The Western Australian Audit of Surgical Mortality (WAASM) is an external, independent, peer-reviewed audit of deaths of patients in hospital while under the care of a surgeon. A pilot based on the Scottish Audit of Surgical Mortality commenced in 2001,1 and the program expanded to the whole state in 2002. The Royal Australasian College of Surgeons (RACS) established the Australian and New Zealand Audit of Surgical Mortality (ANZASM) in 2005.2
Here, we review WAASM from 1 January 2002 to 31 December 2011.
Detailed methods are available in the WAASM annual reports.3 In brief, hospitals notify WAASM of deaths of patients that occur while under the care of a surgeon. Notification is independent of the surgeon. WAASM sends the treating surgeon a semistructured proforma, which is completed, returned and scrutinised by a first-line assessor.
WAASM is protected under the Commonwealth Qualified Privilege Scheme.4
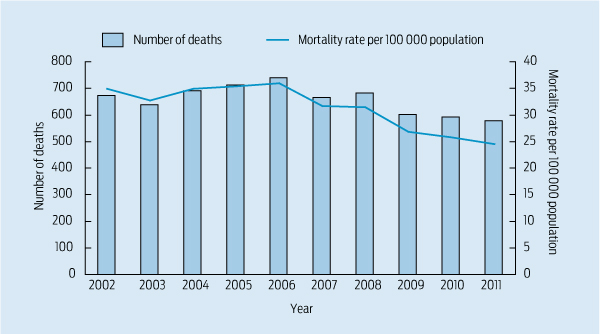
In the first 10 years of WAASM, the annual number of deaths peaked at 740 in 2006, before falling 22.0% to 577 in 2011 (Box). During the audit period, the population of Western Australia increased 22% from 1.9 to 2.3 million.5 Surgical deaths per 100 000 population fell 31.7% from a peak of 35.9 in 2006 to 24.6 in 2011 (an overall fall of 29.6% from 2002 to 2011). The regression trend in deaths per 100 000 population was fitted with the R statistical language using a restricted cubic spline with five knots. Both the regression (P = 0.002) and its non-linear component (P = 0.001) were statistically significant. Deaths per 100 000 surgical separations fell from 35.9 in 2006 to 24.6 in 2011.
Following are some representative examples that illustrate how WAASM influenced care.
In 2004, WAASM reported that a consultant was present for less than half of the operations undertaken in teaching hospitals after which the patient died.3 The teaching hospitals used these data to advocate for the separation of emergency and elective general surgery. In 2006, the WA Department of Health agreed to separate emergency and elective general surgery in teaching hospitals, and established an “on-call day surgeon” with access to a daytime emergency theatre. Between 2002 and 2011, the number of deaths after emergency surgery fell by 22% overall and by 38% for patients aged 65 years or older. Data from Perth underpinned the RACS position paper on the separation of emergency and elective surgery.6
The United Kingdom’s National Confidential Enquiry into Patient Outcome and Death and the Scottish Audit of Surgical Mortality have both recently emphasised the importance of early consultant input in managing emergency patients.7,8
In early reports, WAASM noted that teaching hospital consultants directly performed or assisted in only 40% of first returns to theatre and 35% of second returns. By 2012, these rates of consultant supervision had risen to 51% and 57%, respectively.9 In 2009, ANZASM found consultant participation in WA was greater than in other states.10
An early observation was the failure to appropriately administer deep vein thrombosis prophylaxis. WAASM hosted a symposium on this issue in 2003 and continues to highlight such failures. Subsequent data have demonstrated a fall in the number of deaths secondary to a pulmonary embolus. WAASM concerns preceded publication of the Australian guidelines on prevention of venous thromboembolism.11
Poor postoperative fluid management is an international problem. In 2008, WAASM hosted a symposium that included a Scottish anaesthetist who had been involved in the production of the Scottish Intercollegiate Guidelines on postoperative management.12 Subsequently, there has been a fall in the number of deaths associated with poor fluid management (52 in 2007, nine in 2011). Nationally, poor fluid management remains a problem.13
WAASM noted that death after pancreaticoduodenectomy (Whipple resection) was occurring more frequently than expected, and a statewide analysis confirmed a postoperative mortality rate of 16%, compared with an expected rate of around 2%.14 A working party chaired by WA’s Chief Medical Officer determined that major pancreatic resections should only be undertaken in teaching hospitals with the appropriate personnel and multidisciplinary support. In the past 2 years (May 2010 to May 2012), there have been no deaths after a Whipple resection.
