A young woman was treated for musculoskeletal neck pain with acupuncture and developed a local paracervical abscess that progressed to a disseminated sepsis. The treatment was performed with an unusually long retention time of the acupuncture needle. This unique case shows that although acupuncture is deemed to be safe, serious complications may arise.
Clinical record
A 16-year-old, previously healthy girl was experiencing left-sided neck pain. She had no history of trauma or intravenous drug use, and there were no associated symptoms such as fevers, chills, cough or rigors. Initially, she attempted to manage her pain with simple pain medications. One week after onset, and experiencing ongoing pain, she presented to her general practitioner, who treated her with acupuncture. Two acupuncture needles (about 5 cm long) were placed locally to the left side of her neck. One remained for only 15 minutes; the other was fully inserted with only the handle visible and remained in situ for almost 24 hours.
Three days later, she developed significant worsening of her neck pain, lymphadenopathy, fevers, sweats and rigors. The next day, she was admitted at a small rural hospital with left neck pain and stiffness, associated with left-sided back and chest wall pain. She was started on 1 g of flucloxacillin every 6 hours.
Her pulse rate was 107 beats/min, oxygen saturation was 98% on room air, body temperature was 37.1°C and blood pressure was 121/68 mmHg. On physical examination, there was a diffuse swelling in the posterior triangle of her neck. An ejection systolic flow murmur was audible on auscultation. Oral candidiasis and pharyngitis with small punctate lesions were present. There was decreased air entry in her left lung base.
Investigations at the time of presentation showed a white blood cell count of 24.7 × 109/L (reference interval [RI], 4–11 × 109/L), C-reactive protein level of 404 mg/L (RI, < 10 mg/L) and albumin level of 17 mg/L (RI, 30–50 mg/L). Test results for HIV, hepatitis B and hepatitis C were negative. Blood cultures grew methicillin-sensitive Staphylococcus aureus. A chest x-ray showed a left pleural effusion. An ultrasound scan showed numerous enlarged lymph nodes in her neck that were reactive in appearance, as well as a left chest wall haematoma. A computed tomography (CT) scan of her neck also identified multiple small-volume reactive lymph nodes on both sides of the neck and diffuse subcutaneous oedema extending from the left preauricular region to the root of the neck. No focal fluid collection or abscess was identified. A CT scan of her chest and abdomen showed bilateral pleural effusions (left more than right), bilateral consolidation, splenomegaly, and a chest wall haematoma on the left.
A change of management involved increasing the flucloxacillin dose to 2 g every 4 hours (changed to 6-hourly on Day 10) and further investigations. On Day 1 after admission, a transthoracic echocardiogram showed no evidence of infective endocarditis. Her C-reactive protein level improved to 247 mg/L on Day 3.
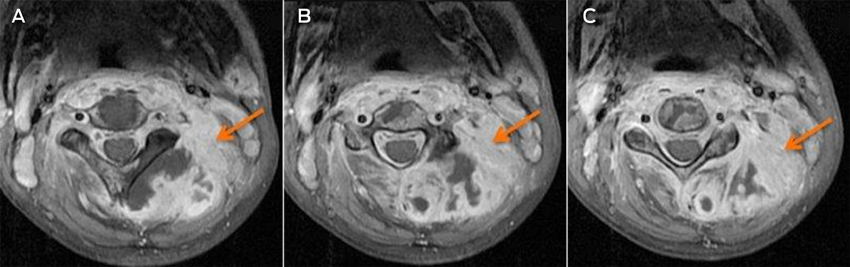
A magnetic resonance imaging scan on Day 7 identified an infiltrative lesion in the posterior paravertebral muscles, involving cervical vertebrae 1–5 and the spinal canal at that level (Box). The diagnostic possibilities were primary or secondary malignancy or infection. A pleural tap the next day drained 500 mL of blood-stained fluid. Laboratory results confirmed an empyema that grew S. aureus from the tap fluid.
Eleven days after her admission to the rural hospital, she was transferred to our tertiary teaching hospital. A CT-guided biopsy of the lesion identified S. aureus infection. No monoclonal B-cell or aberrant T-cell or natural killer cell populations were detected. There was no need for surgical management. The patient improved significantly with antibiotic therapy and was discharged from the tertiary hospital after 10 days and transferred back to the rural hospital.
Discussion
Acupuncture is a common treatment used for the management of pain. It is an invasive procedure whereby a needle is inserted to varying depths below the skin. In a review of 12 prospective studies looking at more than one million treatments, there were 715 adverse events including 12 deaths.1,2 Serious complications included pneumothoraxes,1 infections and neurovascular injuries.3 A review of the literature identified 65 case reports and series of infection occurring after acupuncture. When there is a breakage in the protective skin, barrier infection is an expected complication. There are certain factors that increase the risk of an infection after acupuncture. These include inadequate skin disinfection and poor hygiene,4 the use of needles that are too long (with subsequent penetration of the bowel and direct inoculation of the soft tissues), patients with immunodeficiency,5 and acupuncture into joints that have a metal prosthesis.6 We believe that the time that the needle is kept in situ is likely to be another important factor in increasing the likelihood of developing infection.
