In high-income countries, lower socioeconomic status is associated with both higher prevalence of non-communicable diseases and less-healthy dietary intake.1 In this context, promoting healthier nutrition, particularly increasing the intake of fruits and vegetables, has become an important public health priority.2 For those on low incomes, it has been argued that the cost of healthier foods is an important barrier to improving nutrition.3 Though not widely implemented in Australia, food subsidy programs are one strategy with the potential to improve socioeconomic inequalities in dietary intake.
In 2005, a rural Aboriginal community-controlled health service initiated a program for providing subsidised fruits and vegetables to improve nutrition among disadvantaged Aboriginal families. This program aimed to engage families in preventive health care in partnership with the health service while also addressing the barrier of the cost of healthier food choices.
Our previously published evaluation of this program demonstrated improvements in biomarkers of fruit and vegetable intake among children.4 We were also interested in whether there were short-term health benefits of this program, which may have been indicative of enhanced functioning of the immune system due to improved nutritional status.5
Here, we report on whether participation in this fruit and vegetable subsidy program in northern New South Wales was associated with short-term improvements in the health of children in participating families using a number of markers, including any changes in episodes of illness, episodes of common clinical conditions, prescription of antibiotics and the prevalence of anaemia and iron deficiency.
The mean and 95% confidence interval of changes in the number of health service visits, common clinical conditions and antibiotic use, anthropometric measurements and levels of haemoglobin, iron and ferritin were evaluated in IBM SPSS Statistics, version 19 using a paired sample t test and a general linear model to adjust for sex, age and community. The mean changes in these outcomes were assessed overall and by community, owing to differences in program implementation in each community. The analysis was based on complete data with no imputation for missing values. Based on an international classification of BMI centiles for age,6 the proportions of children who were underweight, normal weight, overweight and obese before participation were compared with the proportions after participation using the Stuart–Maxwell test of marginal homogeneity. The proportions of children with low haemoglobin, ferritin and iron before and after participation were compared using the McNemar test.
The demographic characteristics of 174 children who participated in the fruit and vegetable program are presented in Box 1. Of these, 167 children had an initial health assessment including anthropometry completed at baseline.
Retrospective clinical audits were completed for 167 children whose families received at least one box of subsidised fruits and vegetables. Seven children did not have clinical audits: three whose families moved from the area, and four whose families were withdrawn from the program for non-compliance with initial assessments.
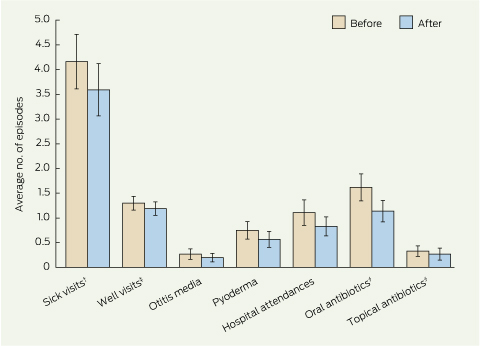
The unadjusted data from clinical audits for the overall sample showed that during program participation the mean annual numbers of visits to any health service for illness, hospital emergency department attendances and oral antibiotic prescriptions were significantly lower (P = 0.037, P = 0.017, P = 0.001, respectively) (Box 2). There was also a non-significant reduction in episodes of pyoderma during program participation (P = 0.093). After adjustment for sex, age and community, only the reductions in illness-related health service or hospital visits and in prescribing of oral antibiotics remained statistically significant (Box 3). An additional adjustment of change scores for the baseline values in the covariate-adjusted models yielded no differences in the conclusions drawn other than a loss of statistical significance for the observed reduction in illness-related visits (− 0.5; 95% CI, − 1.0 to 0.03).
A small, non-significant increase of 1.5 g/L (P = 0.076) in the mean haemoglobin level was shown; this effect increased in magnitude to 3.1 g/L and was statistically significant after adjustment for community, sex and age (Box 4). An additional analysis adjusting for baseline haemoglobin level did not change this conclusion. Comparing the individual communities, a large, statistically significant increase in mean haemoglobin levelwas shown at Bowraville (7.8 g/L) but not in Coffs Harbour or the Clarence Valley (P < 0.001 for difference between communities). The proportion of participants with anaemia decreased by 3% compared with baseline (Box 4). Iron deficiency, based on serum ferritin, was common at baseline (41%). There were small decreases in the proportion of fruit and vegetable program participants with low ferritin and iron levels; however, there were no significant differences in mean serum ferritin and serum iron levels after the fruit and vegetable program compared with baseline with or without adjustment for community, sex and age (Box 4). Additional adjustment for baseline iron and ferritin levels did not change these findings.
