Back pain is one of the most common reasons for medical consultation.1 It is the third most common reason for presentation to Australian general practice.2 Men and women are equally affected, mostly between the ages of 30 and 50 years. It is the most costly cause of work-related disability.3 With a point prevalence of 25% and with half the people with back pain likely to seek care, the economic burden is considerable, estimated at $1 billion in direct costs and a further $8 billion in indirect costs in 2001.4
Back pain is typically a recurrent condition. Although the prognosis for patients with an acute episode is favourable, with many recovering within 6–12 weeks, at least a third of such patients go on to have a recurrent episode within 1 year of the initial episode.5 Recurrent episodes contribute to much of the burden of back pain.
The major causes of back pain are shown in Box 1. The most common cause (> 85% of patients) is presumed musculo-ligamentous injury or “strain”, for which there is no clear pathophysiological basis and no identifying features on currently available clinical tests. It is most usefully classified as non-specific or idiopathic.3,4 Less common causes include radiculopathy (eg, disc herniation or spinal stenosis), referred visceral pain (eg, penetrating peptic ulcer), and other serious spinal conditions (eg, vertebral fracture, malignancy or osteomyelitis).
As non-specific back pain commonly resolves spontaneously, and given that serious aetiologies are rare, undertaking extensive investigations routinely is wasteful and potentially counterproductive. Conversely, history taking and examination should be done carefully to disclose any red flags (Box 2), which raise the potential of more serious underlying causes and demand a more intensive approach.1 In broad terms, these red flags relate to four diagnostic groups: serious neurological illness (eg, myelopathy, cauda equina syndrome), systemic illnesses (eg, malignancy, infection), vertebral fractures, and abnormal illness behaviour (eg, somatisation, psychogenic pain, malingering) (Box 2).
Information should be obtained about precipitating, exacerbating and relieving factors, and the location and radiation of the pain. Although pain may be described in mechanical or neuropathic terms, such terminology does not necessarily predict the underlying pathological process or the response to treatment. However, as illustrated in Hilary’s case, radiation of pain below the knee (“sciatica”), especially with accompanying numbness or paraesthesia, strongly suggests irritation of a lumbosacral nerve root. In these patients, leg pain that is exacerbated by twisting the back, sneezing or a Valsalva manoeuvre implicates herniation of a disc (Box 3), whereas exertional pain in the calf which is eased by forward flexion (eg, walking uphill or pushing a shopping trolley) may suggest spinal canal stenosis. If none of these classic histories is obtained, other potential causes of lumbosacral radiculopathy, plexopathy or sciatic neuropathy should be considered.
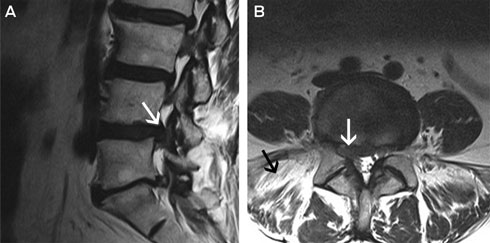
It is important to attempt to localise the neuroanatomical cause of the clinical signs, as multilevel disc herniations are common in older adults and it can be unclear radiologically which level is primarily responsible for a patient’s symptoms. Clinical and radiological correlation can confirm an L4/L5 disc protrusion — most commonly in the posterolateral direction, which can compress the L5 nerve root in the lateral recess of the spinal canal (Box 3), and less commonly in the far lateral direction, which can compress the descending L4 nerve root.
Sciatic stretch test: This test is commonly called the “straight-leg raising test” or Lasègue sign, and is performed with the patient in the supine position with the pelvis stabilised; the result is positive if calf pain is elicited when the leg is raised to less than 70 degrees (although lower limits are used in some studies).7 Straight-leg raising is a highly sensitive test for L5/S1 radiculopathies (positive in 90% of cases),7 but it is non-specific and may be positive in many other conditions (eg, hip osteoarthritis, trochanteric bursitis). Conversely, the “crossed straight-leg raising test” (where straight leg raising induces contralateral pain) is insensitive (positive in about 30% of cases) but highly specific for radiculopathy (about 90%).7
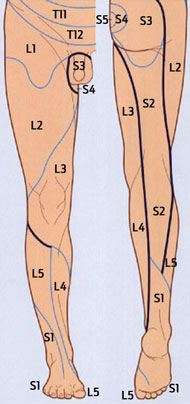
Trying to localise the site of a radiculopathy based on the motor signs is challenging, as most muscles are innervated by more than one nerve root and this varies between individuals. The overall pattern of weakness is more critical than the function of any single muscle being tested (Box 4). Consideration should be given to the pretest probability of finding an abnormality and the knowledge that 95% of all symptomatic disc herniations affect the L5 and S1 roots. Sensory symptoms are usually quite accurate in terms of localising the lesion, but sensory deficits may be ill defined or absent due to overlap of dermatomes (Box 4).
