Pressure is mounting for reform in Australia’s mental health sector.1-4 Mental health research is recognised as playing a role in developing effective, innovative approaches to treatment, intervention and primary health care.
NHMRC funding data for 2001–2010 were obtained from the NHMRC research funding datasets.5
Ethics approval was not sought because data were retrieved in de-identified form from available databases. Funding as a function of disease burden was calculated using methods described elsewhere.6,7
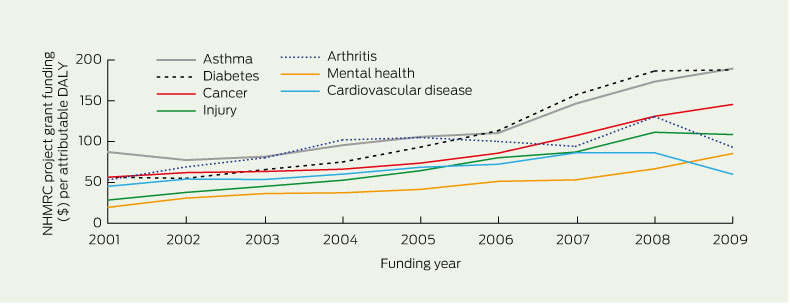
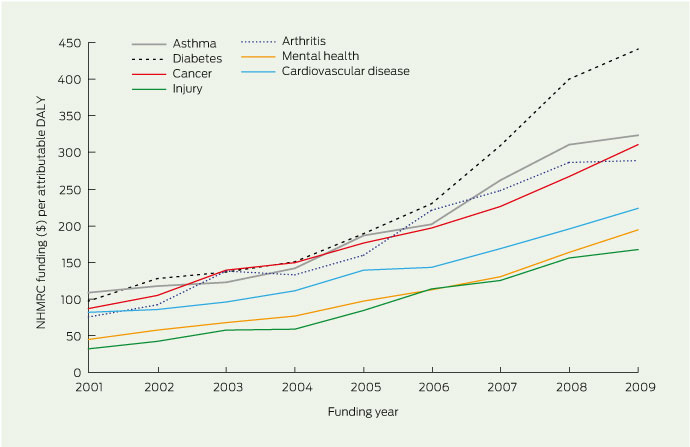
Mental health research receives lower levels of funding than cardiovascular disease and cancer research (about 9.5%, 21.7% and 14.9%, respectively, in 2009). However, when adjustments are made for burden of disease (Box 1), the areas of diabetes, asthma, cancer, arthritis and cardiovascular disease all receive proportionately more research dollars per attributable dis-ability-adjusted life-year (DALY)7 than does mental health. Relative to other conditions, diabetes had the largest increase in research funding from 2001 to 2009 (see Box 2 for data on project grants).
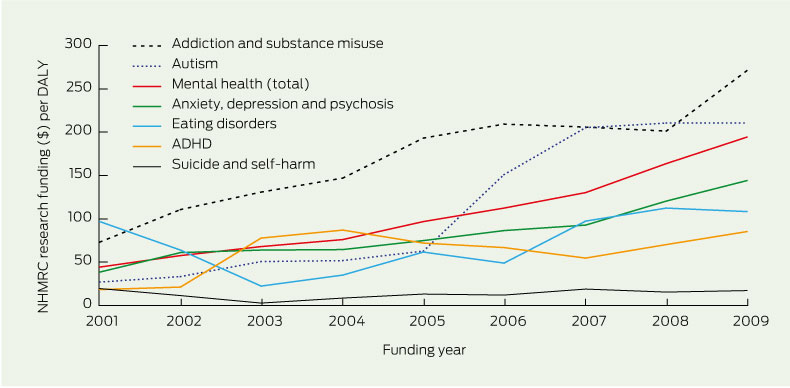
Box 3 outlines the funding awarded within mental health categories from 2001 to 2009, inclusive. Substance misuse and autism did proportionately better per DALY than eating disorders, attention deficit hyperactivity disorder, or anxiety, depression and schizophrenia. Although it is difficult to interpret trends, funding to suicide and eating disorders research does not appear to have increased over the past 10 years, despite the nearly threefold increase in medical research funding overall. Up to 6% of mental health funding consisted of grants for research into ageing in any one year.
Box 4 shows how Australian scientific research has performed in terms of quantity (number of articles) and quality (citations), compared with the rest of the world. The data on papers and citations come from the ISI Essential Science Indicators website (http://wokinfo.com/products_tools/analytical/essentialscience indicators/).
Based on our analysis, it is clear that mental health research does not receive the same level of funding support as other research areas such as cancer and diabetes, a conclusion already reached by Mitchell and colleagues.6 In the United States, 13%–15% of National Institutes of Health funding goes to mental health and drug and alcohol research, and research into ageing, a percentage that has been stable since 2001.8 Even if funding for research into ageing is excluded from the US figures, 10%–11% of US funding goes to the areas covered by the NHMRC mental health category. In short, two indicators (funds per DALY and international funding levels) indicate that mental health research funding is relatively low in Australia.
Our analysis shows little evidence that the criteria used to fund mental health research is biased for project grants. However, bias may be an issue with the “newer” NHMRC schemes (those introduced over the past 4–5 years), such as Australia Fellowships, Development Grants, Centres of Research Excellence, and Translating Research into Practice Fellowships. In 2010, 54 of these grants were offered, but mental health researchers were unsuccessful in every one of these schemes.9 This poor success rate could arise by chance; as a result of poor scientific quality; because of low application rates by mental health researchers; due to other unknown factors; or because of bias in ranking, given the evidence of high international success.