Aboriginal children from the NSW north coast who participated in this fruit and vegetable subsidy program had significantly fewer oral antibiotic prescriptions over 12 months compared with the preceding year. The proportion of overweight or obese children after participation in this program did not change. Although height, weight and BMI had all increased significantly at the 12-month follow-up as expected in children, there was no change in the percentage body fat among a subgroup who had this assessed. The prevalence of iron deficiency at baseline was 41%, with anaemia in 8%. There was a small but statistically significant increase in the mean haemoglobin level and a reduction in the proportion of children with anaemia, but only a non-significant 4% decrease in iron deficiency.
Our study demonstrates the potential to undertake evaluation studies in an Aboriginal community-controlled health service, despite the inherent limitations in a busy community-oriented service organisation. It is also an example of an Aboriginal community-directed program, which are far more common than intervention research, although few are documented in academic literature.
The nutritional challenges in this group of disadvantaged Aboriginal children are consistent with those reported in a study of other towns in northern NSW.7 Low intakes of fruits and vegetables and high intakes of energy-dense, nutrient-poor foods were reported among both Aboriginal and Torres Strait Islander and non-Indigenous children aged 9–13 years, with a particularly high intake of sodium, calories, fat, sugary drinks and white bread by Indigenous boys.7 Although the nature of the intervention in our study differed from other nutrition interventions in remote Aboriginal communities, such as the Looma Healthy Lifestyle Program8 in Western Australia and the Minjilang Health and Nutrition Project9 in the Northern Territory, a common feature of these successful programs was strong community engagement. This, together with ongoing relationships, underpins other current Aboriginal community research programs.10,11
Community support for our healthy food program was fostered by the 88% subsidy for fruits and vegetables. Lower subsidies of 10%–20% have been used in other recent healthy food research and modelling studies.12-14 The higher subsidy used in this program reflects the substantial challenges and barriers to healthy nutrition faced by disadvantaged Aboriginal and Torres Strait Islander families. However, it is consistent with the WIC program (Special Supplemental Food Program for Women, Infants, and Children) in the United States and the Healthy Start program in the United Kingdom, which provide free healthy foods to low-income pregnant women and young children. The WIC program, in particular, has been shown to improve the nutritional status of participating women and children and pregnancy outcomes.15-19 There are still questions about the cost-effectiveness of these healthy food subsidy programs and whether the impacts on nutritional status are sustained.15,20,21 Food subsidies remain topical in Australia, given increasing concerns about food insecurity22 and as a policy alternative to compulsory income management and cash entitlements for low-income families.
The before-and-after uncontrolled study design limits the strength of our data. Regression to the mean due to paired data and the normal reduction in rates of childhood illnesses in older children may have also contributed to the findings.23 Regression to the mean was accounted for through use of all-covariate adjusted models that included age, sex and community, in addition to the baseline value for each outcome analysed. It is also possible that other unrelated environmental factors contributed to the improvements in nutrition and health outcomes, such as local early childhood and school nutrition programs.24,25 In addition, the health record audits may be subject to incomplete ascertainment, due to the ability of patients to potentially access more than one primary health care service and the lack of linkage of hospital records across area health services. It is not possible to predict the impact of this on the findings; however, it is likely to have had a similar impact before and after participation.
We showed an association between subsidised fruits and vegetables and short-term health improvements in this study. We have previously reported increased plasma biomarkers of fruit and vegetable intake among participants,4 which supports the hypothesis that improvements in dietary intake contributed to improved health outcomes. A controlled study is needed for further confirmation of these findings and to allow investigation of the cost-effectiveness of such a program. Our findings are consistent with prospective studies demonstrating an association between healthy nutrition and improved long-term health outcomes.26,27
A larger trial is warranted to investigate the sustainability and feasibility of healthy food subsidy programs in Australia. The program could be adapted to target low-income families more generally. The design of future healthy food subsidy studies needs to allow us to distinguish between the relative contribution of fruit and vegetables and comprehensive primary health care to the improved outcomes. This program aimed to engage families in preventive health activities more fully than previously, which may also have contibuted to the observed health outcomes. This is relevant, given the cost of food subsidies and the need to target effective interventions. Food subsidy programs in the US operate independently of health services, although the WIC program assists participants to access health and social services.28
This fruit and vegetable subsidy program was associated with improvements in some indicators of short-term health status among disadvantaged Aboriginal children. These health outcomes and the associated improvements in biomarkers of fruit and vegetable intake4 have the potential to reduce health disparities in the population.