There is only limited evidence for the advantage of prolonged acupuncture needle retention time and almost no evidence or recommendation for needle retention time for longer than a few hours.
Although some acupuncturists consider needle retention time as an important variable in the management of patients,7,8 there are limited studies examining the best needle retention time.7,8 Further, there are no randomised clinical trials demonstrating the efficacy of a needle retention time of 24 hours or more. Some studies found that increased needle retention time caused a greater duration of breach of the skin barrier, which could increase the likelihood of infection.9,10 The current infection control guidelines for acupuncture of the Australian Acupuncture and Chinese Medicine Association11 do not discuss the needle retention time.
Our patient’s left neck pain was thought to be musculoskeletal in origin and was initially managed with acupuncture by a GP. Both acupuncture needles were placed in the left neck region and one remained in situ for almost 24 hours. Because of the temporal nature of the cervical collection and the pain occurring in the exact location that the acupuncture needle was placed, the needle was the presumed source of infection.
This case shows a serious complication in an otherwise healthy young woman after an acupuncture treatment with unusually long needle retention time, which most likely contributed to the development of the infection. It highlights that even fairly minor invasive procedures can lead to significant complications. This should be considered when recommending these procedures, and high hygiene standards should always be applied.
- Constantin E Dlaska
- Scott Temple
- Michael A Schuetz
- Princess Alexandra Hospital, Brisbane, QLD
No relevant disclosures.
- 1. White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med 2004; 22: 122-133.
- 2. Vincent C. The safety of acupuncture. BMJ 2001; 323: 467-468.
- 3. Bang MS, Lim SH. Paraplegia caused by spinal infection after acupuncture. Spinal Cord 2006; 44: 258-259.
- 4. Rosted P. Literature survey of reported adverse effects associated with acupuncture treatment. Am J Acupunct 1996; 24: 27-34.
- 5. Pierik MG. Fatal Staphylococcal septicemia following acupuncture: report of two cases. Occurrence of Staphylococcal septicemia following acupuncture emphasizes need for thorough medical evaluation before such procedures. R I Med J 1982; 65: 251-253.
- 6. Nakajima A, Kaneyama R, Watanabe H, et al. Acupuncture needle-associated prosthetic knee infection after total knee arthroplasty. Mod Rheumatol 2010; 20: 627-631.
- 7. Wang XL, Huang HY. [Observation on therapeutic effect of long-time needle retention at Baihui (GV 20) on vertebroarterial cervical spondylopathy] [Chinese]. Zhongguo Zhen Jiu 2007; 27: 415-416.
- 8. Yao XJ, Liu JW. [Observation on clinical efficacy of acute pain treated with the intervention of different time of needle retention] [Chinese]. Zhongguo Zhen Jiu 2013; 33: 985-988.
- 9. Botte MJ, Davis JL, Rose BA, et al. Complications of smooth pin fixation of fractures and dislocations in the hand and wrist. Clin Orthop Relat Res 1992; (276): 194-201.
- 10. Desai A, Dramis A, Thompson N, et al. Discharging pin sites following K-wire fixation of distal radial fractures: a case for pin removal? Acta Orthop Belg 2009; 75: 310-315.
- 11. Australian Acupuncture and Chinese Medicine Association. Infection Control Management Plan — template for Queensland Acupuncture Practices. Brisbane: AACMA, 2011. http://www.acupuncture.org.au/Publications/Infection_Control.aspx (accessed Sep 2015).





Bill Meyers
Constantin E Dlaska, Scott Temple and Michael A Schuetz
Med J Aust 2015; 203 (10): 408-409.
On behalf of the Australian Medical Acupuncture College I wish to state that the College does not train medical practitioners to embed 5cm needles in patients.
All Quality Improvement and Continuing Professional Development Activities in Medical Acupuncture include Patient Safety as a core component.
It is regrettable that a young patient has been harmed by a medical practitioner performing acupuncture. However, if we place this case in the context of comparative risk, serious Staphylococcus Aureus Bacteraemia occurs in 0.9 per 10,000 Australian inpatients (1,621 in 2013-2014) http://www.aihw.gov.au/publication-detail/?id=60129550044
Using the Dept of Health data re numbers of GP services: http://www.health.gov.au/internet/main/publishing.nsf/content/general+practice+statistics-1 and extrapolating from: JL Wardle, D Sibbrit, J Adams Acupuncture referrals in rural primary healthcare: a survey of general practitioners in rural and regional New South Wales, Australia Acupunct Med., 31 (2013), pp. 375–382, we find the rate of serious medical acupuncture infections in Australia to be less than 1 per 100,000.
Competing Interests: President Australian Medical Acupuncture College
Dr Bill Meyers
AMAC