Snorkelling is a popular aquatic activity in Australia. In 2007, there were an estimated 2.2 million snorkelling dives conducted on the Great Barrier Reef alone.1 From the perspective of this exposure denominator, reports of harm from snorkelling are rare, and it can generally be considered a safe activity.
Nevertheless, a 1999 report on a 10-year survey of snorkelling-related deaths in Australia highlighted the need for increased vigilance on the part of snorkellers and those who care for them.2 Whereas both the absolute numbers and the rates of all reported drowning deaths have fallen over the past two decades,3 the absolute numbers of reported snorkelling-related deaths have increased.4,5 In 2006, 10 of 16 dive-related deaths involved snorkellers.5
In previous studies in Australia2 and New Zealand,6 most snorkelling-related deaths followed one of two typical scenarios. One scenario was that of a single, sober victim, often a tourist, snorkelling in a small group in relatively calm seas, who was later observed floating, apparently dead. The other involved a relatively young, typically male, spear fisherman who was snorkelling alone or had lost contact with his “buddy” and failed to surface. Some snorkellers died after post-hyperventilation breath-holding. (The practice of taking a series of deep breaths with greater than normal expirations before breath-holding can prolong apnoea by reducing the initial blood carbon dioxide levels, with very little associated increase in oxygenation. This, in turn, delays the stimulus to breathe beyond the point where the diver becomes unconscious from hypoxia.)
The Divers Alert Network (DAN) Asia–Pacific, based in Melbourne, provides support to injured divers throughout the Asia–Pacific region. It compiles and maintains a database with details of all diving-related deaths in the region.7 These include deaths resulting from snorkelling, scuba and surface-supplied diving activities.
Historical data were obtained through Project Stickybeak reports compiled by DAN Asia–Pacific between 1996 and 2002.8,9 More recent data (2003–2006) were compiled from the DAN fatality database; information provided by divers, dive operators, police and workplace authorities; newspaper and internet reports; the annual national drowning reports;10 the National Coroners Information System;11 and additional coronial files (for closed cases) from all states and territories of Australia. We began with cases listed in the DAN database, then cross-referenced these with the other information sources.
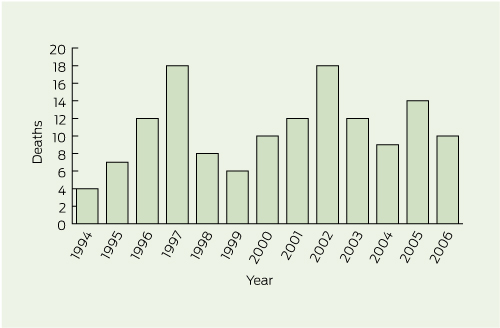
Over the 13-year period, we identified 140 snorkelling-related deaths — an average of about 11 per year. Annual frequencies of deaths from 1994 to 2006 are shown in Box 1. In 10 of the 140 cases, forensic pathology details were unavailable, either because the body was never found or there was no autopsy. Characteristics of the remaining 130 victims are summarised in Box 2.
The second-highest cause of death after cardiac disease was drowning.
The most common cause of death in snorkellers appears to be cardiac disease. People who die from this cause are typically sober, middle-aged or older males, enjoying the novel experience of supervised group snorkelling. Snorkelling involves potential cardiac stressors, including unaccustomed exertion, the anxiety of a novel experience, autonomic cardiogenic reflexes as part of the diving reflex,12 the effects of cold,13 and pulmonary and cardiac reflexes triggered by inhalation of, or immersion in, water. It is our experience that most novice snorkellers remain on the surface with their masked face immersed and avoid diving. However, most cardiac stresses apply whether a snorkeller is submerged or not.
Sudden unexpected deaths in healthy young adults are sometimes found to be due to congenital conditions such as prolonged QT syndrome14 and to channelopathies.15 Several studies have indicated that 14%–20% of healthy young adults who die unexpectedly and have no abnormalities detected on autopsy possess genetic mutations causing channelopathies.16 The preventive message here is that, if there is a family history of such deaths, or if there is a personal history of unexplained seizures, it is advisable to consult a medical practitioner before diving in any form. A further message from our research is that, in all such cases of sudden and unexplained death in which no cause is identified at autopsy, the family doctor should consider initiating genetic studies involving first- and second-degree relatives.17
With respect to snorkelling-related deaths in people with no history of cardiac or other medical conditions and no vascular or cardiac pathology at autopsy, we believe that a proportion of such deaths are consistent with dysrhythmias triggered by the diving reflex or tracheal-cardiac vagal reflexes after the inadvertent inhalation of small amounts of sea water. Such dysrhythmias have been known to trigger fatal cardiac-related outcomes in people with pre-existing cardiac disease. Immersion bradycardia (part of the diving reflex) may progress to various types of dysrhythmia, specifically P wave abnormalities and abnormal nodal rhythms.18 We posit that this process may lead to fatal dysrhythmias not only in people who are predisposed by existing coronary disease (eg, coronary artery disease or acute or chronic myopathies), electrical conduction defects or channelopathies, but also in otherwise normal people. Unaccustomed exercise, especially if vigorous, in people in an “at-risk” demographic group for coronary artery disease is a potential trigger for sudden cardiac death, whether due to dysrhythmias or infarction.