Hilary’s hip weakness ruled out both common peroneal and sciatic neuropathies, and there were no upper motor neurone features or crossed sensory disturbance to suggest a pathological process involving the cerebrum or spinal cord. Her prominent sensory symptoms and lack of upper motor neurone features exclude motor neurone disease.
Urgent neuroimaging is indicated in situations where important neurological symptoms or signs are present in a patient with low back pain. This includes patients with extensive deficits, which are usually due to compression of multiple nerve roots in the cauda equina, and produce symptoms of peri-anal (“saddle”) sensory loss, bowel and urogenital dysfunction and variable leg numbness and weakness.9 Prolapse of a lower lumbar central disc is the commonest cause of such a disturbance, but malignancy must be excluded. Although computed tomography (CT) is widely available and provides good delineation of bony architecture, magnetic resonance imaging (MRI) is the modality of choice as it provides greater contrast between soft tissue structures and does not use ionising radiation. In Australia, this is best facilitated by urgent referral to a specialist (neurologist, neurosurgeon or spinal surgeon).
Expert opinion is unanimous in recommending that imaging not be performed in the absence of red flags (Box 2).1,3,10 As well as the high cost, routine early imaging has not been shown to improve a patient’s level of pain, function or satisfaction, in the short or long term (Grade A evidence).11 As disc herniations are commonly found in asymptomatic individuals, the demonstration of possibly incidental abnormalities may reinforce or prompt abnormal illness behaviour. In cases of mild radicular features and a low suspicion of malignancy or infection, a trial of conservative therapy is recommended before undertaking neuroimaging (usually a CT scan before referral to a specialist), since many patients’ symptoms will resolve spontaneously over several weeks. Neuroimaging is required if surgery is being considered for the treatment of persistent symptoms or neurological deficits.
Hilary’s symptoms did not resolve with conservative management and she was referred to a neurosurgeon. MRI of her lumbar spine was performed, which showed broad-based posterolateral L4/L5 disc herniation with compression of the right L5 nerve root (Box 5). The scan also showed fatty replacement of the right paraspinal muscles, suggesting denervation atrophy and indicating chronicity. This also excluded a plexopathy (Box 5) and indicated that no further investigation was necessary.
In cases of acute-onset back pain and radicular symptoms, it is important to educate the patient. Non-interventional treatment is usually indicated as more than three-quarters of patients recover spontaneously within several weeks (Grade B evidence).12 Despite widespread use, there is inconsistent evidence supporting treatment of sciatica with non-steroidal anti-inflammatory drugs (NSAIDs), traction, physiotherapy or immunosuppressive agents (Grade B evidence). As bed rest does not appear to hasten recovery or improve symptoms,13 patients should generally be encouraged to mobilise. Although there is a paucity of data guiding the choice of specific analgesic medication (Grade C evidence),12 it seems reasonable to extrapolate from back pain guidelines14 and to commence with paracetamol (1 g four times a day) before escalating to an NSAID, then opioid analgesia (slow-release formulations of oxycodone are generally used), and (if pain lasts more than 3–4 weeks) a tricyclic antidepressant (Grade B evidence). The speed of escalation in this treatment algorithm should be determined by the degree of patient discomfort. As a general rule, conservative treatments should be encouraged for several weeks.
The approach to interventional treatment is highly individualised. It depends greatly on the response to conservative measures, the presence of radicular signs, and patient preferences. Some evidence indicates that transforaminal corticosteroid injection improves short- but not long-term outcomes,15 but this is a controversial treatment (Grade B evidence)12 that is best reserved for patients wishing to delay or avoid surgery (and should therefore be ordered by specialists). Although there is good evidence that early surgery (6–12 weeks) hastens recovery (Grade A evidence), it may not improve long-term (> 1 year) outcomes.12 Various surgical approaches are available (open discectomy, micro discectomy and micro-endoscopic discectomy and transforaminal discectomy), but as none has proven superiority, patient preferences play a role in choosing between them (Grade B evidence). Fusion procedures should rarely be performed. Structured rehabilitation hastens recovery after surgery (Grade B evidence).16
Treatment options (Box 6) were discussed with Hilary and she was encouraged to remain active. A stepwise approach to analgesia was suggested (paracetamol, then NSAIDs, then codeine plus paracetamol, and nocturnal amitriptyline). After 5 weeks, a reasonable balance of analgesia and side effects was obtained with moderate doses of oxycodone (5–10 mg four times a day). A transforaminal steroid injection is planned, with subsequent elective micro discectomy if the steroid injection is not effective.
