Abstract
Objectives: To investigate whether patients with English as their second language have similar acute coronary syndrome (ACS) outcomes to people whose first language is English.
Design: Retrospective, observational study, using admissions, treatment and follow-up data.
Participants and setting: : A total of 6304 subjects from 41 sites enrolled in the investigator-initiated CONCORDANCE ACS registry.
Main outcome measures: Baseline characteristics, treatments, and in-hospital and 6-month mortality.
Results: English as a second language (ESL) was reported by 1005 subjects (15.9%). Patients with English as their first language (EFL) were older, and were less likely to have diabetes mellitus or to smoke than the ESL patients. Prior myocardial infarction, heart failure and chronic renal failure were more common in the ESL group. In-hospital mortality was also higher in these patients (7.1% v 3.8% for EFL patients; P < 0.001). Predictors of in-hospital mortality included presentation in cardiogenic shock, cardiac arrest in hospital, a history of renal failure, prior cardiac failure, and ESL. Rates of cardiac catheterisation, percutaneous coronary intervention rates, and referral to cardiac rehabilitation were lower in the ESL group; at 6 months, all-cause mortality was also higher (13.8% v 8.3% for EFL group; P < 0.001). Logistic regression identified language, age, in-hospital renal failure, and recurrent ischaemia as predictors of 6-month mortality.
Conclusion: Patients presenting with an ACS who report English as their second language have poorer outcomes than patients who use English as their first language. This difference may not be entirely explained by baseline demographic disparities or management differences.
Australia is one of the most culturally and linguistically diverse nations in the world, its population of 24 million including an estimated 6 million people who were born overseas.1 Australian research has shown a higher prevalence of cardiovascular risk factors among southern European, Middle Eastern and Indian immigrants.2,3 The lack of a mutually comprehensible and usable written and spoken language is a major barrier to effective communication between health care providers and patients. This potentially affects the provision of primary and secondary disease preventive care, which, in turn, may affect patient outcomes. Immigrants from non-English-speaking backgrounds have a higher incidence of admissions for acute myocardial infarction, and remain in hospital longer than their English-speaking peers.4 Communication and language barriers have also been shown to affect the provision of quality care for South Asian immigrants.5
The Cooperative National Registry of Acute Coronary Care, Guideline Adherence and Clinical Events (CONCORDANCE) is an Australian observational registry that describes the management and outcomes of patients presenting to hospitals with acute coronary syndromes (ACS) from geographically diverse regions of Australia.6 Information about patients’ demographic characteristics, including whether the patient reported English as their second language, their presenting characteristics, past medical history, in-hospital management, and outcomes at 6 months and 2 years are collected. In our study, we examined the effect of having English as the second spoken language on the treatment and outcomes for patients presenting with an ACS.
Methods
The CONCORDANCE registry currently includes data from 41 hospitals representative of regional and acute care facilities, with a range of clinical and treatment characteristics and procedural capabilities. Enrolment processes and inclusion and exclusion criteria for the registry have been described previously.6 In brief, every month each site enrols the first ten patients who present to hospital with symptoms of an ACS together with significant electrocardiographic changes, elevated cardiac enzyme levels, or newly documented coronary heart disease.
Data collection and measures
The data collected included details about pre-hospital assessment and management, and the admission diagnosis; demographic characteristics; medical history; in-hospital investigations and management, including the timing of invasive therapy; medication dosage and timing; and in-hospital events. Clinical events are defined in the Appendix. Patients were followed up to assess quality of life measures, clinical events, and medication compliance 6 months and 2 years after discharge.
Definition of English as a second language
Demographic information collected included data pertaining to Indigenous status, country of birth, and language (English as first language [EFL] v English as second language [ESL] v unknown/undocumented). Ethnic background was classified as documented in the medical record, according to participant self-report or determined when discussing the study with the participant. The focus of our study was an analysis of demographic differences, use of evidence-based therapies, and cardiovascular outcomes, according to whether the subject reported using English as their first or second language.
Statistical analysis
Patients were dichotomised according to their English language status (ESL v EFL). Data for continuous variables were summarised as means and standard deviations (SDs), and for dichotomous variables as numbers of people and percentages.