This is an area of current national and international concern.15 WAASM has repeatedly reported that delay in recognising deterioration in a patient’s condition is the leading cause of death. In 2011, WAASM hosted a multidisciplinary symposium on clinical deterioration, with the most important feedback being that nurses better understood the detrimental impact of delay and the importance of escalating care early.16
During its first 10 years, WAASM recorded a 30% reduction in the number of deaths per 100 000 population. The pattern observed — no initial change while data are collected, analysed and disseminated, followed by improved outcomes — is in keeping with numerous surgical audits.19-21 Recent examples of audits incorporating external peer review and risk-adjusted data are the American College of Surgeons National Surgical Quality Improvement Program, which recorded decreases in both mortality and morbidity during its first 10 years,22 and the UK’s National Adult Cardiac Surgery Audit that showed a 25% reduction in mortality, with outcomes now superior to the European average.23
Second, it is highly likely that the Hawthorne effect — where those under observation change their practice — contributed to these changes.24 For example, as a consequence of restricting pancreatectomies to teaching hospitals, most upper gastrointestinal cancer resections now occur in the same institutions. It is also highly likely that some patients avoided secondary complications, and thus death, because of increased consultant presence during returns to theatre.
These observations are in keeping with reports suggesting that any difference in outcome between high- and low-volume surgeons and hospitals may not be related to the initial complication rate, but to the management of complications — so-called failure to rescue.25-28 These studies suggest that initial complications are usually related to patient factors, such as advanced age and medical comorbidities, and rates are similar in high- and low-volume hospitals. The ability to rescue patients after an initial complication seems to depend on facilities found in large hospitals, such as high nurse-to-patient ratios, junior staff, high-dependency units, interventional radiologists and cardiologists, and greater consultant availability.28 Failure to rescue may be five times higher in poorly performing hospitals and it is likely this, rather than the initial complication rate, that determines differences in outcome.
The hallmark feature of WAASM is its external, independent, blind peer review. WAASM has found that treating surgeons only record 18% of the deficiencies of care that are identified by external reviewers.29 External review is normal in other safety-critical industries. The case-note review booklets given to surgeons have consistently been identified as providing the most valued feedback.
Although all WA surgeons now participate in WAASM, this has taken 10 years to achieve. In 2002, many surgeons expressed reservations about personal and medicolegal consequences of participation. Without qualified privilege, WAASM would never have commenced. Although perceived medicolegal concerns have not been borne out, some surgeons remain resistant to participation or complete the proformas in a less than satisfactory manner. This has been an issue in other audits.30 The RACS has recognised that non-participation is no longer defensible. Since 2010, participation in ANZASM has been a mandatory part of its Continuous Professional Development Program, and the proportion of Fellows verified has increased. A current certificate is essential to register with the Medical Board of Australia.
Hospitals and health departments need to accept responsibility when audits demonstrate a need for service redesign. Although there is overwhelming evidence to support the separation of emergency and elective surgical patients, there has been some reluctance to undertake the fundamental reorganisation required.31
A natural progression is open publication of outcome data. Those who pay for health care (governments) and those who use it (the public) want to know what they are purchasing and using. The profession should rise to the challenge of agreeing to greater transparency.32 Identifying regions in ANZASM reports would be an appropriate start.
Provenance: Not commissioned; externally peer reviewed.
- Diana G Azzam1
- C Adeline Neo1
- Franca E Itotoh1
- R James Aitken1,2
- 1 The Western Australian Audit of Surgical Mortality, Royal Australasian College of Surgeons (WA), Perth, WA.
- 2 Sir Charles Gairdner Hospital, Perth, WA.
We thank Dr John Field for his statistical advice.