1 Major causes of back pain and proportions of patients affected1,3
Disc herniation and compressive or irritative radiculopathy
Spinal stenosis
Osteophytic nerve root compression
Neoplastic nerve root compression or infiltration
Inflammatory radiculopathy
Failed back surgery syndrome
Infection (eg, herpes zoster)
Referred visceral pain (1%–2%)
Aortic aneurysm
Gastrointestinal disease (eg, penetrating ulcer)
Pelvic disease (eg, prostatitis)
Renal disease (eg, pyelonephritis)
2 Red flags that should raise index of suspicion of a serious underlying condition1,3
Leg weakness
Saddle anaesthesia
Sphincteric disturbance
Gait disturbance
Hyporeflexia
Decreased anal tone
Babinski sign
3 Herniated disc
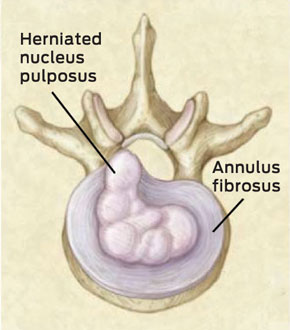
Figure reproduced with permission from the Massachusetts Medical Society, copyright 2001.3
4 Patterns of clinical signs associated with specific nerve root lesions6,8
Hip abduction and internal rotation; knee extension; foot dorsiflexion and inversion |
|||||||||||||||
Ankle and toe plantar flexion; toe dorsiflexion; ankle eversion; knee flexion; hip extension |
|||||||||||||||
Figure (dermatome diagram only) reproduced with permission from Elsevier, copyright 2010.6
6 Treatment options for radiculopathy
Advice (nature of condition, simple safe treatments for pain, graded activity resumption, avoidance of bed rest)
Graded analgesia (paracetamol, non-steroidal anti-inflammatory drug, opioid, tricyclic antidepressant) (Grade B evidence)14
Transforaminal corticosteroid injection (Grade B evidence)12,15
Surgery if symptoms do not resolve (Grade A evidence)12
- Timothy J Kleinig1
- Brian P Brophy1
- Chris G Maher2
- 1 Royal Adelaide Hospital, Adelaide, SA.
- 2 The George Institute for Global Health, University of Sydney, Sydney, NSW.
No relevant disclosures.
- 1. Cohen SP, Argoff CE, Carragee EJ. Management of low back pain. BMJ 2008; 337: a2718.
- 2. Australian Institute of Health and Welfare. Australia’s health 2010. Canberra: AIHW, 2010. (AIHW Cat. No. AUS 122; Australia’s Health Series No. 12.)
- 3. Deyo RA, Weinstein JN. Low back pain. N Engl J Med 2001; 344: 363-370.
- 4. Walker BF, Muller R, Grant WD. Low back pain in Australian adults: the economic burden. Asia Pac J Public Health 2003; 15: 79-87.
- 5. Stanton TR, Henschke N, Maher CG, et al. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine 2008; 33: 2923-2928.
- 6. O’Brien MD, for the guarantors of Brain. Aids to the examination of the peripheral nervous system. 5th ed. London: Elsevier, 2010.
- 7. van der Windt DA, Simons E, Riphagen II, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev 2010; (2): CD007431.
- 8. Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin 2007; 25: 387-405.
- 9. Lavy C, James A, Wilson-MacDonald J, Fairbank J. Cauda equina syndrome. BMJ 2009; 338: b936.
- 10. Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J 2010; 10: 514-529.
- 11. Chou R, Fu R, Carrino JA, Deyo RA. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet 2009; 373: 463-472.
- 12. van Tulder M, Peul W, Koes B. Sciatica: what the rheumatologist needs to know. Nat Rev Rheumatol 2010; 6: 139-145.
- 13. Vroomen PC, de Krom MC, Wilmink JT, et al. Lack of effectiveness of bed rest for sciatica. N Engl J Med 1999; 340: 418-423.
- 14. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 147: 478-491.
- 15. Chou R, Atlas SJ, Stanos SP, Rosenquist RW. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976) 2009; 34: 1078-1093.
- 16. Ostelo RW, Costa LO, Maher CG, et al. Rehabilitation after lumbar disc surgery: an update Cochrane review. Spine (Phila Pa 1976) 2009; 34: 1839-1848.





Abstract
Back pain is very common; it has a point prevalence of 25% and is the third most common reason for consultation in Australian general practice.
A thorough history and examination can identify the minority of patients who require urgent neuroimaging or other targeted investigations.
Careful correlation of clinical and radiological findings is required when abnormal neurological findings are detected. Radiological investigations may detect abnormalities at multiple levels but cannot confirm which level is primarily responsible for a patient’s symptoms.
A trial of conservative treatment is appropriate, even in cases of radiculopathy. Most patients with an acute episode of back pain recover within 6–12 weeks, but at least a third go on to have a recurrent episode within 1 year.
Various invasive treatments, such as transforaminal steroid injection and discectomy, may speed up recovery from radiculopathy, but the long-term benefits of invasive treatment are uncertain.