Data were analysed in SAS 9.3 (SAS Institute). Baseline data were compared in univariate analyses (χ2 tests, t tests and Wilcoxon rank sum tests). Stepwise logistic regression was used to model the predictors associated with mortality. To account for the clustering effect of hospital as a factor, generalised estimating equation correction with an exchangeable working correlation matrix was applied. Similarly, a robust variance estimator was applied to the Cox regression analysis used to model overall mortality (from admission to 6-month follow-up). The proportional hazards assumption was visually checked by plotting the estimated survivor functions, and the ratio of hazards was found to be constant across time. Estimates of adjusted survival curves from the proportional hazard model were generated using the mean of covariates method.
The following factors were included in the Cox regression model: age, sex, diagnosis, Global Registry of Acute Coronary Events (GRACE) risk score, prior percutaneous coronary intervention (PCI), prior coronary bypass grafting (CABG), in-hospital PCI, in-hospital CABG, diabetes, prior myocardial infarction, congestive heart failure, renal failure, and prior stroke.
Candidate variables for the stepwise logistic regression models included those statistically significant at α = 0.1 in univariate comparisons. GRACE risk score was included in the model regardless of the statistical significance in the univariate comparison. Generalised linear modelling was performed using a forward selection process with entry and exclusion criteria set at α = 0.1.
Missing data
For 106 patients there was no registry information about language; these patients were excluded from the models that included language as a variable. In addition, about 2% of responses for other variables were missing; patients with missing data have been omitted from analyses where these variables were included in the model.
Ethics approval
The study protocol conforms with the ethics guidelines of the 1975 Declaration of Helsinki as reflected by a priori approval in the guidelines of the institutions’ human research ethics committees. Concord Hospital was the lead site for the New South Wales sites (approval reference, HREC 08/CRGH/180). Two authors (BD and DB) had full access to the data and assume full responsibility for the integrity of the data and the accuracy of the analysis. The lead author (CJ) affirms that this article is an accurate and transparent account of the study.
Results
Enrolment in the CONCORDANCE registry commenced in February 2009. In this article we present data on the first 6304 patients enrolled at 41 sites, of whom 27.7% presented with ST elevation myocardial infarction (STEMI), 47.3% with non-STEMI (NSTEMI), and 25% with unstable angina. The data used in this analysis include patients registered to June 2014.
Nearly three-quarters of the patients (4578, or 73%) were from Australia or New Zealand; 287 were from Asia (Chinese, 37; Southern Asian, 117; other Asian, 133), 498 from the United Kingdom or North America, 578 from Europe, 45 from Africa, and 318 were categorised as “other”. A total of 418 patients (6.6%) identified themselves as Aboriginal or Torres Strait Islander.
One thousand and five patients (15.9%) reported English as their second language. These patients were younger than those in the EFL group, and the prevalence of cardiovascular risk factors was higher (Box 1). The incidence of comorbidities was also higher in the ESL group, but there were no significant differences between the ESL and EFL groups in median GRACE risk score. ESL patients were more likely to be admitted to a metropolitan than to a rural hospital (70.4% v 61.1%; P < 0.001), but there were no differences in median symptom onset to admission time (2.4 h v 2.6 h; P = 0.44), median door-to-needle time (47 min v 42 min; P = 0.59), or median door-to-balloon time (118 min v 113 min; P = 0.40).
Rates of coronary angiography and PCI were lower in the ESL group, while rates of CABG were similar. ESL patients were also less likely to be referred for outpatient cardiac rehabilitation (Box 2).
The median length of hospital stay was greater for ESL patients (5 days v 4 days; P < 0.001). Antiplatelet agents such as ticagrelor and prasugrel were used less by ESL patients, but the use of other evidence-based therapies was similar in both groups (Box 3).