WAASM was initially funded directly by the WA Department of Health (WADH) on a 3-year trial basis. In 2005, after the establishment of ANZASM, the WADH funded WAASM via the RACS. The contract requires WAASM to provide the WADH with reports, to publish regular case-note review booklets and newsletters and to host symposia. WADH-nominated staff attend WAASM management committee meetings. The WADH has never sought to influence, restrict or manage WAASM’s reports. James Aitken was responsible for establishing WAASM and receives funding for oversight.
- 1. Scottish Audit of Surgical Mortality [website]. http://www.sasm.org.uk (accessed Nov 2012).
- 2. Royal Australasian College of Surgeons. Audits of surgical mortality. http://www.surgeons.org/for-health-professionals/audits-and-surgical-research/anzasm (accessed Nov 2012).
- 3. Royal Australasian College of Surgeons. Western Australian Audit of Surgical Mortality annual report 2004. http://www.surgeons.org/media/303897/waasm_annual_report_2004.pdf (accessed Nov 2012).
- 4. Australian Government Department of Health and Ageing. Legislation for the Commonwealth Qualified Privilege Scheme. Part VC of the Health Insurance Act 1973 (gazetted 23 August 2011). http://www.health.gov.au/internet/main/publishing.nsf/Content/qps-legis (accessed Aug 2013).
- 5. Australian Bureau of Statistics. Australian demographic statistics, Dec 2012. Canberra: ABS, 2012. (ABS Cat. No. 3101.0.) http://www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 (accessed Nov 2012).
- 6. Royal Australasian College of Surgeons. Position statement on emergency surgery. Melbourne: RACS, 2008. http://www.surgeons.org/media/311630/FES_FES_2269_P_Position_Statement_Emergency_Surgery.pdf (accessed Nov 2012).
- 7. Martin IC, Mason DG, Stewart J, et al. Emergency admissions: a journey in the right direction? A report of the National Confidential Enquiry into Patient Outcome and Death. London: NCEPOD, 2007. http://www.ncepod.org.uk/2007report1/Downloads/EA_report.pdf (accessed Nov 2012).
- 8. Mullen R, Scollay JM, Hecht G, et al. Death within 48 h — adverse events after general surgical procedures. Surgeon 2012; 10: 1-5.
- 9. Royal Australasian College of Surgeons. Western Australian Audit of Surgical Mortality annual report 2012. http://www.surgeons.org/media/18645340/rpt_2012-09-24_waasm_ar_2012.pdf (accessed Nov 2012).
- 10. Wong TH, Guy G, Babidge W, Maddern GJ. Impact of consultant operative supervision and surgical mortality in Australia. ANZ J Surg 2012; 82: 895-901.
- 11. National Health and Medical Research Council. Clinical practice guideline for the prevention of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to Australian hospitals. Melbourne: NHMRC, 2009. http://www.nhmrc.gov.au/_files_nhmrc/file/nics/programs/vtp/guideline_prevention_venous_thromboembolism.pdf (accessed Nov 2012).
- 12. Scottish Intercollegiate Guidelines Network. Postoperative management in adults. A practical guide to postoperative care for clinical staff. http://www.sign.ac.uk/pdf/sign77.pdf (accessed Nov 2012).
- 13. Royal Australasian College of Surgeons. Australian and New Zealand Audit of Surgical Mortality national report 2011. http://www.surgeons.org/media/18835539/rpt_2013-02-15_anzasm_annual_report_2011_updated.pdf (accessed Mar 2013).
- 14. Samra JS, Bachmann RA, Choi J, et al. One hundred and seventy-eight consecutive pancreatoduodenectomies without mortality: role of the multidisciplinary approach. Hepatobiliary Pancreat Dis Int 2011; 10: 415-421.
- 15. Australian Commission on Safety and Quality in Health Care. Safety and Quality Improvement Guide Standard 9. Recognising and responding to clinical deterioration in acute health care (October 2012). Sydney: ACSQHC, 2012. http://www.safetyandquality.gov.au/wp-content/uploads/2012/10/Standard9_Oct_2012_WEB.pdf (accessed Nov 2012).
- 16. Royal Australasian College of Surgeons. Western Australian Audit of Surgical Mortality annual report 2011. http://www.surgeons.org/media/85747/waasm_annual_report_2011.pdf (accessed Dec 2012).
