11: 188.
- 7. Cabrera-Chavez F, Dezar GV, Islas-Zamorano AP, et al. Prevalence of self-reported gluten sensitivity and adherence to a gluten-free diet in Argentinian adult population. Nutrients 2017; 9: 81.
- 8. Spence D. Bad medicine: food intolerance. BMJ 2013; 346: f529.
- 9. Golley S, Corsini N, Topping D, et al. Motivations for avoiding wheat consumption in Australia: results from a population survey. Public Health Nutr 2015; 18: 490-499.
- 10. DiGiacomo DV, Tennyson CA, Green PH, Demmer RT. Prevalence of gluten-free diet adherence among individuals without celiac disease in the USA: results from the Continuous National Health and Nutrition Examination Survey 2009–2010. Scand J Gastroenterol 2013; 48: 921-925.
- 11. Aziz I, Lewis NR, Hadjivassiliou M, et al. A UK study assessing the population prevalence of self-reported gluten sensitivity and referral characteristics to secondary care. Eur J Gastroenterol Hepatol 2014; 26: 33-39.
- 12. van Gils T, Nijeboer P, IJssennagger CE, et al. Prevalence and characterization of self-reported gluten sensitivity in The Netherlands. Nutrients 2016; 8: E714.
- 13. Cabrera-Chavez F, Granda-Restrepo DM, Aramburo-Galvez JG, et al. Self-reported prevalence of gluten-related disorders and adherence to gluten-free diet in Colombian adult population. Gastroenterol Res Pract 2016; 2016: 4704309.
- 14. Ontiveros N, López-Gallardo J, Vergara-Jiménez M, Cabrera-Chávez F. Self-reported prevalence of symptomatic adverse reactions to gluten and adherence to gluten-free diet in an adult Mexican population. Nutrients 2015; 7: 6000-6015.
- 15. Volta U, Caio G, Karunaratne TB, et al. Non-coeliac gluten/wheat sensitivity: advances in knowledge and relevant questions. Expert Rev Gastroenterol Hepatol 2017; 11: 9-18.
- 16. Nanayakkara WS, Skidmore PM, O’Brien L, et al. Efficacy of the low FODMAP diet for treating irritable bowel syndrome: the evidence to date. Clin Exp Gastroenterol 2016; 9: 131-142.
- 17. Staudacher HM, Irving PM, Lomer MC, Whelan K. Mechanisms and efficacy of dietary FODMAP restriction in IBS. Nat Rev Gastroenterol Hepatol 2014; 11: 256-266.
- 18. Biesiekierski JR, Peters SL, Newnham ED, et alNo effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 2013; 145: 320-328.e1-e3.
- 19. Junker Y, Zeissig S, Kim SJ, et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J Exp Med 2012; 209: 2395-2408.
- 20. Dalla Pellegrina C, Perbellini O, Scupoli MT, et al. Effects of wheat germ agglutinin on human gastrointestinal epithelium: insights from an experimental model of immune/epithelial cell interaction. Toxicol Appl Pharmacol 2009; 237: 146-153.
- 21. Catassi C, Elli L, Bonaz B, et al. Diagnosis of non-celiac gluten sensitivity (NCGS): the Salerno experts’ criteria. Nutrients 2015; 7: 4966-4977.
- 22. Molina-Infante J, Carroccio A. Suspected nonceliac gluten sensitivity confirmed in few patients after gluten challenge in double-blind, placebo-controlled trials. Clin Gastroenterol Hepatol 2017; 15: 339-348.
- 23. Gibson PR, Skodje GI, Lundin KE. Non-coeliac gluten sensitivity. J Gastroenterol Hepatol 2017; 32 Suppl 1: 86-89.
- 24. Husby S, Murray JA. Gluten sensitivity: celiac lite versus celiac like. J Pediatr 2014; 164: 436-438.
- 25. Volta U, Bardella MT, Calabro A, et al. Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med 2014; 12: 85.
- 26. Elli L, Tomba C, Branchi F, et al. Evidence for the presence of non-celiac gluten sensitivity in patients with functional gastrointestinal symptoms: results from a multicenter randomized double-blind placebo-controlled gluten challenge. Nutrients 2016; 8: 84.
- 27. Carroccio A, Mansueto P, Iacono G, et al. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity. Am J Gastroenterol 2012; 107: 1898-1906; quiz 907.
- 28. Carroccio A, Soresi M, D’Alcamo A, et al. Risk of low bone mineral density and low body mass index in patients with non-celiac wheat-sensitivity: a prospective observation study. BMC Med 2014; 12: 230.
- 29. Carroccio A, D’Alcamo A, Cavataio F, et al. High proportions of people with nonceliac wheat sensitivity have autoimmune disease or antinuclear antibodies. Gastroenterology 2015; 149: 596-603.e1.
- 30. Ford AC, Talley NJ, Walker MM, Jones MP. Increased prevalence of autoimmune diseases in functional gastrointestinal disorders: case-control study of 23471 primary care patients. Aliment Pharmacol Ther 2014; 40: 827-834.
- 31. Hollon J, Puppa EL, Greenwald B, et al.Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients 2015; 7: 1565-1576.
- 32. Uhde M, Ajamian M, Caio G, et al. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut 2016; 65: 1930-1937.
- 33. Sapone A, Lammers KM, Casolaro V, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med 2011; 9: 23.
- 34. Brottveit M, Beitnes AC, Tollefsen S, et al. Mucosal cytokine response after short-term gluten challenge in celiac disease and non-celiac gluten sensitivity. Am J Gastroenterol 2013; 108: 842-850.
- 35. Nylund L, Kaukinen K, Lindfors K. The microbiota as a component of the celiac disease and non-celiac gluten sensitivity. Clinical Nutrition Experimental 2016; 6: 17-24.
