This is a republished version of an article previously published in MJA Open
Cancer is a life-threatening and dreaded illness. Its treatments can have direct organic effects on mood; interactions can occur between antidepressants and chemotherapy agents; and, as patients undergo cancer treatment, they may be debilitated, immunosuppressed, underweight and in pain for considerable periods of time. When active cancer treatment is complete, patients often have to adjust to changes in body function, persistent pain, alterations in role and sense of self, and the possibility of cancer recurrence. All these factors put patients with cancer at increased risk of depression,1,2 which can have consequences including reduced quality of life,3,4 greater risk of cancer mortality5 and higher risk of suicide.6,7 A particular challenge can be persuading a patient to accept treatment for depression at the same time as onerous cancer treatment. Early detection of depression and expeditious commencement of treatment can be difficult to achieve in the context of complex and busy cancer treatment protocols.
Although evidence shows that psychosocial interventions can effectively prevent poor mental health outcomes for many people diagnosed with cancer, the health system, faced with an ever-growing demand on cancer treatment programs, has yet to fully integrate the psychological and biological aspects of comprehensive cancer care.8 Psycho-oncology services remain largely reactive and referral-based at large treating centres in Australia, and are minimal or non-existent at smaller centres, despite longstanding calls for their wider implementation.
Many people with cancer are distressed but will not meet Diagnostic and statistical manual of mental disorders, 4th edition, text revision (DSM-IV-TR)9 criteria for a diagnosis of an anxiety disorder or major depression. This has led to recognition in the field of psycho-oncology of the broader concept of psychological distress, now considered the sixth vital sign in cancer (pain being the fifth).10 Multiple factors will affect a person’s capacity to manage the physical and psychological threat of a new cancer diagnosis, including past experiences of illness (including other cancers), stage of disease at diagnosis, the quality and accuracy of information received about current disease and treatments, and the communication skills and perceived availability of health care professionals.11,12
In the past decade, the trend towards use of screening tools to detect distress has grown. Problem checklists and the use of visual analogue scales, such as the “distress thermometer” (Box 1),10 have shown the most promise. It is recommended that GPs routinely screen patients diagnosed with cancer for distress. In the process of this screening, GPs can normalise the experience of mild to moderate distress for the patient and reassure him or her that it is normal and appropriate to seek psychological support if distressing emotions persist or become intense and affect normal function (Box 2).
Although the prevalence depends on exact definitions, depressive disorders are said to occur in up to half of patients with cancer,2,13 with a prevalence of more strictly defined major depression estimated to be 10%–25%.14
Existential distress is a particular form of distress that occurs in the context of a life-threatening illness such as cancer and may initially resemble a depressive state. It is characterised by loss of meaning and purpose, or the sense that one’s fundamental frame of reference for life is being challenged. One characterisation of existential distress that appears to have clinical utility is “demoralisation syndrome”,15 a clinical state that encompasses helplessness, hopelessness, meaninglessness, subjective incompetence and loss of self-esteem. Modes of psychotherapy that directly address existential distress and demoralisation syndrome have been developed by psycho-oncology researchers.
The DSM-IV-TR criteria for major depression9 are predicated on the assumption that the patient is generally physically well, so that neurovegetative symptoms (weight loss, sleep disturbance, fatigue) can be used to establish the presence and severity of a depressive episode. Patients with cancer receiving oncological treatment present a classification problem using this diagnostic system, because many of their symptoms may be due to the cancer or its treatment rather than to depression. In patients with cancer, the cognitive symptoms of depression (guilt, low self-esteem, hopelessness, helplessness, feeling useless or a burden, suicidal thoughts) are therefore especially important in diagnosis and in monitoring response to treatment.16 It is important that doctors managing patients with cancer are alert to these cognitive symptoms and seek expert psychiatric assessment of the patient’s mood, rather than dismissing such symptoms as an expected or normal response to having cancer.
Through the Medicare-funded Better Access initiative, many GPs now have links to community-based psychologists. In some situations, a community-based psychologist who does not have specific training or expertise in the cancer setting may be able to offer the necessary support. However, in other circumstances, the patient may prefer to see or may require a more specialised clinician, and a referral to a specialist psycho-oncology service should be made (Box 3).
