Australian doctors must report to the coroner deaths that meet the legislative requirements of the Coroners Act relevant to their jurisdiction. In Victoria, the reporting requirements in section 4 of the Coroners Act 2008 (Vic) include deaths that appear unexpected, unnatural or violent or have resulted directly or indirectly from an accident or injury, or are related to a medical procedure. Despite this legal obligation, there is significant underreporting of deaths to the coroner,1 and medical practitioners have difficulty recognising reportable deaths.2 Non-reporting of reportable deaths limits the ability of the coroners court to fulfil its statutory role in death investigation, particularly in preventing health care-related deaths.3
External cause of death was defined based on the World Health Organization classification as “any death that resulted directly or indirectly from environmental events or circumstances that caused injury, poisoning and other adverse events”. Deaths were included if the cause of death had an external cause code (V01–Y89) in the International statistical classification of diseases and related health problems, 10th revision (ICD-10).4 Deaths were excluded if the coroner determined the death was from natural causes.
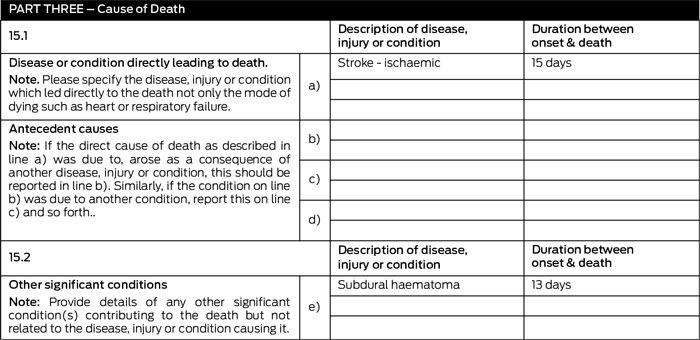
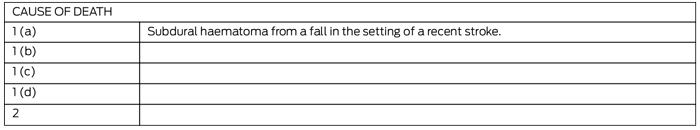
We compared cause of death recorded on the death certificate with cause of death after investigation, and any changes were deemed major, minor or a simple deletion of comorbidities not relevant to cause of death. There are two parts to cause of death on the death certificate. Part 1 is the disease or condition directly leading to death. Part 2 comprises conditions contributing to the death but not related to the disease, injury or illness causing death. We defined a major change as the condition in Part 1 being moved to Part 2 or vice versa, or a new disease or condition not previously recorded being included in Part 1 (Box 1). A minor change was a change in wording or ordering of conditions in Part 1 or the addition of a mechanism of injury (example in Appendix 1). A deletion was removal of comorbidities (Appendix 2).
This study was approved by the Victorian Department of Justice Human Research Ethics Committee.
Nearly all deaths resulted from trauma (Box 2). The three main injuries or complications were fracture complicated by pneumonia, fracture only, and head injury. Of the 190 fracture-related deaths, 142 (74.7%) involved fracture of the femur (including neck of femur) or pelvis. Rib fractures leading to pneumonia were also common. Of the deaths involving head injuries, 81 (76.4%) were from subdural haematomas. Non-trauma-related causes of death were choking, intentional and unintentional poisoning, and transport-related incidents; several deaths had medical procedures recorded in the cause of death field.
Just over half of the deceased (179, 55.9%) were women (Box 3). For both men and women, the highest-frequency age group was 80–89 years. Most deaths occurred in hospitals (219, 68.4%) and in metropolitan Melbourne (221, 69.1%). Almost half (158, 49.4%) occurred in Melbourne-based public and private hospitals. In regional Victoria, deaths were evenly distributed among the major regions.
In just under half of deaths, a major change to the cause of death was made after medical review (Box 4). Only 10 causes of death (3.1%) were not amended. In 309 cases (96.6%), the coroner directed a change to the cause of death to more accurately reflect the condition causing death, the time sequence and causative connection between the listed conditions, the mechanism of injury (eg, fracture sustained in a fall), or any contributing factors (eg, subdural haematoma in the setting of anticoagulation).
In 21 cases (6.6%), the coroner directed that further investigation be undertaken. This comprised:
request for further witness statements from medical, nursing and administrative personnel regarding medical management or other investigation (n = 13)
request to residential aged care facilities to provide policies and protocols on falls prevention and management (n = 4)
referral to the CPU’s Health and Medical Investigation Team for extensive review of health care provided (n = 4).
An inquest into a non-reported death caused by an unintentional heroin overdose was held in the CCOV in 2012 to highlight this problem.5 During the inquest, evidence was given about possible reasons for doctors’ non-reporting of reportable deaths (summarised in Box 5). Ignorance and misunderstanding of the reporting requirements of the Act appear to lie behind many failures to report deaths to the coroner.
Listing mode of death (eg, multiorgan failure, cardiac arrest) rather than a pathological condition (eg, pneumonia, myocardial infarction, dementia) as cause of death
Failure to list conditions in a logical causative sequence
Problems determining whether a condition caused or contributed to the death
Inclusion of conditions unrelated to the death (eg, “glass eye” listed in Part 2). Death certificates should not include all comorbidities, just the causative disease.