1 Baseline demographic characteristics of participating children, in total and by community
|
All communities |
Clarence |
Coffs Harbour |
Nambucca |
|||||||||||
No. of families |
55 |
30 |
12 |
13 |
|||||||||||
No. of children |
174 |
90 |
36 |
48 |
|||||||||||
No. of boys |
82 |
46 |
18 |
18 |
|||||||||||
Age in years, mean (SD) |
7.6 (4.2) |
7.5 (3.8) |
11.0 (3.3) |
5.8 (4.3) |
|||||||||||
Children with at least one smoker in household* |
107/164 |
62/90 |
18/36 |
27/38 |
|||||||||||
Families receiving unemployment benefits, pensions, no./total |
51/55 |
28/30 |
10/12 |
13/13 |
|||||||||||
* Proportion of participants with a valid response to the number of smokers in the household. |
|||||||||||||||
2 Retrospective clinical audit data for health outcomes among participants for the 12 months before and 12 months after starting the subsidised fruit and vegetable program (n = 167)*
 |
|
* Error bars show 95% CI. † Illness-related visits to health services. ‡ Preventive health-related visits to health services. § Number of prescriptions. |
3 Change in health outcomes among Aboriginal children participating in the subsidised fruit and vegetable program (n = 167)
|
Sick visits* |
Well visits† |
Otitis media episodes |
Pyoderma episodes |
Hospital attendances |
Oral antibiotics‡ |
Topical antibiotics‡ |
||||||||
Unadjusted mean Δ-score§ (95% CI) |
− 0.6 (− 1.1 to − 0.04)** |
− 0.1 (− 0.3 to 0.03) |
− 0.1 (− 0.2 to 0.06) |
− 0.2 (− 0.4 to 0.03) |
− 0.3 (− 0.5 to − 0.05) |
− 0.5 (− 0.8 to − 0.2)** |
− 0.06 (− 0.2 to 0.1) |
||||||||
Adjusted¶ mean Δ-score (95% CI) |
− 0.6 (− 1.2 to − 0.001)** |
− 0.2 (− 0.3 to − 0.01) |
− 0.1 (− 0.2 to 0.06) |
− 0.2 (− 0.4 to 0.05) |
− 0.2 (− 0.4 to 0.1) |
− 0.5 (− 0.8 to − 0.2)** |
− 0.1 (− 0.2 to 0.1) |
||||||||
* Illness-related visits to health services. † Preventive health-related visits to health services. ‡ Number of prescriptions. § (Number of episodes per year during 12 months’ participation) − (number of episodes in the year before program participation). ¶ Adjusted for sex, age and community. ** Significantly different to zero (P < 0.05). |
|||||||||||||||
4 Changes in haemoglobin and iron status among fruit and vegetable program participants (n = 129)
|
Mean level (SD) |
Δ-score (95% CI) |
Proportion classified as low |
||||||||||||
|
Before |
After |
Unadjusted mean |
Adjusted mean* |
Before (no. [%])† |
After (no. [%])† |
P |
||||||||
Haemoglobin (g/L)‡ |
126.8 (12.3) |
128.2 (10.5) |
1.5 (− 0.2 to 3.1) |
3.1 (1.4 to 4.8)** |
12/150 (8%) |
7/137 (5%) |
0.453 |
||||||||
Ferritin (μg/L)§ |
33.3 (24.2) |
35.2 (22.5) |
3.2 (− 0.5 to 6.2) |
1.7 (− 2.5 to 6.0) |
63/152 (41%) |
51/139 (37%) |
0.440 |
||||||||
Iron (μmol/L)¶ |
12.7 (6.0) |
13.2 (5.3) |
0.5 (− 0.6 to 1.6) |
0.8 (− 0.5 to 2.0) |
43/152 (28%) |
32/139 (23%) |
0.405 |
||||||||
* Adjusted for sex, age and community. † 129 participants had valid haemoglobin, ferritin and iron at baseline and follow-up. Additional participants had valid pathology at either baseline or follow-up as shown. ‡ Reference interval (RI): ≥ 5 years, 115–140 g/L; < 5 years, 105–140 g/L. § RI: boys, 20–200 μg/L; girls, 29–200 μg/L. ¶ RI, 11–28 μmol/L. ** Significantly different to zero (P < 0.05). |
|||||||||||||||
Received 8 April 2013, accepted 11 June 2013
- Andrew P Black1,2
- Hassan Vally3
- Peter S Morris4
- Mark Daniel1
- Adrian J Esterman1
- Fiona E Smith2
- Kerin O’Dea1
- 1 Division of Health Sciences, University of South Australia, Adelaide, SA.
