Supporters of Better Outcomes have criticised Better Access since its inception. Criticisms include that Better Access is used more often by relatively advantaged patients from major cities;1 and, since GPs no longer have to review the plans, “GPs have allowed their role in Better Access to dwindle to that of glorified referrers”.2
Several evaluations of Better Access have been published over the past year.3,4 Critics have called for the use of Bettering the Evaluation and Care of Health (BEACH) data to assist the evaluation process.5 In this article, we test the above two contentions in GP management of depression, as depression is the most frequently managed psychological problem in general practice.6
We analysed data from the BEACH program (detailed methods are described elsewhere).7 In summary, each year about 1000 GPs from a national, rolling random sample (drawn by the Department of Health and Ageing) participate by providing patient and encounter information for 100 consecutive encounters with consenting, unidentified patients.
We weighted each April to March year in the dataset (about 100 000 encounters) to match the age–sex distribution of all GPs in the sample frame and for each GP’s activity level (measured by number of MBS GP items claimed). The annual weighted BEACH encounter samples have repeatedly been shown to be representative of GP service items claimed through Medicare.7
We defined January 2002 to October 2006 as the Better Outcomes period and November 2006 to December 2011 as the Better Access period. Applying the Socio-Economic Indexes for Areas8 to patients’ residential postcodes, we defined Groups 6–10 as advantaged and Groups 1–5 as disadvantaged. Major city was defined according to the Australian Standard Geographical Classification.9 Depression was defined as problems classified as “P76 – Depressive disorder” in the International Classification of Primary Care (Version 2).10
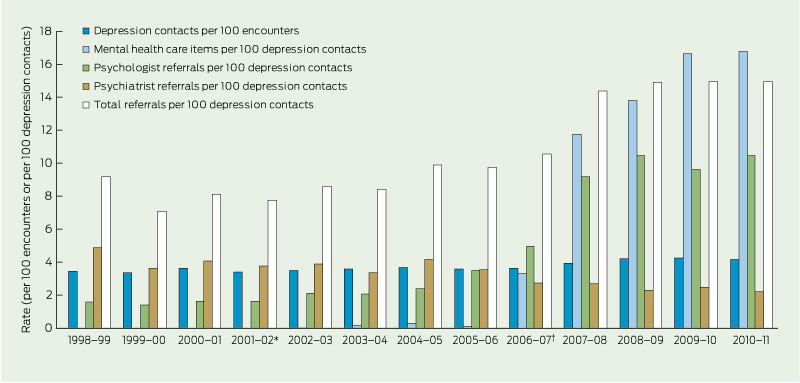
The overall rates of depression management, items claimed for depression and referrals for depression are shown in Box 1. Rates of depression management increased significantly during the study period, with the sharpest increase between 2006–07 and 2008–09. Between 2002–03 and 2005–06 (Better Outcomes), GPs used about one mental health care item number per 500 depression contacts. Between 2007–08 and 2010–11 (Better Access), this changed to a mental health care item being claimed for about one in six depression contacts.
A comparison of depression management during the two initiatives by patient location and socioeconomic group is shown in Box 2. During Better Outcomes, the highest depression management rate was for advantaged patients from non-major city areas. The rate of depression management increased significantly during Better Access for advantaged patients from major cities (16.0% increase) and for disadvantaged patients from non-major city areas (21.5% increase).
This study shows that, since the inception of Better Access, there has been a surge in referrals to psychologists for the management of depression. However, it also shows that GPs remained as active in the management of depression over the Better Access period as they were during Better Outcomes — GPs managed depression at a significantly higher rates, prescribed medication at similar rates, and provided counselling at slightly lower rates. We found no evidence from the BEACH data that the role of GPs has been reduced to that of “glorified referrers”.2
1 Rates of depression management, items claimed for depression and referrals for depression, April 1998 to March 2011
2 Comparison of rates of depression management by patient location and socioeconomic group during the Better Outcomes (January 2002 – October 2006) and Better Access (November 2006 – December 2011) initiatives
Received 28 March 2012, accepted 31 May 2012
- Christopher M Harrison1
- Helena C Britt2
- Janice Charles3
- Family Medicine Research Centre, School of Public Health, University of Sydney, Sydney, NSW.
