This is a republished version of an article previously published in MJA Open
In Australia, about 23% of children live in households where at least one parent has a mental health issue.1 While many parents with a mental illness are able to cope well with parenting and some children show little, if any, adverse outcomes,2 there is a strong association between parental mental illness and poor outcomes in children.3 Many parents with mental health problems are reluctant to seek help because of the stigma that surrounds mental illness.4 This stigma is often associated with the fear of custody loss and can keep parents from acknowledging problems, particularly in relation to parenting and requesting services.4-6
Of the interventions targeting family relationships and parenting in families, behavioural family interventions founded on social learning models have the greatest empirical support.7,8 The Positive Parenting Program (Triple P)9 is a well established behavioural family intervention that has been successfully adapted to a number of different populations. Some of these include overweight and obese children,10 Indigenous families11 and working parents.12 Currently, there are very limited parenting interventions available for parents with mental illness.
In recognising the need for such services, Central Coast Children and Young People’s Mental Health (CYPMH) developed the Mental Health Positive Parenting Program (MHPPP).13 The MHPPP is an adaptation of the Triple P, retaining the four fundamental sessions and incorporating an additional two sessions: “The impact of mental health on parenting” and “Children’s fears, friendships and schooling”. These sessions were developed from recommendations from both clinicians and parents with mental illness who completed the Triple P in an earlier intervention.14 “The impact of mental health on parenting” involves parents exploring their thoughts, feelings and behaviours when they are unwell in the context of their parenting, then linking their responses back to the Triple P principles. This process aims to increase parental insight and encourages them to plan parenting strategies to manage future periods of being unwell. “Children’s fears, friendships and schooling” involves parents identifying appropriate expectations of children across different ages regarding their fears, friendships and schooling. This allows parents to identify common concerns and apply parenting strategies that support children’s development in these areas. The MHPPP also varies from the Triple P in that it replaces the four follow-up phone calls with four weekly home visits. This allows facilitators to assist parents to apply their learnt skills in the home environment, model effective parenting strategies and create opportunities to talk directly with children, where appropriate, about their parent’s mental health problem.
In 2005, CYPMH ran a pilot study of 19 families, to investigate the effectiveness of the MHPPP.13 The pilot study found that following the MHPPP, parents with mental health issues reported a reduction in both dysfunctional parenting strategies and children’s behavioural problems. As a result of these encouraging findings, the present study aimed to replicate the pilot study with a larger sample and across a greater number of settings. We report a before- and after-intervention evaluation of the MHPPP with a larger sample of parents with mental health problems.
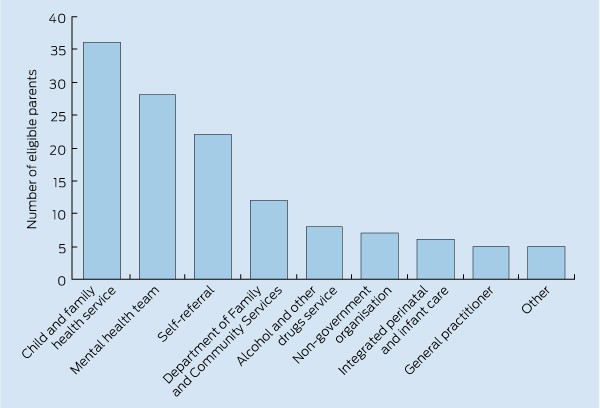
A detailed explanation of the participant criteria has previously been provided.13 Principally, participants were eligible if they were parents of children aged 2–10 years and self-reported a mental health problem. The referral pathways by which participants were recruited are shown in Box 1.
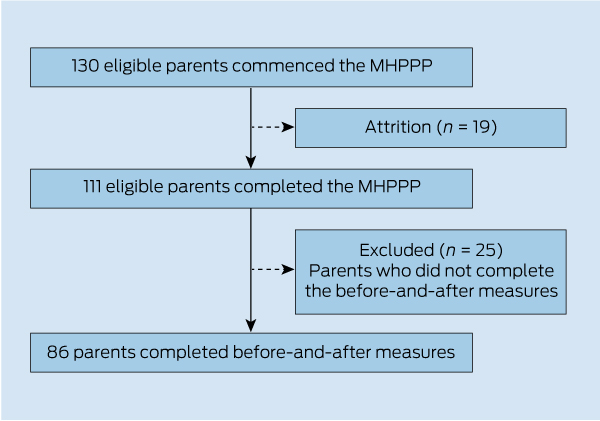
Between July 2005 and February 2011, 23 groups undertook the MHPPP in four community health centres across two local government areas. In total, 130 parents commenced the program and 111 (85.4%) parents completed the program. Of the 111 parents who completed the program, 86 (77.5%) completed both the before- and after-MHPPP measures. This paper reports on data provided from these 86 participants. The movement of participants through the program is shown in Box 2.