- 2 Bulgarr Ngaru Medical Aboriginal Corporation, Grafton, NSW.
- 3 School of Public Health and Human Biosciences, La Trobe University, Melbourne, VIC.
- 4 Department of Paediatrics, Royal Darwin Hospital, Darwin, NT.
We acknowledge the families who participated in this evaluation study and the staff at the three health services, particularly David Ferguson and May Robinson from the Bulgarr fruit and vegetable committee, for the success of the study. Kerry Hampshire, Nicole Turner, Karen Spark, Lea Clayden, Marie Gough and Irina Holmes, Tracy Bradshaw and the team at Giingan Darrunday Marlaanggu Aboriginal Health Service contributed significantly to the clinical assessments. Thanks to Robyn Liddle for database design and Judy Boatswain for assistance with data entry. This study was supported by National Health and Medical Research Council, Australia (PhD scholarship 520681 and Program Grant 320860).
No relevant disclosures.
- 1. Marmot M, Friel S, Bell R, et al; Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008; 372: 1661-1669.
- 2. World Health Organization. Fruit and vegetables for health. Report of a joint FAO/WHO workshop, 1-3 September 2004, Kobe, Japan. Geneva: World Health Organization and Food and Agriculture Organization, 2005. http://www.who.int/entity/dietphysicalactivity/publications/fruit_vegetables_report.pdf (accessed Jun 2013).
- 3. Drewnowski A, Darmon N. Food choices and diet costs: an economic analysis. J Nutr 2005; 135: 900-904.
- 4. Black AP, Vally H, Morris P, et al. Nutritional impacts of a fruit and vegetable subsidy programme for disadvantaged Australian Aborigi-nal children. Br J Nutr 2013; Jun 7: 1-9. [Epub ahead of print.]
- 5. Calder PC, Jackson AA. Undernutrition, infection and immune function. Nutr Res Rev 2000; 13: 3-29.
- 6. Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 2007; 335: 194.
- 7. Gwynn JD, Flood VM, D’Este CA, et al. Poor food and nutrient intake among Indigenous and non-Indigenous rural Australian children. BMC Pediatr 2012; 12: 12.
- 8. Rowley KG, Su Q, Cincotta M, et al. Improvements in circulating cholesterol, antioxidants, and homocysteine after dietary intervention in an Australian Aboriginal community. Am J Clin Nutr 2001; 74: 442-448.
- 9. Lee AJ, Bailey AP, Yarmirr D, et al. Survival tucker: improved diet and health indicators in an aboriginal community. Aust J Public Health 1994; 18: 277-285.
- 10. Kanyini Vascular Collaboration [website]. Sydney: The George Institute for Global Health; 2012. http://www.kvc.org.au (accessed Jul 2012).
- 11. Lehmann D, Arumugaswamy A, Elsbury D, et al. The Kalgoorlie Otitis Media Research Project: rationale, methods, population characteristics and ethical considerations. Paediatr Perinat Epidemiol 2008; 22: 60-71.
- 12. Ni Mhurchu C, Blakely T, Jiang Y, et al. Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. Am J Clin Nutr 2010; 91: 736-747.
- 13. Ball K, McNaughton SA, Mhurchu CN, et al. Supermarket Healthy Eating for Life (SHELf): protocol of a randomised controlled trial promoting healthy food and beverage consumption through price reduction and skill-building strategies. BMC Public Health 2011; 11: 715.
- 14. Vos T, Carter R, Barendregt J, et al; ACE-Prevention Team. Assessing cost-effectiveness in prevention (ACE–Prevention): final report. Brisbane and Melbourne: University of Queensland and Deakin University, 2010. http://www.lowitja.org.au/assessing-cost-effectiveness-prevention-ace%E2%80% 93prevention-final-report (accessed Jun 2013).
- 15. Rush D, Leighton J, Sloan NL, et al. The National WIC Evaluation: evaluation of the Special Supplemental Food Program for Women, Infants, and Children. VI. Study of infants and children. Am J Clin Nutr 1988; 48 (2 Suppl): 484-511.
