We present the first case of severe injuries caused by an elephant in an Australian zoo. Although the patient sustained potentially life-threatening injuries, excellent prehospital care allowed her to make a full recovery without any long-term complications.
Clinical record
A 41-year-old female zookeeper was urgently transferred to the Royal North Shore Hospital Emergency Department (ED) by ambulance after a severe crush injury to the chest caused by a 2-year-old male elephant.
The 1200 kg male Asian elephant was born in captivity and was well known to the keeper. On the day of the incident, they were involved in a training session when the elephant challenged an instruction. The keeper recognised this change in his behaviour and tried to leave the training area, but the elephant used his trunk to pin her by the chest against a bollard in the barn, resulting in immediate dyspnoea and brief loss of consciousness for 20–30 seconds. Her colleagues arrived and moved her to safety.
When the ambulance arrived, the woman was alert and oriented, and complaining of dyspnoea and severe right-sided chest pain. Initial observations were pulse rate of 110 beats/min, systolic blood pressure (SBP) of 100 mmHg, and a respiratory rate of 36 breaths per minute. She rapidly developed increasing respiratory distress and was found to have absent breath sounds on the right side of her chest and reduced air entry on the left. She had subcutaneous emphysema involving the head, neck, torso and upper limbs. Intensive care paramedic backup was requested; when they arrived, she was unconscious with agonal respirations and no palpable pulse. High-flow oxygen was applied at 15 L/min through a mask and cardiopulmonary resuscitation was commenced. A provisional diagnosis of bilateral tension pneumothoraces (PTx) was made. The ambulance officers performed bilateral needle chest thoracostomies with 12G × 9 cm Dwellcath cannulas at the level of the second intercostal spaces in the mid-clavicular line. Although there was no immediate rush of air following either procedure, after about 10 minutes there was a return of cardiac output (pulse rate, 76 beats/min; SBP, 160 mmHg), return of spontaneous respiration (32/min) and improved conscious state (Glasgow coma scale, 10).
On arrival in the ED, she had a heart rate of 115 beats/min, SBP of 90 mmHg, respiratory rate of 38/min and SaO2 of 74% on 14 L oxygen. Physical examination was difficult because of extensive subcutaneous emphysema over the torso. There was significant bruising over the right breast and upper abdomen. No other injuries were identified. A Focused Assessment by Sonography for Trauma (FAST) examination of the abdomen was performed, but it was difficult to interpret because of the extensive subcutaneous emphysema over the chest and abdominal walls.
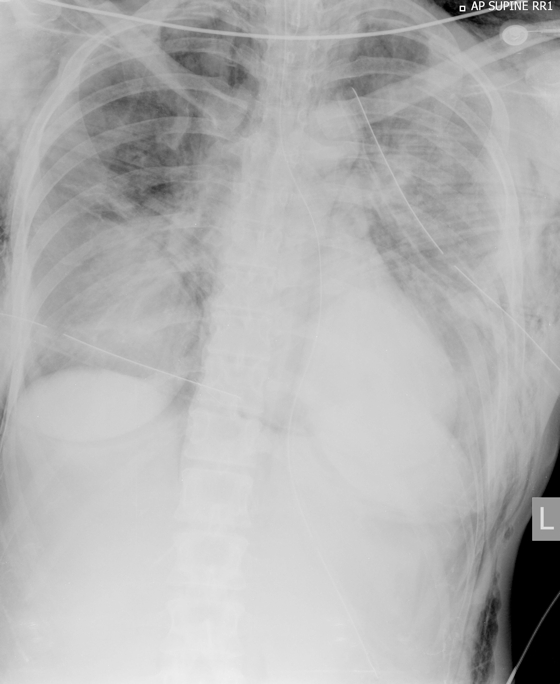
She was intubated and bilateral 32 Fr intercostal catheters were inserted, which improved ventilation and haemodynamic stability; the bilateral decompression needle catheters were removed. Chest x-rays (Box 1) showed extensive subcutaneous emphysema, multiple rib fractures and a persistent small right apical PTx.
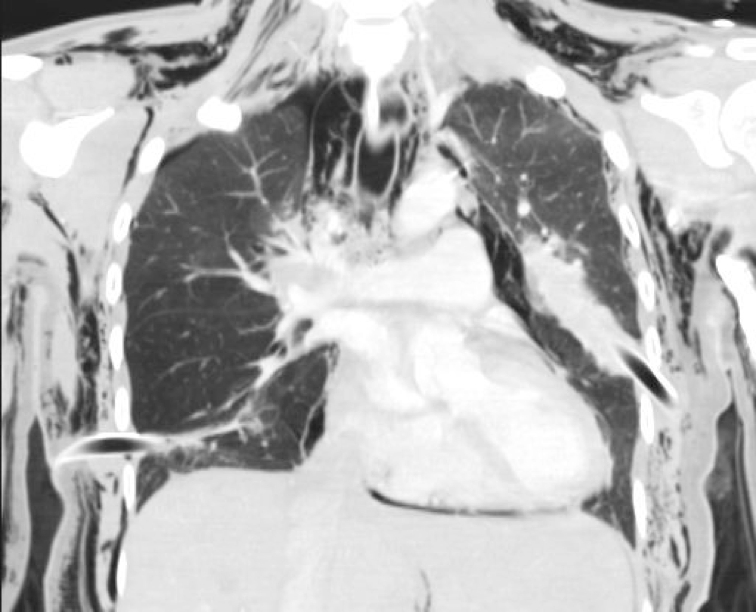
Computed tomography of the cervical spine, chest (Box 2) and abdomen showed injuries involving the spine, ribs, sternum, lungs and liver (Box 3).