- 36. Talley NJ, Walker MM, Aro P, et al. Non-ulcer dyspepsia and duodenal eosinophilia: an adult endoscopic population-based case-control study. Clin Gastroenterol Hepatol 2007; 5: 1175-1183.
- 37. Di Liberto D, Mansueto P, D’Alcamo A, et al. Predominance of type 1 innate lymphoid cells in the rectal mucosa of patients with non-celiac wheat sensitivity: reversal after a wheat-free diet. Clin Transl Gastroenterol 2016; 7: e178.
- 38. Biesiekierski JR, Newnham ED, Irving PM, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol 2011; 106: 508-514; quiz 15.
- 39. Volta U, Tovoli F, Cicola R, et al. Serological tests in gluten sensitivity (nonceliac gluten intolerance). J Clin Gastroenterol 2012; 46: 680-685.
- 40. Troncone R, Ferguson A. Anti-gliadin antibodies. J Pediatr Gastroenterol Nutr 1991; 12: 150-158.
- 41. Molina-Infante J, Santolaria S, Sanders DS, Fernandez-Banares F. Systematic review: noncoeliac gluten sensitivity. Aliment Pharmacol Ther 2015; 41: 807-820.
- 42. Talley NJ, Walker MM. Celiac disease and nonceliac gluten or wheat sensitivity: The risks and benefits of diagnosis. JAMA Intern Med 2017; 177: 615-616.
- 43. Walker MM, Murray JA, Ronkainen J, et al. Detection of celiac disease and lymphocytic enteropathy by parallel serology and histopathology in a population-based study. Gastroenterology 2010; 139: 112-119.
- 44. Brown I, Mino-Kenudson M, Deshpande V, Lauwers GY. Intraepithelial lymphocytosis in architecturally preserved proximal small intestinal mucosa: an increasing diagnostic problem with a wide differential diagnosis. Arch Pathol Lab Med 2006; 130: 1020-1025.
- 45. Leffler D, Schuppan D, Pallav K, et al. Kinetics of the histological, serological and symptomatic responses to gluten challenge in adults with coeliac disease. Gut 2013; 62: 996-1004.
- 46. Rubio-Tapia A, Hill ID, Kelly CP, et al. American College of Gastroenterology. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 2013; 108: 656-676; quiz 77.
- 47. Ludvigsson JF, Bai JC, Biagi F, et al. Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut 2014; 63: 1210-1228.
- 48. Rosinach M, Fernandez-Banares F, Carrasco A, et al. Double-blind randomized clinical trial: gluten versus placebo rechallenge in patients with lymphocytic enteritis and suspected celiac Ddisease. PLoS One 2016; 11: e0157879.
- 49. Husby S, Koletzko S, Korponay-Szabo IR, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr 2012; 54: 136-160.
- 50. Ludvigsson JF, Leffler DA, Bai JC, et al. The Oslo definitions for coeliac disease and related terms. Gut 2013; 62: 43-52.
- 51. Lambert K, Ficken C. Cost and affordability of a nutritionally balanced gluten-free diet: Is following a gluten-free diet affordable? Nutr Diet 2016; 73: 36-42.
- 52. Hallert C, Grant C, Grehn S, et al. Evidence of poor vitamin status in coeliac patients on a gluten-free diet for 10 years. Aliment Pharmacol Ther 2002; 16: 1333-1339.
- 53. Theethira TG, Dennis M, Leffler DA. Nutritional consequences of celiac disease and the gluten-free diet. Expert Rev Gastroenterol Hepatol 2014; 8: 123-129.
- 54. Vici G, Belli L, Biondi M, Polzonetti V. Gluten free diet and nutrient deficiencies: a review. Clin Nutr 2016; 35: 1236-1241.
- 55. Missbach B, Schwingshackl L, Billmann A, et al. Gluten-free food database: the nutritional quality and cost of packaged gluten-free foods. PeerJ 2015; 3: e1337.
- 56. Miranda J, Lasa A, Bustamante MA, et al. Nutritional differences between a gluten-free diet and a diet containing equivalent products with gluten. Plant Foods Hum Nutr 2014; 69: 182-187.
- 57. Zanini B, Mazzoncini E, Lanzarotto F, et al. Impact of gluten-free diet on cardiovascular risk factors. A retrospective analysis in a large cohort of coeliac patients. Dig Liver Dis 2013; 45: 810-815.
- 58. Tortora R, Capone P, De Stefano G, et al. Metabolic syndrome in patients with coeliac disease on a gluten-free diet. Aliment Pharmacol Ther 2015; 41: 352-359.
- 59. Berti C, Riso P, Monti LD, Porrini M. In vitro starch digestibility and in vivo glucose response of gluten-free foods and their gluten counterparts. Eur J Nutr 2004; 43: 198-204.
- 60. Capristo E, Malandrino N, Farnetti S, et al. Increased serum high-density lipoprotein-cholesterol concentration in celiac disease after gluten-free diet treatment correlates with body fat stores. J Clin Gastroenterol 2009; 43: 946-949.
- 61. Bulka CM, Davis MA, Karagas MR, et al. The unintended consequences of a gluten-free diet. Epidemiology 2017; 28: e24-e25.
- 62. Munera-Picazo S, Ramirez-Gandolfo A, Burlo F, Carbonell-Barrachina AA. Inorganic and total arsenic contents in rice-based foods for children with celiac disease. J Food Sci 2014; 79: T122-T128.
- 63. Bonder MJ, Tigchelaar EF, Cai X, et al. The influence of a short-term gluten-free diet on the human gut microbiome. Genome Med 2016; 8: 45.
- 64. Sanz Y. Effects of a gluten-free diet on gut microbiota and immune function in healthy adult humans. Gut Microbes 2010; 1: 135-137.





Summary