For other issues that may be managed by referral to a psycho-oncology service, see Box 3.
It is thought that some types of cancer cause a depressed mood through humoral effects (cytokines)17 and possibly through dysregulation of cell-mediated immune function. Direct mass effects in the brain or infiltration of the meninges can also potentially cause alterations in mood, as can any intracranial space-occupying lesion.
Corticosteroids (dexamethasone, prednisolone) are an integral part of many chemotherapy protocols and are also used for control of nausea and reduction of tumour swelling (especially in the brain). The high doses of corticosteroids used in many cancer treatment protocols often lead to mood disturbance, most often characterised by a mild hypomania as the dose is increased, and a depressed mood as the dose is reduced or ceased.18
Chemotherapy drugs, including vinblastine, etoposide, cyclophosphamide and protein-bound paclitaxel, interleukin-β (used in the treatment of multiple myeloma) and interferon-α (used for some leukaemias and melanomas) have all been described as causing or contributing to depressed mood in some patients.16 Some cancer treatments will affect hormone function, with potential adverse mood and cognitive side effects (eg, medically induced menopause after oophorectomy, or androgen ablation in prostate cancer treatment).19,20 As many patients now receive chemotherapy and/or hormone therapy as day patients, the cancer centre team may not notice mood changes that may instead come to the attention of the patient’s family or GP.
The psychological stress and the direct biological effects of the cancer and its treatment all act to increase the incidence of depression and the likelihood of relapse of pre-existing depressive illness. Antidepressant therapy tailored to the symptom profile can treat major depression in the presence of cancer, and can also relieve some of the other common symptoms experienced with cancer (anxiety, insomnia, anorexia, nausea, agitation, fatigue, loss of motivation, pain, pruritus and hot flushes).21,22 The evidence base for the use of particular antidepressants in cancer, particularly in the palliative care setting, is not strong, due to the paucity of research.23,24 In choosing from a range of equally effective second-generation antidepressants,25 psychiatrists in specialist psycho-oncology services take into consideration the patient’s symptom profile, ambulatory versus palliative care status, comorbid illnesses, desired and undesired drug side effects, and potential drug interactions. Close liaison between the psychiatrist, the oncology team and the GP is necessary to ensure selection of the most appropriate antidepressant for the individual patient.
In some circumstances, a previously effective antidepressant will have to be discontinued because of interactions with chemotherapy or adjuvant treatments. As with the use of antidepressants during pregnancy, GPs are advised to seek an expert psychiatric opinion, as recommendations change and interactions between new antidepressants and new cancer treatments continue to be discovered.26,27
Psychotherapeutic support can be of great benefit to many patients and their families facing life-threatening illness. In its simplest form, this may be through empathic, active listening at times of distress. All clinicians, including GPs, who are involved with cancer patients and their families are advised to develop essential communication skills through available programs. A suggested general approach for GPs is shown in Box 2. Psycho-oncology services can provide specialised psychotherapy services that may include individual, couple, family or group therapies.
A number of modes of psychotherapy have been developed and studied for different cancer populations. A comprehensive account of psychotherapies in cancer care can be found elsewhere;28 we discuss some of these briefly here.
All encounters with patients and their families have the potential to be psychotherapeutic, but for more complex and ongoing issues, skilled therapists with special knowledge of cancer and the nature and impact of treatment are recommended. Flexibility with approach and model is often required at different stages of the patient’s experience.