Given the enormous denominator of exposure experience in our Australia-wide survey over a 13-year period, we do not wish to overstate the small risk of cardiogenic death while snorkelling, but rather to highlight the increased relative risk of death if pre-existing cardiac disease is known to be present. Some large tourist boats in Queensland carry automated external defibrillators. However, the availability of a defibrillator does not guarantee survival, partly because of the delays in the recognition of a problem and the retrieval of the victim.5 Intending snorkellers with pre-existing cardiac disease or other serious conditions with potential cardiac comorbidity should have a prior medical consultation and be prudent in their physical exertion.
However, at least a quarter of the drowning deaths occurred in highly experienced snorkellers. Such deaths often followed hyperventilation before extended breath-holding, with subsequent hypoxic blackout before or immediately after surfacing. Many studies have described these preventable tragedies,2,4,5 in which a misguided diver “blows off” carbon dioxide by hyperventilation. There is then a risk that the normal hypercapnoeic “break point” may occur after the point where hypoxia produces unconsciousness in the submerged diver. If inspiration then occurs while the diver is still submerged, cardiopulmonary reflexes come into play. Hypoxic blackout can also occur without hyperventilation on extended breath-hold dives, especially those involving sustained exercise and ascent.19
Four of the surface drowning deaths occurred in snorkellers with a history of epilepsy. Snorkellers who suffer epileptic seizures are at risk of drowning. Water itself can trigger convulsive seizures, a phenomenon known as “bathing epilepsy”.20 There are two syndromes related to bathing epilepsy: (a) “water immersion epilepsy”, as defined by the International League Against Epilepsy,20 and (b) “hot water epilepsy”. Both syndromes have genetic implications. “Hot water epilepsy” has a particularly strong genetic basis, with recent provisional localisation of the gene concerned (4q24–q28).21 Hyperventilation before swimming underwater may also lead to anoxic seizures after a short (40–90 seconds) and apparently successful underwater swim.22 (The seizures described in this report were anoxic convulsions following hyperventilation coupled with breath-holding.)
Another phenomenon leading to respiratory compromise is that of immersion pulmonary oedema.23 In this potentially fatal syndrome, usually triggered by extreme exertion in the water, pulmonary congestion leads to cough, dyspnoea and haemoptysis. This syndrome, involving surface swimmers, is often associated with extreme exertion, not only in cold but also in warmer waters. Pre-existing diseases such as asthma and diabetes also increase the risk of potentially fatal events during snorkelling and diving.6,24 Most drowning victims identified in our study were either snorkelling alone or had lost contact with a buddy.
Received 1 August 2011, accepted 11 March 2012
- John M Lippmann1,2
- John H Pearn3
- 1 Divers Alert Network Asia–Pacific, Melbourne, VIC.
- 2 James Cook University, Townsville, QLD.
- 3 Department of Paediatrics and Child Health, Royal Children’s Hospital, Brisbane, QLD.
- 4 Royal Life Saving Society Australia, Sydney, NSW.
We acknowledge the assistance of the National Coroners Information System and are grateful for access to coronial data from the coroners’ offices of the states and territories. We also acknowledge DAN Asia–Pacific for funding this continued research.
No relevant disclosures.
- 1. Tourism Research Australia. Scuba diving and snorkelling report: visitor activities and characteristics, November 2007. Canberra: Commonwealth of Australia, 2007: 23, 52.
- 2. Edmonds CW, Walker DG. Snorkelling deaths in Australia, 1987–1996. Med J Aust 1999; 171: 591-594. <MJA full text>
- 3. Franklin RC, Scarr JP, Pearn JH. Reducing drowning deaths: the continued challenge of immersion fatalities in Australia. Med J Aust 2010; 192: 123-126. <MJA full text>
- 4. Walker D, Lippmann J, Lawrence C, et al. Provisional report on diving-related fatalities in Australian waters 2004. Diving Hyperb Med 2009; 39: 138-161.