There was a higher incidence of heart failure, renal failure, stroke, recurrent myocardial infarction, major bleeding, and in-hospital mortality in the ESL group (Box 4). Independent predictors of in-hospital mortality included presentation in cardiogenic shock, cardiac arrest in hospital, in-hospital renal or cardiac failure, and having English as a second language (Box 5). At the 6-month follow-up, all-cause mortality was also higher in the ESL group (13.8% v 8.3%; P = 0.0001) (Box 6). ESL, age, in-hospital renal failure, and recurrent ischaemia were independent predictors of 6-month mortality (Box 7). The Cox regression model of survival at 6 months is outlined in Box 8.
Discussion
We found that mortality among patients presenting with an ACS who report English as their second language was higher than among those who report English as their first language. Other studies of Australian populations have not reported such a difference,7,8 but analyses of administrative data have compared populations according to standardised mortality rates, and did not specifically assess language as a marker of risk.
The incidence of diabetes mellitus, hypertension, dyslipidaemia and smoking was higher in our ESL group than among than those who used English as their first language. A systematic review2 found a higher incidence of smoking among male immigrants from the Middle East, the UK and Ireland, western and southern Europe, China, and Vietnam than among Australians of the same age. Another UK study suggested that people of South Asian origin had a higher incidence of diabetes mellitus, hypertension, dyslipidaemia and obesity than comparable Europeans,9 although the authors concluded that the measured metabolic risk factors did not entirely explain the overall differences in the incidence of coronary heart disease. Similarly, a study of Asian Indians living in Australia found a higher incidence of hypertension, diabetes mellitus and obesity than the national average.3 The proportion of patients from South Asia in our study was less than 2%, too small for us to identify this particular group as being at increased risk.
Several American studies have found longer delays to treatment for myocardial infarction for Hispanics than for non-Hispanic whites.10-12 The median door-to-needle and door-to-balloon times were slightly longer for our ESL patients, but the differences were not statistically significant.
Although patients with ESL were more likely to be admitted to a metropolitan rather than a rural hospital, we identified a reduced rate of cardiac catheterisation in ESL patients presenting with an ACS and a much lower rate of PCI than for those with English as their first language. Similar findings have been reported for Hispanic migrants in the United States13 and migrants of South Asian background in the UK.14 This is thought to reflect not a physician bias in recommending patients for revascularisation,14 but rather patient treatment preferences15 and perhaps their lack of language skills.16,17 We did not collect data on why revascularisation was not performed, but ESL patients may have had more diffuse disease, not amenable to revascularisation. Lack of English comprehension can affect access to health education that promotes health maintenance (primary prevention), which may mean patients present later, at a more advanced stage of disease.18
An Australian study4 that examined hospital discharge data for the period between 1993–94 and 1997–98 compared outcomes using an English-speaking background (ESB) v non-English-speaking background (NESB) dichotomy, based on the patient’s country of birth rather than their actual capacity to speak English. It was found that NESB patients were more likely to be admitted for acute myocardial infarction than ESB patients, possibly because of a delay in diagnosis. This study found a longer average length of hospital stay for NESB than for ESB patients, which the authors attributed to complications associated with later presentation. We also found a slightly longer length of stay in our ESL group; this may reflect differences in hospital events, but may also reflect delays in organising professional interpreters for obtaining an accurate history and facilitating informed consent for procedures.
Deficiencies in intercultural communication may play a role in the adverse outcomes for patients from culturally and linguistically diverse backgrounds.19,20 A review of the literature on cultural differences in communication suggested that doctors behave less effectively when interacting with patients from ethnic minorities, and patients themselves are also less verbally expressive and seem to be less assertive and effective during medical encounters.4
Fewer patients in our ESL group were referred for cardiac rehabilitation after discharge than patients with English as their first language. Two systematic reviews of secondary prevention programs of randomised controlled trials have shown that either supervised exercise alone21,22 or risk factor education or counselling without an exercise component22 reduced mortality. It is therefore possible that reduced attendance at cardiac rehabilitation in the ESL group also contributed to poorer outcomes. Hospitals should extend the reach of cardiac rehabilitation services by offering multilingual opportunities for patients of different backgrounds.