We thank the GP participants in BEACH and all members of the BEACH team. During the data collection years reported here, the BEACH program was funded in all or some years by the Australian Government Department of Health and Ageing, the Australian Government Department of Veterans’ Affairs, the Australian Institute of Health and Welfare, the National Prescribing Service, AstraZeneca, Roche, Janssen-Cilag, Merck Sharp and Dohme, Pfizer, Sanofi-Aventis, Abbott, Wyeth, CSL Limited, GlaxoSmithKline, and the Office of the Australian Safety and Compensation Council (Australian Government Department of Employment and Workplace Relations).
No relevant disclosures.
- 1. Crosbie D, Rosenberg S; COAG Mental Health Reform. Mental Health and the new Medicare Services: 2nd report November 2006 – August 2008. Canberra: Mental Health Council of Australia, 2008. http://www.mhca.org.au/index.php/component/rsfiles/download? path=Mental%20Health%20Services/COAG%2 0MBS%202nd%20Report%20Sept%202008.pdf&Itemid=539 (accessed Jun 2012).
- 2. Rosenberg S, Hickie IB. Were the budgetary reforms to the Better Access to Mental Health Care initiative appropriate? No. Med J Aust 2011; 194: 595. <MJA full text>
- 3. Pirkis J, Ftanou M, Williamson M, et al. Australia’s Better Access initiative: an evaluation. Aust N Z J Psychiatry 2011; 45: 726-739.
- 4. Jorm AF. Australia’s Better Access initiative: do the evaluation data support the critics? Aust N Z J Psychiatry 2011; 45: 700-704.
- 5. Rosenberg S, Hickie I. How to tackle a giant: creating a genuine evaluation of the Better Access Program. Australas Psychiatry 2010; 18: 496-502.
- 6. Harrison CM, Britt H. The rates and management of psychological problems in Australian general practice. Aust N Z J Psychiatry 2004; 38: 781-788.
- 7. Britt H, Miller GC, Charles J, et al. General practice activity in Australia 2010–11. General practice series no. 29. Sydney: Sydney University Press, 2011. http://purl.library.usyd.edu.au/sup/9781920899868 (accessed Jun 2012).
- 8. Australian Bureau of Statistics. An introduction to Socio-Economic Indexes for Areas (SEIFA). Canberra: ABS, 2006. (ABS Cat. No. 2039.0.) http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/D729075E079F9FDECA2574170011B088/$File/20390_2006.pdf (accessed Feb 2009).
- 9. Australian Bureau of Statistics. Australian standard geographical classification. Canberra: ABS, 2008. (ABS Cat. No. 1216.0.) http://www. abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/1216.0Jul%202008?OpenDocument (accessed Dec 2008).
- 10. Classification Committee of the World Organization of Family Doctors. International Classification of Primary Care. 2nd ed. Oxford: Oxford University Press, 1998.





Abstract
Objective: To compare the Better Access to Psychiatrists, Psychologists and General Practitioners through the MBS initiative with the Better Outcomes in Mental Health Care initiative, to test contentions that Better Access is used more often by advantaged major city patients and that the role of GPs has been reduced to that of referrers.
Design and setting: Analysis of Bettering the Evaluation and Care of Health data relating to management of depression from April 1998 to March 2011, with the Better Outcomes period defined as January 2002 to October 2006 and the Better Access period defined as November 2006 to December 2011.
Main outcome measures: Rates of depression management by GPs, including rates of mental health care item claims, referrals, prescribing and counselling, by patient location and socioeconomic group.
Results: During the study period, rates of depression management increased and rates of referrals to psychiatrists halved. Compared with Better Outcomes, Better Access resulted in: increased depression management for advantaged major city and disadvantaged non-major city patients (16.0% and 21.5% increases, respectively); a small decrease in prescribing for advantaged major city patients; decreases in GP counselling; increases in referrals to psychologists for all patient groups (three- to fourfold increases), with advantaged major city patients referred more often than patients in other groups; and increases in mental health care item claims for all patient groups (44–65-fold increases), with more claims for advantaged major city patients than both non-major city patient groups.
Conclusion: Far from becoming “glorified referrers”, GPs remain heavily involved in the management of depression. Better Access brought about an enormous increase in access to primary care management of depression, although advantaged major city patients gained most. Any changes to the system must not compromise the strong improvements in access that have occurred for all groups.