Being mortal is about the struggle to cope with the constraints of our biology, with the limits set by genes and cells and flesh and bone. Medical science has given us remarkable power to push against these limits, and the potential value of this power was a central reason I became a doctor. But again and again, I have seen the damage we in medicine do when we fail to acknowledge that such power is finite and always will be.
We've been wrong about what our job is in medicine. We think our job is to ensure health and survival. But really it is larger than that. It is to enable well-being. And well-being is about the reasons one wishes to be alive.
Atul Gawande. Being mortal. London: Profile Books, 2014.
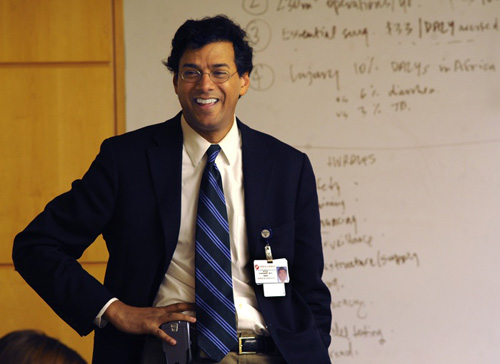
Atul Gawande, 49, is a general surgeon at the Brigham and Women's Hospital in Boston and holds academic positions in the Harvard Medical School and School of Public Health. He is also a writer. Being mortal uses both his clinical experiences and literary skills as they relate to the care we give, or should give, when our patients enter the twilight zone between responsiveness to medical and surgical interventions and when they move beyond the reach of our finest instruments and technical remedies.
The central question of the book is not new, nor are the answers. The question is this: given the inevitable decline in capacity as we age, especially when sick, how can medicine best assist us? The answer is that by determining what it is that patients perceive to be what gives their life purpose, we should work with them so that it can be achieved. Of course, that is not always possible but it is more likely than we may think.
The book is packed with cases that demonstrate that this is so. Each page is informed by Gawande's clinical experiences, including interviews with hundreds of patients and family members about their experiences of illness and ageing, as well as discussions with health care workers including aged care, nursing, palliative care specialists, geriatricians and other experts in the field.
Gawande's arguments derive from, and are informed by, the immediacy of his clinical practice. The book contains eight chapters: The Independent Self, Things Fall Apart, Dependence, Assistance, A Better Life, Letting Go, Hard Conversations, Courage, and a personal epilogue about Gawande's experience as he shared his father's final journey over years with cancer.
Gawande was born to Indian parents (both doctors) in Brooklyn and grew up in Athens, Ohio. He graduated first from Stanford in 1987 and was a Rhodes Scholar in philosophy, politics and economics at Balliol College, Oxford, in 1989. He completed his medical studies at Harvard in 1995. A political activist, he helped the first Clinton presidential campaign and worked on his ill fated health care reform efforts. He has published highly acclaimed articles with The New Yorker on medical matters (including the chapter in this book entitled Letting Go) and became a staff writer there in 1998. He gave the 2014 Reith Lectures on BBC Radio 4 on The Future of Medicine; his first presentation entitled Why do Doctors Fail? He wrote Being mortal at the Rockefeller villa in Bellagio, Italy.
The medical curriculum and mortality
Gawande observes:
I learned about a lot of things in medical school, but mortality wasn't one of them . . . What worried us was knowledge . . . Yet within a few years, when I came to experience surgical training and practice, I encountered patients forced to confront the realities of decline and mortality, and it did not take long to realize how unready I was to help them.
His is not a book about palliative care and certainly not about euthanasia, although both feature in it: rather, it is about discerning together with patients and carers who have entered the twilight zone what their wishes are about the life that lies ahead of them, and then making judicious choices — sometimes heroic, sometimes quiet and low-key — in relation to therapy and support that are most likely to enable and enhance those choices.
People with serious illness have priorities besides simply prolonging their lives. Surveys find that their top concerns include avoiding suffering, strengthening relationships with family and friends, being mentally aware [even at the expense of foregoing narcotic analgesics], not being a burden on others, and achieving a sense that their life is complete . . . The question therefore is not how we can afford [our system of technological care]. It is how we can build a health care system that will actually help people achieve what's important to them at the end of their lives.
Gawande heads up a health system innovation centre at Harvard.
Gawande's book is a gallery of portraits of patients, carers and doctors and a document of conversations with them that reassure, challenge and inspire. Oliver Sacks, himself a great medical writer, says:
Being Mortal is not only wise and deeply moving, it is an essential and insightful book for our times, as one would expect from Atul Gawande, one of our finest physician writers.1
Late for Christmas? Consider giving yourself a copy for the new year!
- Stephen Leeder1
- 1. Atul Gawande. Being mortal: medicine and what matters in the end. http://atulgawande.com/book/being-mortal (accessed Dec 2014).