- 17. Western Australian Review of Mortality. Policy and guidelines for reviewing inpatient deaths — 2008 edition. http://www.safetyandquality.health.wa. gov.au/docs/mortality_review/3_warm_final_2008.pdf (accessed Nov 2012).
- 18. Semmens JB, Mountain JA, Sanfilippo FM, et al. Providers and consumers support the Western Australian Audit of Surgical Mortality. ANZ J Surg 2006; 76: 442-447.
- 19. Wolff AM, Bourke J, Campbell IA, Leembruggen DW. Detecting and reducing hospital adverse events: outcomes of the Wimmera clinical risk management program. Med J Aust 2001; 174: 621-625. <MJA full text>
- 20. Aitken RJ, Nixon SJ, Ruckley CV. Lothian Surgical Audit: a 15-year experience of improvement in surgical practice through regional computerised audit. Lancet 1997; 350: 800-804.
- 21. Wibe A, Møller B, Norstein J, et al; Norwegian Rectal Cancer Group. A national strategic change in treatment policy for rectal cancer — implementation of total mesorectal excision as routine treatment in Norway. A national audit. Dis Colon Rectum 2002; 45: 857-866.
- 22. Khuri SF, Daley J, Henderson WG. The comparative assessment and improvement of quality of surgical care in the Department of Veterans Affairs. Arch Surg 2002; 137: 20-27.
- 23. National Institute for Cardiovascular Outcomes Research. National Adult Cardiac Surgery Audit annual report 2010–2011. http://www.hqip.org.uk/assets/NCAPOP-Library/NCAPOP-2012-13/Adult-Cardiac-Surgery-Report-2010-11-published-2012.pdf (accessed Nov 2012).
- 24. Birkmeyer JD, Dimick JB, Birkmeyer NJ. Measuring the quality of surgical care: structure, process or outcomes. J Am Coll Surg 2004; 198: 626-632.
- 25. Silber JH, Williams SV, Krakauer H, Schwartz JS. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Med Care 1992; 30: 615-629.
- 26. Silber JH, Rosenbaum PR, Trudeau ME, et al. Changes in prognosis after the first postoperative complication. Med Care 2005; 43: 122-131.
- 27. Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in Medicare patients. Ann Surg 2009; 250: 1029-1034.
- 28. Ghaferi AA, Osborne NH, Birkmeyer JD, Dimick JB. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg 2010; 211: 325-330.
- 29. Royal Australasian College of Surgeons. Western Australian Audit of Surgical Mortality annual report 2010. http://www.surgeons.org/media/18782994/rpt_2010-09-22_waasm_ar_2010.pdf (accessed Nov 2012).
- 30. Beiles CB, Bourke B, Thomson I. Results from the Australasian Vascular Surgical Audit: the inaugural year. ANZ J Surg 2012; 82: 105-111.
- 31. Stokes B. Four Hour Rule Program progress and issues review. December 2011. Perth: Department of Health, 2011. http://www.health.wa.gov.au/publications /documents/FourHourRule_Review_Stokes.pdf (accessed Nov 2012).
- 32. Godlee F. Measure your team’s performance, and publish the results. BMJ 2012; 334: e4590.





Summary
The Western Australian Audit of Surgical Mortality (WAASM) is an external, peer-reviewed audit of all deaths that occur in hospital of patients under the care of a surgeon.
We conducted a retrospective analysis of prospective audit data collected from 1 January 2002 to 31 December 2011.
The annual number of deaths peaked in 2006, then fell 22% by 2011. After correcting for population growth, the overall reduction from 2002 to 2011 was 30% (regression analysis, P = 0.002).
Some changes in practice, such as with pancreatic surgery, can be directly attributed to WAASM. There is strong evidence to suggest that WAASM improved other aspects of care, such as thromboembolic prophylaxis, consultant supervision and fluid management.
A shift of high-risk patients to teaching hospitals, where there is a greater ability to “rescue” patients after complications, may have been an important factor in improved outcomes.
This external, peer-reviewed mortality audit has changed surgical practice and reduced deaths. The same process should be applied to other sentinel events, and the lessons learned can also be extended to non-surgical specialties.