The Eyberg Child Behavior Inventory (ECBI)15 was used to measure parent perceptions of behavioural problems in their children. The 36-item questionnaire comprises two subscales, which assess the frequency in which the behaviour occurs (intensity subscale) and its identification as a problem (problem subscale). The intensity subscale requires parents to indicate the frequency with which each behaviour occurs, using a 7-point Likert scale ranging from 1 (never) to 7 (always). Scores range from 36 to 252, with higher scores indicating greater frequency of behaviour. Intensity scores > 132 are considered to be in the clinical range.15 The problem subscale requires the parent to indicate whether a behaviour is currently a problem for them (1 = yes, 0 = no). Scores range from 0 to 36, with higher scores indicating a greater number of child behaviour problems. Scores > 15 on the problem subscale are considered to be in the clinical range.15 The ECBI has good reliability with test–retest coefficients of 0.86 for intensity and 0.88 for problem scores.16 The ECBI has also demonstrated good construct and concurrent validity.17,18
The Parenting Scale (PS)19 is a 30-item self-report measure that assesses parent discipline practices. The PS requires parents to indicate their tendencies to employ each of the discipline strategies on a 7-point Likert scale from 1 (high probability of selecting an effective discipline strategy) to 7 (high probability of selecting an ineffective discipline strategy). PS scores above 3.2 for laxness, 3.1 for over-reactivity and 4.1 for verbosity are considered to be in the clinical range.19 The PS has good reliability, with high test–retest reliability over a 2-week period in a combined sample of clinical and non-clinical children (laxness, r = 0.83; over-reactivity, r = 0.82; verbosity, r = 0.79).19 The PS has good concurrent and convergent validity.19
There were no significant differences between the characteristics of parents who completed the before- and after-MHPPP measures and of those who did not complete the measures (Box 3).
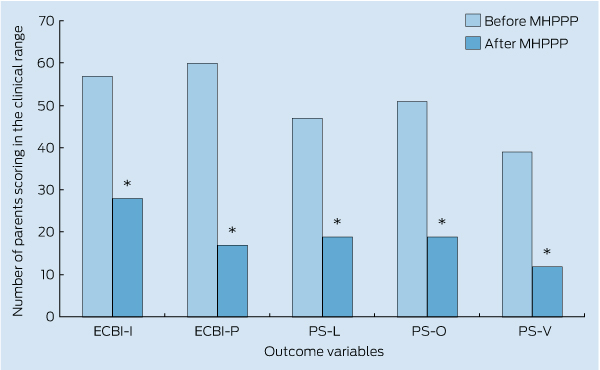
Clinical improvement: The numbers of parents who scored in the clinical range on each of the outcome measures before and after the MHPPP are shown in Box 4. A series of McNemar’s tests demonstrated that significantly fewer (P < 0.001) parents reported in the clinical range on all the outcome measures following the MHPPP.
The results are consistent with our earlier pilot study,13 providing further support for the effectiveness of the MHPPP. The results are also consistent with positive outcomes from studies using adapted versions of the Triple P for different target populations.10-12 Our findings provide preliminary support that an adapted version of the Triple P can be helpful for parents with mental health problems. It is therefore a promising avenue for early intervention in this population.
There are a number of limitations to our study. First, we did not include long-term follow-up measures and therefore are unable to comment on the durability of the intervention effects. However, Triple P has been demonstrated to be well maintained over time, and given the MHPPP is based largely on the Triple P, it is feasible that we would be able to achieve similar results.20 Second, the before-and-after-intervention study design, without a control group, means that we cannot determine the effectiveness of the MHPPP. It is possible that the MHPPP provided no advantage over the basic Triple P. Third, parental mental health problems were self-reported, which means that we may not have accurate information to meet diagnostic criteria. Further, we did not measure the severity of parental mental health problems and are thus unable to report on the degree of impairment in the sample and whether it affected the results.
3 Characteristics of parents who completed the before-and-after measures for the Mental Health Positive Parenting Program (study sample), compared with those who did not (excluded sample)
Provenance: Not commissioned; externally peer reviewed.
Received 19 September 2011, accepted 5 March 2012
- Ruth F Phelan1
- Deborah J Howe2
- Emma L Cashman3
- Samantha H Batchelor4
- Prevention Promotion and Early Intervention, Children and Young People’s Mental Health, Gosford, NSW.
No relevant disclosures.
- 1. Maybery DJ, Reupert AE, Patrick K, et al. Prevalence of parental mental illness in Australian families. The Psychiatrist 2009; 33: 22-26. doi: 10.1192/pb.bp.107.018861.