Second-line antiplatelet agents, such as ticagrelor and prasugrel, were used less in our ESL group. This may be partially explained by fewer PCIs in this cohort and a higher incidence of major bleeding, but clinicians may also have been concerned that they could not accurately exclude contraindications of their use in ESL patients. Prasugrel23 and ticagrelor24 reduce major adverse ischaemic events in patients presenting with an ACS more effectively than clopidogrel, and the less frequent use of these agents in our ESL patients may have contributed to their poorer outcomes.
Limitations
The patients themselves identified whether English was their first or second language, and we have no data on their fluency or length of time in Australia, and this may affect patient care and understanding. Further, we did not collect data on the use of interpreters with our ESL patients. A professionally trained medical interpreter can provide a higher degree of accuracy and confidentiality than family members or bilingual staff members; using non-professional interpreters can be expedient, but has the disadvantage of loss of productivity and additional stress on the staff involved, together with the risk of inadequate or incomplete translation. It is therefore unknown whether the use of interpreter services was adequate, and whether improving their availability would enhance clinical outcomes.
While we attempted to adjust for baseline differences, there may have been unmeasured variables, such as socio-economic status and educational level, that may have confounded the impact of English proficiency on outcomes. Finally, we did not rigorously collect data on compliance with medications and physician follow-up, which may also have affected long term outcomes.25
Conclusion
In this large registry study of patients presenting with an ACS, in-hospital and 6-month mortality was greater for patients who reported English as their second language. While this may be explained by a higher prevalence of cardiovascular risk factors leading to more advanced disease, problems of culturally specific communication may also play important roles, and should be the subject of further research.
Box 1 – Baseline demographics of the 6304 patients at 41 sites enrolled in the CONCORDANCE database
English as second language |
English as first language |
Difference (95% CI) |
P |
||||||||||||
Number |
1005 |
5299 |
|||||||||||||
Age [SD], years |
63.3 [14.9] |
65.3 [13.5] |
–2.06 (–3.05 to –1.07) |
< 0.001 |
|||||||||||
Sex (men) |
691 (68.8%) |
3699 (69.8%) |
–1% (–4% to 2%) |
0.507 |
|||||||||||
Diabetes |
403 (40.1%) |
1351 (25.5%) |
15% (11% to 18%) |
< 0.001 |
|||||||||||
Hypertension |
669 (66.6%) |
3287 (62.0%) |
5% (1% to 8%) |
0.005 |
|||||||||||
Dyslipidaemia |
628 (62.5%) |
2970 (56.0%) |
6% (3% to 10%) |
< 0.001 |
|||||||||||
Current smoker |
310 (30.8%) |
1429 (27.0%) |
4% (1% to 7%) |
0.011 |
|||||||||||
Median GRACE risk score [IQR] |
124 [100.8–147.6] |
125 [104.0–147.6] |
–1.00 (–3.30 to 1.30) |
0.400 |
|||||||||||
Prior cerebrovascular accident |
73 (7.3%) |
430 (8.1%) |
–1% (–3% to 1%) |
0.396 |
|||||||||||
Prior myocardial infarction |
368 (36.6%) |
1609 (30.4%) |
6% (3% to 10%) |
< 0.001 |
|||||||||||
Prior heart failure |
134 (13.3%) |
488 (9.2%) |
4% (2% to 6%) |
< 0.001 |
|||||||||||
Prior coronary artery bypass grafting |
131 (13.0%) |
681 (12.9%) |