1 The distress thermometer*
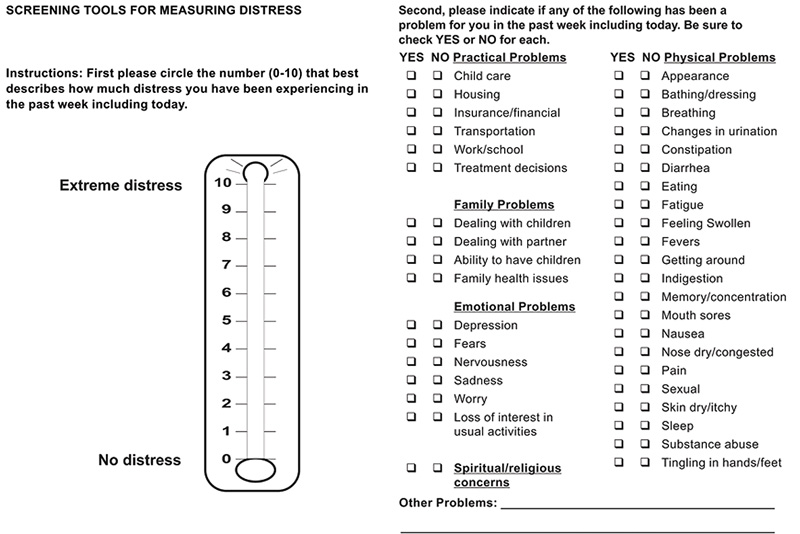
* Reproduced with permission from the National Comprehensive Cancer Network (NCCN) clinical practice guidelines in oncology for distress management (V.1.2013). © 2012 National Comprehensive Cancer Network. Available at http://www.ccn.org (accessed Aug 2012).
2 Good practice points for general practitioners
Maintaining a supportive therapeutic presence
Screening for psychological distress at regular intervals, with particular emphasis on enquiring about distress at times of increased risk (eg, receiving bad news, ending treatment, a diagnosis of or transition to advanced or incurable disease, and transition to palliative care)
Assessing family functioning, with referrals to family therapy (especially where there are dependent children under the age of 18 years)
Making referrals for psychological support to a community psychologist under the Medicare Better Access initiative or to a specialist psycho-oncology service at a cancer centre, as needed
Problem solving and education about ongoing health risks, including importance of lifestyle change and future cancer screening
3 When to refer to a community psychologist or a specialist psycho-oncology service
Refer to a community psychologist for:
Mild–moderate psychological distress
Pre-existing family relationship problems
Worries about young or dependent children
Family or caregiver conflicts
Employment-related concerns
Longstanding interpersonal difficulties
Social isolation
History of abuse (physical or sexual)
Normal grief and bereavement
Refer to a psycho-oncology service for:
Moderate–severe distress related to cancer diagnosis and treatment
Longer-term adjustment difficulties and existential distress associated with cancer
Past psychiatric history or alcohol and drug misuse
Significant mood change
Advanced disease at diagnosis
Advice on choice of antidepressant and/or mood stabiliser
Benefit from cancer-specific psychotherapy programs
Competency issues, cognitive change, neuropsychiatric symptoms
Refusal to comply with recommended treatment for unclear reasons
Conflict with cancer-treating team
Difficulty deciding between cancer treatment options
Anxiety out of proportion to prognosis
Phobic reactions to specific aspects of cancer treatment
Familial cancer concerns
Prophylactic cancer treatments to manage familial cancer risk (eg, mastectomy)
Concerns about loss of fertility due to cancer treatment
Treatments that will result in major loss of function or body part (eg, permanent stoma, amputation)
Major disfigurement or change in appearance
Long-term debilitating cancer treatment
Risk of self-harm or harm to others
Provenance: Commissioned by supplement editors; externally peer reviewed.
- Jeremy W Couper1,2,3
- Annabel C Pollard1
- Dianne A Clifton3
- 1 Peter MacCallum Cancer Centre, Melbourne, VIC.
- 2 Department of Psychiatry, University of Melbourne, Melbourne, VIC.
- 3 St Vincent’s Hospital, Melbourne, VIC.
No relevant disclosures.
- 1. Chochinov HM. Depression in cancer patients. Lancet Oncol 2001; 2: 499-505.
- 2. Reich M, Lesur A, Perdrizet-Chevallier C. Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Res Treat 2008; 110: 9-17.
- 3. Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr 2004; (32): 57-71.
- 4. Smith EM, Gomm SA, Dickens CM. Assessing the independent contribution to quality of life from anxiety and depression in advanced cancer. Palliat Med 2003; 17: 509-513.
- 5. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer 2009; 115: 5349-5361.
- 6. Robson A, Scrutton F, Wilkinson L, MacLeod F. The risk of suicide in cancer patients: a review of the literature. Psychooncology 2010; 19: 1250-1258.