The woman was admitted to the intensive care unit with ventilation support for 4 days. Subsequent recovery was uneventful and she was discharged home on Day 11 without further complications.
Discussion
In the past 15 years, there have been at least 18 fatal incidents involving elephants in zoos around the world.1,2 To date, no cases of injury or death caused by an elephant in Australia have been reported in the literature.
This case of elephant-related trauma shows the importance of clinical acumen and good prehospital management in the management of serious chest trauma. Tension PTx is a rare and potentially fatal medical emergency. It is a reversible cause of traumatic shock and cardiac arrest.3
Tension PTx can occur after significant blunt chest injury.4 Symptoms and signs include severe respiratory distress, decreased oxygen saturation, hyperexpansion and hyperresonance on percussion, and reduced air entry on auscultation.5 Tension PTx can cause acute cardiovascular collapse and shock because of decreased venous return that results from sudden positive intrapleural pressure.5 The diagnosis is usually made clinically (as in this case). A chest x-ray is not usually seen, but, if taken, will show marked midline shift, hyperexpansion of the affected side and lung collapse in a unilateral tension PTx. In bilateral tension PTx, there is bilateral hyperexpansion of the pleural cavities and bilateral lung collapse.
Trauma consensus guidelines recommend that tension PTx be diagnosed clinically, because urgent chest decompression is required.4
Unilateral or bilateral tension PTx caused by blunt injury may be associated with significant subcutaneous emphysema6 that makes auscultation of the chest difficult.
The immediate management of tension PTx requires urgent needle decompression in the second intercostal space mid-clavicular line, followed by definitive management with insertion of an intercostal catheter (tube thoracostomy), usually in the fourth or fifth intercostal space anterior to the mid-axillary line.
In Australia, needle decompression of the chest can be performed by appropriately skilled paramedics (level 4 and above). Indications for prehospital chest decompression after serious injury include traumatic cardiorespiratory arrest, significant (refractory) hypoxia or hypotension, multiple concomitant injuries, long transport time, need for positive pressure ventilation, and helicopter transport. Retrieval medical specialists may also perform tube thoracentesis or open thoracostomy in the prehospital environment.6
1 Initial chest x-ray showing bilateral rib fractures, extensive subcutaneous emphysema and bilateral intercostal catheters
2 Coronal computed tomography of the chest showing residual right-side pneumothorax, pneumomediastinum, extensive bilateral subcutaneous emphysema and bilateral intercostal catheters
3 Injuries sustained by the woman and identified by trauma computed tomography
Fractures
- Left C1 transverse process
- Sternum (undisplaced)
- Left ribs: 1, 2–5 (flail segment), 6–8
- Right ribs: 1–2
- Right sternochondral joint angulation: ribs 3–5
Other
- Left haemopneumothorax
- Right pneumothorax and pneumomediastinum
- Bilateral pulmonary contusions
- Extensive bilateral lower lobe collapse
- Periportal oedema of the liver
- Extensive subcutaneous emphysema
- 1. Accidents with elephants. Elephant Encyclopedia [website]. http://www.upali.ch/accident_en.html (accessed Nov 2014).
- 2. ‘Panic-attack’ elephant crushes zoo owner to death in trunk. Sydney Morning Herald, 2012; Apr 26. http://www.smh.com.au/environment/animals/panicattack-elephant-crushes-zoo-owner-to-death-in-trunk-20120426-1xmi1.html (accessed Nov 2014).
- 3. American College of Surgeons, Committee on Trauma. Advanced trauma life support (ATLS), 9th ed. Chicago: American College of Surgeons Committee on Trauma, 2012.
- 4. Leigh-Smith S, Harris T. Tension pneumothorax — time for a re-think? Emerg Med J 2005; 22: 8-16.
- 5. Lee C, Revell M, Porter K, Steyn R. The prehospital management of chest injuries: a consensus statement. Faculty of Pre-hospital Care, Royal College of Surgeons of Edinburgh. Emerg Med J 2007; 24: 220-224.
- 6. NSW Aeromedical and Medical Retrieval Services. Pre-hospital blunt thoracic trauma. 2010. https://nswhems.files.wordpress.com/2011/09/c-09-blunt-thoracic-trauma.pdf (accessed Mar 2015).





: No relevant disclosures.