0% (–2% to 3%) |
0.840 |
|||||||||||
Prior percutaneous coronary intervention |
201 (20.0%) |
1125 (21.2%) |
–1% (–4% to 1%) |
0.380 |
|||||||||||
Chronic renal failure |
185 (18.4%) |
411 (7.8%) |
11% (8% to 13%) |
< 0.001 |
|||||||||||
GRACE = Global Registry of Acute Coronary Events. | |||||||||||||||
Box 2 – In-hospital interventions in 6304 patients at 41 sites enrolled in the CONCORDANCE database
English as second language |
English as first language |
Difference (95% CI) |
P |
||||||||||||
Number |
1005 |
5299 |
|||||||||||||
Cardiac catheter |
714 (71.0%) |
4003 (75.5%) |
–5% (–8% to –2%) |
0.002 |
|||||||||||
Percutaneous coronary intervention |
346 (34.4%) |
2240 (42.3%) |
–8% (–11% to –5%) |
< 0.001 |
|||||||||||
Coronary artery bypass grafting |
89 (8.9%) |
411 (7.8%) |
1% (–1% to 3%) |
0.234 |
|||||||||||
Rehabilitation referral |
495 (49.3%) |
3120 (58.9%) |
–9% (–13% to –6%) |
< 0.001 |
|||||||||||
Box 3 – Discharge medications for 6304 patients at 41 sites enrolled in the CONCORDANCE database
English as second language |
English as first language |
Difference (95% CI) |
P |
||||||||||||
Number |
1005 |
5299 |
|||||||||||||
Aspirin |
790 (85.9%) |
4276 (85.0%) |
1% (–2% to 3%) |
0.917 |
|||||||||||
Clopidogrel |
497 (54.0%) |
2596 (51.6%) |
2% (–1% to 6%) |
0.341 |
|||||||||||
Ticagrelor or prasugrel |
79 (8.6%) |
627 (12.5%) |
–4% (–6% to –2%) |
< 0.001 |
|||||||||||
β-Blockers |
719 (78.1%) |
3881 (77.1%) |
1% (–2% to 4%) |
0.733 |
|||||||||||
Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker |
704 (76.5%) |
3799 (75.5%) |
–1% (–4% to 2%) |
0.740 |
|||||||||||
Statin |
815 (88.6%) |
4508 (89.6%) |
–1% (–3% to 1%) |
0.548 |
|||||||||||
Box 4 – In-hospital events for 6304 patients at 41 sites enrolled in the CONCORDANCE database
English as second language |
English as first language |
Difference (95% CI) |
P |
||||||||||||
Number |
1005 |
5299 |
|||||||||||||
Left ventricular failure |
153 (15.2%) |
444 (8.4%) |
7% (5% to 9%) |
< 0.001 |
|||||||||||
Renal failure |
103 (10.2%) |
268 (5.1%) |
5% (3% to 7%) |
< 0.001 |
|||||||||||
Myocardial infarction |
41 (4.1%) |
144 (2.7%) |
1% (0 to 3%) |
0.021 |
|||||||||||
Stroke |
12 (1.2%) |
25 (0.5%) |
1% (0 to 1%) |
0.007 |
|||||||||||
Major bleed |
106 (10.5%) |
441 (8.3%) |
2% (0 to 4%) |
0.020 |
|||||||||||
Death |
71 (7.1%) |
200 (3.8%) |
3% (2% to 5%) |
< 0.001 |
|||||||||||
Box 5 – Logistic regression analysis of in-hospital mortality
Characteristic |
Odds ratio |
95% CI |
P |
||||||||||||
English as first language |
0.56 |
0.33–0.94 |
0.029 |
||||||||||||
Cardiac arrest in hospital |
16.95 |
10.53–27.78 |
< 0.001 |
||||||||||||
Cardiogenic shock |
7.04 |
4.46–11.11 |
< 0.001 |
||||||||||||
GRACE score |
1.04 |
1.03–1.05 |
< 0.001 |
||||||||||||
Renal failure |
5.08 |
3.29–7.81 |
< 0.001 |
||||||||||||
Congestive failure |
2.08 |
1.26–3.44 |
0.005 |
||||||||||||
GRACE = Global Registry of Acute Coronary Events. | |||||||||||||||
Box 6 – Kaplan–Meier estimates of survival at 6 months for 6304 patients at 41 sites enrolled in the CONCORDANCE database*
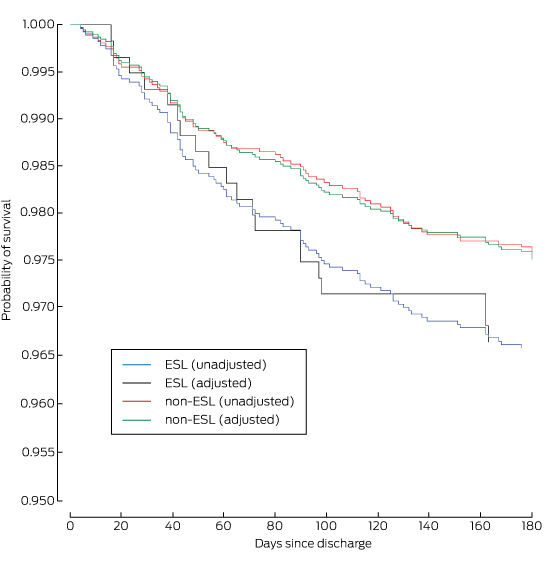
ESL = English spoken as second language. * Adjusted for age, diagnosis, sex, previous stroke, chronic renal failure, chronic heart failure, diabetes, prior myocardial infarction, prior coronary artery bypass grafting and prior percutaneous coronary intervention.