- 16. Rush D, Sloan NL, Leighton J, et al. The National WIC Evaluation: evaluation of the Special Supplemental Food Program for Women, Infants, and Children. V. Longitudinal study of pregnant women. Am J Clin Nutr 1988; 48 (2 Suppl): 439-483.
- 17. Rush D, Alvir JM, Kenny DA, et al. The National WIC Evaluation: evaluation of the Special Supplemental Food Program for Women, Infants, and Children. III. Historical study of pregnancy outcomes. Am J Clin Nutr 1988; 48 (2 Suppl): 412-428.
- 18. Metcoff J, Costiloe P, Crosby WM, et al. Effect of food supplementation (WIC) during pregnancy on birth weight. Am J Clin Nutr 1985; 41: 933-947.
- 19. Hoynes HW, Page ME, Stevens AH. Is a WIC start a better start? Evaluating WIC’s impact on infant health using program introduction. NBER Working Paper No.15589. Cambridge, MA: National Bureau of Economic Research, 2009. http://www.nber.org/papers/w15589 (accessed Jun 2013).
- 20. D’Souza L, Renfrew M, McCormick F, et al. Food-support programmes for low-income and socially disadvantaged childbearing women in developed countries. Systematic review of the evidence. London: National Institute for Health and Clinical Excellence, 2006. http://www.nice.org.uk/aboutnice/whoweare/aboutthehda/hdapublications/p105.jsp (accessed Jun 2013).
- 21. Joyce T, Racine A, Yunzal-Butler C. Reassessing the WIC effect: evidence from the Pregnancy Nutrition Surveillance System. J Policy Anal Manage 2008; 27: 277-303.
- 22. Foley W, Ward P, Carter P, et al. An ecological analysis of factors associated with food insecurity in South Australia, 2002-7. Public Health Nutr 2010; 13: 215-221.
- 23. Barnett AG, van der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol 2005; 34: 215-220.
- 24. Healthy Kids Eat Well, Get Active. Live Life Well @ School. Sydney: NSW Department of Health, NSW Department of Education and Communities and the Heart Foundation, 2012. http://www.healthykids.nsw.gov.au/campaigns-programs/live-life-well-@-school.aspx (accessed Jul 2012).
- 25. Healthy Kids Eat Well, Get Active. About Munch & Move. Sydney: NSW Department of Health, NSW Department of Education and Communities and the Heart Foundation, 2012. http://www. healthykids.nsw.gov.au/campaigns-programs/about-munch-move.aspx (accessed Jul 2012).
- 26. Ford ES, Zhao G, Tsai J, Li C. Low-risk lifestyle behaviors and all-cause mortality: findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health 2011; 101: 1922-1929.
- 27. Khaw KT, Wareham N, Bingham S, et al. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med 2008; 5: e12.
- 28. United States Department of Agriculture Food and Nutrition Service. How the WIC helps. 2004. http://www.fns.usda.gov/wic/aboutwic/howwichelps.htm (accessed Jun 2013).





Abstract
Objective: To evaluate the impact of a fruit and vegetable subsidy program on short-term health outcomes of disadvantaged Aboriginal children.
Design, setting and participants: A before-and-after study involving clinical assessments, health record audits and blood testing of all children aged 0–17 years (n = 167) from 55 participating families at baseline and after 12 months at three Aboriginal community-controlled health services in New South Wales. All assessments were completed between December 2008 and September 2010.
Intervention: A weekly box of subsidised fruit and vegetables linked to preventive health services and nutrition promotion at an Aboriginal Medical Service.
Main outcome measures: Change in episodes of illness, health service and emergency department attendances, antibiotic prescriptions and anthropometry.
Results: There was a significant decrease in oral antibiotics prescribed (− 0.5 prescriptions/year; 95% CI, − 0.8 to − 0.2) during 12 months of participation in the program compared with the 12 months before the program. The proportion of children classified as overweight or obese at baseline was 28.3% (38/134) and the proportion in each weight category did not change (P = 0.721) after 12 months. A small but significant increase in mean haemoglobin level (3.1 g/L; 95% CI, 1.4–4.8 g/L) was shown, although the proportion with iron deficiency (baseline, 41%; follow-up, 37%; P = 0.440) and anaemia (baseline, 8%; follow-up, 5%; P = 0.453) did not change significantly.
Conclusion: This fruit and vegetable subsidy program was associated with improvements in some indicators of short-term health status among disadvantaged Aboriginal children. A controlled trial is warranted to investigate the sustainability and feasibility of healthy food subsidy programs in Australia.