- 5. Lippmann J, Walker D, Lawrence C, et al. Provisional report on diving-related fatalities in Australian waters 2006. Diving Hyperb Med 2011; 41: 70-84.
- 6. Davis M, Warner M, Ward B. Snorkelling and scuba diving deaths in New Zealand, 1980–2000. SPUMS J 2002; 32: 70-80.
- 7. Divers Alert Network Asia–Pacific. Diving related fatality database and cumulative register (incorporating data from Project Stickybeak). http://www.danasiapacific.org (data only available to authorised internal investigators.)
- 8. Walker D. Report on Australian diving deaths 1994–1998. Melbourne: Divers Alert Network Asia–Pacific, 2002.
- 9. Walker D. Report on Australian diving deaths 1999–2002. Melbourne: Divers Alert Network Asia–Pacific, 2009.
- 10. Royal Life Saving Society Australia. National Drowning Report [2005–2010]. Sydney: RLSSA, 2005–2010. http://www.royallifesaving.com.au/www/html/157-national-drowning-reports.asp (accessed Apr 2012).
- 11. National Coroners Information System. http://www.ncis.org.au.
- 12. Kooyman GL, Ponganis PJ. The physiological basis of diving to depth: birds and mammals. Annu Rev Physiol 1998; 60: 19-32.
- 13. Ferretti G, Costa M. Diversity in and adaption to breath-hold diving in humans. Comp Biochem Physiol A Mol Integr Physiol 2003; 136: 205-213.
- 14. Arnestad M, Crotti L, Rognum TO, et al. Prevalence of long-QT syndrome gene variants in sudden infant death syndrome. Circulation 2007; 115: 361-367.
- 15. de Caen AR, Kleinman ME, Chameides L, et al. Part 10: Paediatric basic and advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2010; 81 Suppl 1: e213-e259.
- 16. Chugh SS, Senashova O, Watts A, et al. Post-mortem molecular screening in unexplained sudden death. J Am Coll Cardiol 2004; 43: 1625-1629.
- 17. Behr ER, Delageorgou C, Christiansen M, et al. Sudden arrhythmic death syndrome: familial evaluation identifies inheritable heart disease in the majority of families. Eur Heart J 2008; 29: 1670-1680.
- 18. Ferrigno M, Grassi B, Ferretti G, et al. Electrocardiogram during deep breath-hold dives by elite divers. Undersea Biomed Res 1991; 18: 81-91.
- 19. Lindholm P, Gennser M. Aggravated hypoxia during breath-holds after prolonged exercise. Eur J Appl Physiol 2005; 93: 701-707.
- 20. Franzoni E, Gentile V, Grosso S, et al. Bathing epilepsy: report of two Caucasian cases. Epileptic Disord 2010; 12: 88-90.
- 21. Ratnapriya R, Satishchandra P, Dilip S, et al. Familial autosomal dominant reflex epilepsy triggered by hot waters maps to 4q24-q28. Hum Genet 2009; 126: 677-683.
- 22. Kumar KR, Ng K. Don’t hold your breath: anoxic convulsions from coupled hyperventilation — underwater breath-holding. Med J Aust 2010; 192: 663-664. <MJA full text>
- 23. Edmonds C. Scuba divers’ pulmonary oedema. A review. Diving Hyperb Med 2009; 39: 226-231.
- 24. Bennett MH, editor. The SPUMS recreational diving medical. Diving Hyperb Med 2010; 40: 150-155.





Abstract
Objective: To examine the frequency and causes of snorkelling-related deaths in Australia.
Design, setting and subjects: We conducted a retrospective analysis of snorkelling-related deaths recorded in Australia from 1994 to 2006 inclusive, based on information from the Divers Alert Network Asia–Pacific database, the National Coroners Information System, coronial files from all states and territories, and annual national drowning reports.
Main outcome measures: Number and attributed causes of snorkelling-related deaths.
Results: We identified 140 snorkelling-related deaths. Forensic details were available for 130 of these. Four principal cause-of-death categories were identified: deaths from cardiac or suspected cardiac causes (60), deaths from surface drowning (largely in inexperienced snorkellers) (33), deaths from drowning after prolonged breath-hold diving (largely in experienced divers) (19), and deaths from trauma (10). Eight people died of other causes.
Conclusions: In the context of the large population sampled, snorkelling-related deaths are rare. Preventive measures for such deaths could include pre-dive medical assessments for people with a history of cardiac or respiratory disease or with a family history of sudden unexpected death; improved training in how to use snorkelling equipment; better matching of skills to health, fitness and water conditions; better supervision and quality training of supervisors in rescue and resuscitation techniques; and avoidance of hyperventilation before breath-hold diving.