Our analysis suggests that the main barrier to mental health research funding is capacity. As noted by Mitchell and colleagues,6 the Wills report recommended that the NHMRC engage in building national workforce capacity.10 It also recommended that the NHMRC could specifically allocate personnel support funds to under-resourced areas to build up workforce capacity.6 Based on the data we have from 2009 and 2010, this recommendation has not resulted in any substantial change in workforce capacity in mental health research. In this respect, it is pleasing to see that in the Australian Budget of May 2011, $26.2 million of NHMRC money was earmarked for special mental health research initiatives.11
In conclusion, there has been no “narrowing of the gap” over the past 10 years in the proportion of funding provided to mental health research. If we assume that NHPAs should be equally prioritised, the failure to narrow the gap indicates the need for action over the next decade.
2 Project funding adjusted for DALYs, 2001–2009
 | |||||||||||||||
|
DALY = disability-adjusted life-year. NHMRC = National Health and Medical Research Council. | |||||||||||||||
Received 2 December 2010, accepted 27 July 2011
- Helen Christensen1
- Philip J Batterham1
- Ian B Hickie2
- Patrick D McGorry3
- Philip B Mitchell4
- Jayashri Kulkarni5
- 1 Centre for Mental Health Research, Australian National University, Canberra, ACT.
- 2 Brain and Mind Research Institute, University of Sydney, Sydney, NSW.
- 3 Orygen Youth Health, University of Melbourne, Melbourne, VIC.
- 4 School of Psychiatry, University of New South Wales, Sydney, NSW.
- 5 Monash Alfred Psychiatry Research Centre, Monash University, Melbourne VIC.
We thank Saraid Billiards and Marcus Nicol, from the NHMRC, for making data available.
No relevant disclosures.
- 1. Department of Health and Ageing. Towards a national primary health care strategy. Canberra: DoHA , 2008. http://www.health.gov.au/internet/main/publishing.nsf/Content/D66FEE14F736A789CA2574E3001783C0/$File/DiscussionPaper.pdf (accessed Nov 2011).
- 2. Department of Health and Ageing. National Mental Health Report 2010. Canberra: DoHA , 2008. http://www.health.gov.au/internet/main/publishing.nsf/content/8C20A89EAC527C40CA 2577EE000F6E01/$File/rep10cov.pdf (accessed Nov 2011).
- 3. National Health and Hospitals Reform Commission. A healthier future for all Australians, final report June 2009. Canberra: NHHRC, 2009. http://www.health.gov.au/internet/nhhrc/publishing.nsf/Content/nhhrc-report (accessed Nov 2011).
- 4. Australian Medical Association. Mental health position statement. Canberra: AMA, 2011. http://ama.com.au/node/6524 (accessed Nov 2011).
- 5. National Health and Medical Research Council. NHMRC research funding dataset 2001–2010. Canberra: NHMRC, 2010. http://www.nhmrc.gov. au/grants/dataset/rmis/index.htm (accessed Nov 2011).
- 6. Mitchell RJ, McClure RJ, Olivier J, Watson W. Rational allocation of Australia’s research dollars: does the distribution of NHMRC funding by National Health Priority Area reflect actual disease burden? Med J Aust 2009; 191: 648-652. <MJA full text>
- 7. Australian Institute of Health and Welfare. The burden of disease and injury in Australia 2003. Canberra: AIHW, 2007. http://www.aihw.gov.au/publication-detail/?id=6442467990 (accessed Nov 2011).
- 8. National Institutes of Health Office of Budget. NIH history of congressional appropriations, fiscal years 2000–2010. http://officeofbudget.od.nih. gov/pdfs/FY11/Approp.%20History%20by% 20IC%20%28FINAL%29.pdf (accessed Nov 2011).
- 9. National Health and Medical Research Council. Outcomes of funding rounds. Canberra: NHMRC, 2011. http://www.nhmrc.gov.au/grants/rounds/index.htm (accessed Nov 2011).
- 10. Wills PJ. The virtuous cycle. Working together for health and medical research. Canberra: Commonwealth of Australia, 1998. http://www. health.gov.au/internet/main/publishing.nsf/Content/hmrsr.htm (accessed Nov 2011).
- 11. Australian Government. Budget 2011–12: delivering better hospitals, mental health and health services. Canberra: Commonwealth of Australia, 2011. http://budget.australia.gov.au/2011-12/content/download/glossy_health.pdf (accessed Nov 2011).





Abstract
Objectives: To examine the levels and growth rates of absolute funding to mental health research from 2001 to 2010, compared with other National Health Priority Areas (NHPAs), and the relative rate of mental health funding compared with other NHPAs, by taking disease burden into account. The quality of Australian research in mental health was also examined using objective indicators of research strength.
Design and setting: Retrospective analysis of levels of funding overall and as a function of mental health domains using data from the National Health and Medical Research Council, with and without adjustment for burden of disease. A keyword analysis was used to assess the success rate of mental health project grant applications. Objective indicators of the quality of Australian mental health research were sought from citation indicators.
Main outcome measures: Funding for mental health research relative to disease burden; funding according to disease category; project grant success rates.Results: Using actual and adjusted figures, mental health research received a lower proportion of health funding than other NHPAs, including cancer, diabetes and cardiovascular disease. Research projects into substance misuse and autism were proportionately better funded than those in anxiety, depression or schizophrenia. A significant proportion of mental health research funding was awarded to research into ageing. Citation data indicated that mental health research in Australia performed better than research in neuroscience, clinical medicine, microbiology, and pharmacology and toxicology, and at a comparable level to immunology research, despite poor levels of funding.
Conclusions: Low levels of funding for mental health research appear to be largely attributable to low capacity. Mental health research in Australia is of high quality, and efforts are needed to build capacity.