- 7. Fang F, Fall K, Mittleman MA, et al. Suicide and cardiovascular death after a cancer diagnosis. N Engl J Med 2012; 366: 1310-1318.
- 8. Clarke DM. No cancer health without mental health. Med J Aust 2010; 193 (5 Suppl): S43. <MJA full text>
- 9. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Publishing, 2000.
- 10. Holland JC, Bultz BD; National Comprehensive Cancer Network. The NCCN guideline for distress management: a case for making distress the sixth vital sign. J Natl Compr Canc Netw 2007; 5: 3-7.
- 11. Maguire P, Pitceathly C. Key communication skills and how to acquire them. BMJ 2002; 325: 697-700.
- 12. Butow P, Gilchrist J. How to build relationships with good communication. In: Hodgkinson K, Gilchrist J, editors. Psychosocial care of cancer patients: a health professional’s guide of what to say and do. Melbourne: Ausmed, 2008.
- 13. Brintzenhofe-Szoc KM, Levin TT, Li Y, et al. Mixed anxiety/depression symptoms in a large cancer cohort: prevalence by cancer type. Psychosomatics 2009; 50: 383-391.
- 14. Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 2011; 12: 160-174.
- 15. Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry 2002; 36: 733-742.
- 16. Rackley S, Bostwick JM. Depression in medically ill patients. Psychiatr Clin North Am 2012; 35: 231-247.
- 17. Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry 2009; 65: 732-741.
- 18. Stiefel FC, Breitbart WS, Holland JC. Corticosteroids in cancer: neuropsychiatric complications. Cancer Invest 1989; 7: 479-491.
- 19. Ganz PA. Menopause and breast cancer: symptoms, late effects, and their management. Semin Oncol 2001; 28: 274-283.
- 20. Couper JW, Love AW, Dunai JV, et al. The psychological aftermath of prostate cancer treatment choices: a comparison of depression, anxiety and quality of life outcomes over the 12 months following diagnosis. Med J Aust 2009; 190 (7 Suppl): S86-S89. <MJA full text>
- 21. Grassi L, Nanni MG, Uchitomi Y, Riba M. Pharmacotherapy of depression in people with cancer. In: Kissane DW, Maj M, Sartorius N, editors. Depression and cancer. Chichester, UK: John Wiley & Sons, 2010: 151-176.
- 22. Schwartz TL, Uderitz D. Tailoring antidepressant treatment: factors to individualize medication selection. Medscape Education 2011. http://www.medscape.org/viewarticle/755180 (accessed Dec 2011).
- 23. Rodin G, Lloyd N, Katz M, et al; Supportive Care Guidelines Group of Cancer Care Ontario Program in Evidence-Based Care. The treatment of depression in cancer patients: a systematic review. Support Care Cancer 2007; 15: 123-136.
- 24. Rayner L, Price A, Hoptof M, Higginson IJ. The development of evidence-based European guidelines on the management of depression in palliative cancer care. Eur J Cancer 2011; 47: 702-712.
- 25. Morgan LC, Gartlehner G, Richard HA. Comparative effectiveness of second generation antidepressants in the pharmacologic treatment of adult depression. Eur Psychiatry 2012; 27: 1102.
- 26. Breitbart W. Do antidepressants reduce the effectiveness of tamoxifen? Psychooncology 2011; 20: 1-4.
- 27. Yap KY, Tay WL, Chui WK, Chan A. Clinically relevant drug interactions between anticancer drugs and psychotropic agents. Eur J Cancer Care (Engl) 2011; 20: 6-32.
- 28. Watson M, Kissane DW, editors. Handbook of psychotherapy in cancer care. Chichester, UK: John Wiley & Sons, 2011.





Summary
Depression in patients with cancer can present a challenging clinical problem for both general practitioners and the oncology team.
Detecting depression in a patient with cancer, who may be debilitated and in pain, can be difficult.
Cancer treatments can complicate antidepressant choices.
Community-based psychologists are an important resource for helping manage less complex and less severe psychological problems that can arise in the cancer setting.
Specialist psycho-oncology services (where available) can help with more complex and severe presentations of depression by advising on the prescription of antidepressants and providing psychotherapy programs that address the patient’s psychological orientation and needs and consider the patient’s cancer type and stage.