- 2. Falkov A, Lindsey C, editors. Patients as parents: addressing the needs, including the safety, of children whose parents have mental illness. Council Report CR105. London: Royal College of Psychiatrists, 2002. http://www.londonscb.gov.uk/diary/2008conference/ (accessed Mar 2012).
- 3. Berg-Nielsen TS, Vikan A, Dahl AA. Parenting related to child and parental psychopathology: a descriptive review of the literature. Clin Child Psychol Psychiatr 2002; 7: 529-552. doi: 10.1177/1359104502007004006.
- 4. Nicholson J. Services for parents with mental illness and their families. Journal of the California Alliance for the Mentally Ill 1996; 7: 66-68.
- 5. Hearle J, Plant K, Jenner L, et al. A survey of contact with offspring and assistance with child care among parents with psychotic disorders. Psychiatr Serv 1999; 50: 1354-1356.
- 6. Ackerson BJ. Coping with the dual demands of severe mental illness and parenting: the parents’ perspective. Fam Soc 2003; 84: 109-118.
- 7. Sanders MR. Parenting interventions and the prevention of serious mental health problems in children. Med J Aust 2002; 177 Suppl: S87-S92.
- 8. Patterson GR. A social learning approach to family interventions: III. Coercive family process. Eugene, OR: Castalia Publishing, 1982.
- 9. Sanders MR. Triple P-Positive Parenting Program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev 1999; 2: 71-90.
- 10. West F, Sanders MR, Cleghorn GJ, Davies PS. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behav Res Ther 2010; 48: 1170-1179.
- 11. Turner KM, Richards, M, Sanders MR. Randomised clinical trial of a group parent education programme for Australian Indigenous families. J Paediatr Child Health 2007; 43: 429-437.
- 12. Sanders MR, Stallman HM, McHale M. Workplace Triple P: a controlled evaluation of a parenting intervention for working parents. J Fam Psychol 2011; 25: 581-590.
- 13. Phelan R, Lee L, Howe D, Walter G. Parenting and mental illness: a pilot group programme for parents. Australas Psychiatry 2006; 14: 399-402.
- 14. Howe D. Final report of the Parent Link Project. Sydney: Children and Young People’s Mental Health, Northern Sydney Central Coast Health Service, 2006.
- 15. Eyberg SM, Pincus D. Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory-Revised. Odessa, FLA: Psychological Assessment Resources, 1999.
- 16. Robinson EA, Eyberg SM, Ross WA. The standardisation of an inventory of child conduct problem behaviours. J Clin Child Psychol 1980; 9: 22-28. doi: 10.1080/15374418009532938.
- 17. Eyberg SM, Ross AW. Assessment of child behavior problems: the validation of a new inventory. J Clin Child Psychol 1978; 7: 113-116. doi: 10.1080/15374417809532835.
- 18. Boggs SR, Eyberg S, Reynolds LA. Concurrent validity of the Eyberg Child Behavior Inventory. J Clin Child Psychol 1990; 19: 75-78. doi: 10.1207/s15374424jccp1901_9.
- 19. Arnold DS, O’Leary SG, Wolff LS, Acker MM. The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychol Assessment 1993; 5: 137-144.
- 20. de Graaf I, Speetjens P, Smit F, et al. Effectiveness of the Triple P Positive Parenting Program on behavioral problems in children: a meta-analysis. Behav Modif 2008; 32: 714-735.





Abstract
Objective: To determine the effect of the Mental Health Positive Parenting Program (MHPPP) on parenting practices of parents reporting a mental health problem.
Design, setting and participants: A prospective before-and-after examination of positive parenting skills and parent-reported child outcomes among parents of children aged 2–10 years who had self-reported a mental health problem. One hundred and eleven (85.4%) of 130 parents who commenced the MHPPP completed the program. Of these, 77.5% (n = 86) completed both before- and after-intervention measures. The MHPPP was conducted across four community health centres.
Intervention: A 10-week intervention was tailored to parents with a mental health problem. The intervention was divided into a 6-week group parenting program based on the Positive Parenting Program and four weekly home visits.
Main outcome measures: Parental discipline practices and children’s behaviour were measured by the Parenting Scale (PS) and the Eyberg Child Behavior Inventory (ECBI), respectively.
Results: Following the MHPPP, parents scored significantly lower on each of the PS subscales: laxness (Z = − 6.23; P < 0.001), over-reactivity (Z = − 7.15; P < 0.001) and verbosity (Z = − 6.59; P < 0.001); and significantly lower on both ECBI subscales: intensity (Z = − 7.08, P < 0.001) and problem (Z = − 7.57; P < 0.001).
Conclusions: Our findings suggest the MHPPP can reduce the number of dysfunctional parenting strategies and parent-reported child behavioural problems. The MHPPP is a promising avenue for early intervention in this population.