Box 7 – Logistic regression analysis of mortality to 6 months after discharge for 6304 patients at 41 sites enrolled in the CONCORDANCE database
Characteristic |
Odds ratio |
95% CI |
P |
||||||||||||
English as first language |
0.55 |
0.31–0.97 |
0.040 |
||||||||||||
Age |
1.09 |
1.07–1.11 |
< 0.001 |
||||||||||||
Renal failure |
4.67 |
2.88–7.58 |
< 0.001 |
||||||||||||
Ischaemia |
2.54 |
1.54–4.22 |
< 0.001 |
||||||||||||
Box 8 – Cox regression model of survival at 6 months for 6304 patients at 41 sites enrolled in the CONCORDANCE database
Characteristic |
Hazard ratio |
95% CI |
P |
||||||||||||
Age |
1.08 |
1.06–1.10 |
< 0.001 |
||||||||||||
Diagnosis |
3.96 |
3.22–4.70 |
< 0.001 |
||||||||||||
Sex |
0.86 |
0.42–1.30 |
0.502 |
||||||||||||
Prior stroke/transient ischaemic attack |
0.95 |
0.35–1.55 |
0.868 |
||||||||||||
Chronic renal failure |
0.43 |
0.05–0.90 |
< 0.001 |
||||||||||||
Congestive heart failure |
0.36 |
0.12–0.84 |
< 0.001 |
||||||||||||
Diabetes |
0.90 |
0.46–1.34 |
0.642 |
||||||||||||
Prior myocardial infarction |
0.84 |
0.36–1.33 |
0.489 |
||||||||||||
Prior coronary artery bypass grafting |
1.03 |
0.52–1.53 |
0.922 |
||||||||||||
Prior percutaneous coronary intervention |
1.08 |
0.57–1.59 |
0.764 |
||||||||||||
Percutaneous coronary intervention |
1.36 |
0.85–1.87 |
0.239 |
||||||||||||
Coronary artery bypass grafting |
8.00 |
6.01–9.98 |
0.040 |
||||||||||||
Received 16 July 2015, accepted 9 December 2015
- Craig P Juergens1,6
- Bilyana Dabin2
- John K French1,6
- Leonard Kritharides2
- Karice Hyun3
- Jens Kilian4
- Derek PB Chew5
- David Brieger2
- 1 Liverpool Hospital, Sydney, NSW
- 2 Concord Repatriation Hospital, Sydney, NSW
- 3 The George Institute for Global Health, Sydney, NSW
- 4 Bankstown Hospital, Sydney, NSW
- 5 Flinders Medical Centre, Adelaide, SA
- 6 South Western Sydney Clinical School, University of NSW, Sydney, NSW
We thank all the investigators and study coordinators who contributed to the CONCORDANCE Registry.
The CONCORDANCE registry has been funded by grants to the Sydney Local Health District from Sanofi Aventis, Astra Zeneca, Eli Lilly, Boehringer Ingelheim, the Merck Sharp and Dohme/Schering Plough joint venture, and the National Heart Foundation of Australia. The sponsors played no role in the design, analysis, or preparation of this article.