Since the 2012 inquest,5 the CCOV has attempted to overcome communication problems between the Court and medical practitioners when they are reporting a death. Coronial recommendations arising from the inquest included that health services should ensure medical practitioners are appropriately educated and made aware of their legal obligations, and that hospitals should develop a system of senior medical peer review of the cause of death before submission to BDM. The Australian Health Practitioner Regulation Agency has responded6 by preparing an educational article for all registered medical practitioners in Australia.7
3 Deaths referred by BDM to Coroners Court of Victoria, July 2010 – June 2011, by age group and sex of the deceased
4 Frequency and nature of changes to cause of death in death certificates referred by BDM to Coroners Court of Victoria, July 2010 – June 2011
5 Possible reasons for doctors’ non-reporting of reportable deaths5
Difficulty in understanding their statutory obligations, possibly due to differing medical and legal interpretations of terms such as “unexpected” or “unnatural” death
Communication problems between doctors and Court staff when doctors attempt to report a death or obtain advice about whether a death is reportable
Difficulty in understanding the causal connection between trauma and the death, particularly when events are separated in time (eg, traumatic spinal or brain injuries or fractures may cause death a long time after the injury). Together with factors including prolonged care, transfer between facilities and involvement of multiple medical practitioners over time, this may result in the reportability of the death, as related to the original injury, not being considered
Difficulty determining whether deaths related to medical procedures are reportable
The potential for junior doctors who correctly believe that a death is reportable to be advised otherwise by senior medical colleagues
Misconceptions that deaths are only reportable when they are “suspicious”. Practitioners may recognise that injury has contributed to death but because the death is not suspicious, they believe the death is not reportable
Misconceptions that families’ objections to autopsy should be considered before reporting
Received 26 February 2013, accepted 29 May 2013
- Sandra L Neate1
- Lyndal C Bugeja1
- George A Jelinek1
- Heather M Spooner1
- Luke Ding1
- David L Ranson2
- 1 Coroners Prevention Unit, Coroners Court of Victoria, Melbourne, VIC.
- 2 Victorian Institute of Forensic Medicine, Melbourne, VIC.
Heather Spooner is the coroner who made the relevant findings in the 2012 inquest discussed in this article.
- 1. Charles A, Ranson D, Bohensky M, Ibrahim JE. Under-reporting of deaths to the coroner by doctors: a retrospective review of deaths in two hospitals in Melbourne, Australia. Int J Qual Health Care 2007; 19: 232-236.
- 2. Start RD, Delargy-Aziz Y, Dorries CP, et al. Clinicians and the coronial system: ability of clinicians to recognise reportable deaths. BMJ 1993; 306: 1038-1041.
- 3. Ibrahim JE, Ranson DL, O’Brien A, et al. Forensic investigation of medical treatment related deaths. Leg Med (Tokyo) 2009; 11 Suppl 1: S71-S75.
- 4. World Health Organization. International statistical classification of diseases and related health problems, 10th revision (ICD-10). Chapter XX: External causes of morbidity and mortality. Geneva: WHO, 2010.
- 5. Coroners Court of Victoria. Finding: inquest into the death of Fikri Memedovski. Melbourne: CCOV, 2012. http://www.coronerscourt.vic.gov.au/home/coroners+written+findings/findings+-+inquest+into+the+death+of+fikri+memedov ski (accessed Feb 2013).
- 6. Flynn J; Medical Board of Australia. Response: Investigation into the death of Fikri Memedovski. Melbourne: MBA, 2013. http://www.coroners court.vic.gov.au/resources/77f07c52-d727-4479-a028-b350dc3f9bb8/responsemedicalboard aust_memedovski.pdf (accessed Feb 2013).
- 7. Medical Board of Australia. From the coroner. Update 2013; (6): 3. http://www.medicalboard. gov.au/News/Newsletters/June-2013.aspx (accessed Aug 2013).





Abstract
Objective: To better understand the non-reporting of reportable deaths by determining the frequency and nature of reportable deaths referred to the Coroners Court of Victoria (CCOV) by the Registry of Births, Deaths and Marriages (BDM).
Design and setting: Review of referrals from BDM to the CCOV between 2003 and 2011 where an external cause of death was recorded on the death certificate, with detailed review for the period 1 July 2010 to 30 June 2011.
Main outcome measures: Frequency and nature of deaths referred, accuracy of cause of death recorded on death certificate, and degree of change made to cause of death after investigation.
Results: Over 9 years, there were 4283 referrals (annual mean, 476). Of 656 deaths referred between 1 July 2010 and 30 June 2011, 320 (48.8%) were found to be reportable. Most causes of death related to injuries; less common were choking, deaths after medical procedures, poisoning and transport-related deaths. Most of the deceased were women (55.9%), were aged ≥ 80 years (80.0%), and died in hospital (68.4%). In 309 cases (96.6%), the coroner changed the cause of death after investigation, with a major change in 146 (45.6%), minor change in 160 (50.0%), and deletion of comorbidities in three (0.9%). Twenty-one cases (6.6%) were investigated further, with one proceeding to an inquest.
Conclusions: Deaths referred by BDM represent a proportion of the unquantified pool of non-reported deaths. Non-reporting of potentially reportable deaths and inaccurate completion of death certificates have significant implications for the health system and community. Further education of medical practitioners about reportable deaths and death certificates is required. Doctors should report any death about which they have doubt.