- 1. Australian Bureau of Statistics. Migration, 2009–2010 (Cat. No. 3412.0). Canberra: ABS, 2011. http://www.abs.gov.au/ausstats/subscriber.nsf/log?openagent&34120_2009-10.pdf&3412.0&Publication&CAC6E05106F66A13CA2578B000119F19&&2009-10&16.06.2011&Previous (accessed Jan 2016).
- 2. Dassanayake J, Dharmage SC, Gurrin L, et al. Are immigrants at risk of heart disease in Australia? A systematic review. Aust Health Rev 2009; 33: 479-491.
- 3. Fernandez R, Rolley JX, Rajaratnam R, et al. Risk factors for coronary heart disease among Asian Indians living in Australia. J Transcult Nurs 2015; 26: 57-63.
- 4. Renzaho A. Ischaemic heart disease and Australian immigrants: the influence of birthplace and language skills on treatment and use of health services. HIM J 2007; 36: 26-36.
- 5. Schouten BC, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient Educ Couns 2006; 64: 21-34.
- 6. Aliprandi-Costa B, Ranasinghe I, Turnbull F, et al. The design and rationale of the Australian cooperative national registry of acute coronary care, guideline adherence and clinical events (CONCORDANCE). Heart Lung Circ 2013; 22: 533-541.
- 7. Young CM. Migration and mortality: the experience of birthplace groups in Australia. Int Migr Rev 1987; 21: 531-554.
- 8. Singh M, de Looper M. Australian health inequalities: 1 Birthplace (AIHW Cat. No. AUS 27; Australian Institute of Health and Welfare Bulletin No. 2). Canberra: AIHW, 2002. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442453153 (accessed Jan 2016).
- 9. Tillin T, Hughes AD, Mayet J, et al. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians and African Caribbeans: SABRE (Southall and Brent Revisited) — a prospective population-based study. J Am Coll Cardiol 2013; 61: 1777-1786.
- 10. Henderson SO, Magana RN, Korn CS, et al. Delayed presentation for care during acute myocardial infarction in a Hispanic population of Los Angeles County. Ethn Dis 2002; 12: 38-44.
- 11. Bradley EH, Herrin J, Wang Y, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA 2004; 292: 1563-1572.
- 12. DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among US Hispanics. Am J Prev Med 2006; 30: 189-196.
- 13. Daumit GL, Hermann JA, Coresh J, Powe NR. Use of cardiovascular procedures among black persons and white persons: a 7-year nationwide study in patients with renal disease. Ann Intern Med 1999; 130: 173-182.
- 14. Feder G, Crook AM, Magee P, et al. Ethnic differences in invasive management of coronary disease: prospective cohort study of patients undergoing coronary angiography. BMJ 2002; 324: 511-516.
- 15. Whittle J, Conigliaro J, Good CB, Joswiak M. Do patient preferences contribute to racial differences in cardiovascular procedure use? J Gen Intern Med 1997; 12: 267-273.
- 16. Renzaho A. Addressing the needs of refugees and humanitarian entrants in Victoria: an evaluation of health and community services. Melbourne: Centre for Culture, Ethnicity and Health, 2002.
- 17. Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982–84. Am J Public Health 1990; 80 Suppl: 11-19.
- 18. Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured. Findings from a national sample. Med Care 2002; 40: 52-59.
- 19. Woloshin S, Bickell NA, Schwartz LM, et al. Language barriers in medicine in the United States. JAMA 1995; 273: 724-728.
- 20. Webster RA, Thompson DR, Mayou RA. The experiences and needs of Gujarati Hindu patients and partners in the first month after a myocardial infarction. Eur J Cardiovasc Nurs 2002; 1: 69-76.
- 21. Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 2004; 116: 682-692.
- 22. Clark AM, Hartling L, Vendermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med 2005; 143: 659-672.
- 23. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357: 2001-2015.
- 24. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009; 361: 1045-1057.
- 25. Sundquist J, Winkleby MA, Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: an analysis of NHANES III, 1988–94. J Am Geriatr Soc 2001; 49: 109-116.





dani fried
Competing Interests: No relevant disclosures
Ms dani fried
-
Craig Juergens
Competing Interests: No relevant disclosures
Assoc Prof Craig Juergens
Liverpool Hospital